6 Femoral Neck Fractures
Reduction and Fixation
Defining the Injury
Fractures of the proximal femur are generally categorized as follows: (1) femoral head fractures, (2) femoral neck fractures, and (3) trochanteric fractures (including the subtrochanteric region). In their 1961 study of the proximal femur, Garden et al defined femoral neck fractures as subcapital fractures of the femur with fracture lines present between the femoral head and the trochanteric region.1 These investigators also highlighted the importance of differentiating between fractures lending themselves to stable reduction and fractures less amenable to stabilization.1,2 Based on the position and displacement of the fragments, Garden et al demonstrated that unstable fractures are more likely than stable fractures to damage the blood vessels of the femoral head and potentially cause avascular femoral head necrosis.
Classification
There are several comprehensive classification systems for femoral neck fractures and related prognostic factors such as femoral head necrosis, fracture nonunion, and fracture stability. The best-known classification systems are those of Garden (1964) and Pauwels (1935).3,4
Historical Background
Many investigators have devised classification schemes for femoral neck fractures that indicate prognostic differences according to fracture type. The first classification of femoral neck fractures was published in 1823 by Cooper, who divided these injuries into intracapsular and extracapsular fractures.5 Waldenström in 1924 and Cotton in 1927 classified these injuries as either abduction fractures and adduction fractures, according to their displacement features.6,7 In 1955, Watson-Jones developed a system based on the age of the patient. He concluded that certain fracture types were typical in certain age groups.8 Enduring and meaningful classification systems were finally developed by Pauwels in 1935, Linton in 1941, and Garden in 1961.3,4,9,10
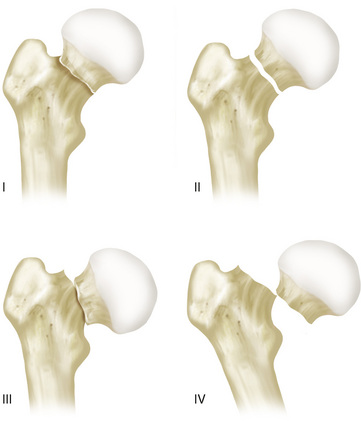
Classification System of Garden
In 1964, Garden et al created a classification system for femoral neck fractures that consisted of four fracture types (Garden I to Garden IV), depending on the position and displacement of the femoral head in the anteroposterior (AP) projection (Fig. 6-1). In this system, type I includes fractures with an incomplete fracture line through the femoral neck and valgus position of the proximal fragment, type II comprises fractures with a complete fracture line through the femoral neck and no displacement between the proximal and distal fragments, type III includes fractures with a complete fracture line through the femoral neck and varus displacement of the proximal fragment that is less than 50% of the femoral neck diameter, and type IV comprises fractures with varus displacement of more than 50% of the femoral neck diameter or complete dissociation of the proximal and distal fragments.
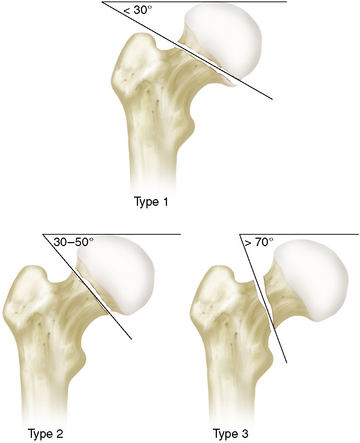
Classification System of Pauwels
In 1935, Pauwels published a classification system of femoral neck fractures that included three types (Pauwels I to Pauwels III). The fractures were divided according to the angle between the fracture line and the horizontal line in the AP radiographic projection (Fig. 6-2). In this system, type I fractures have an angle smaller than 30 degrees between the fracture line and the horizontal line, type II fractures have an angle between 30 and 70 degrees, and type III fractures have an angle larger than 70 degrees.
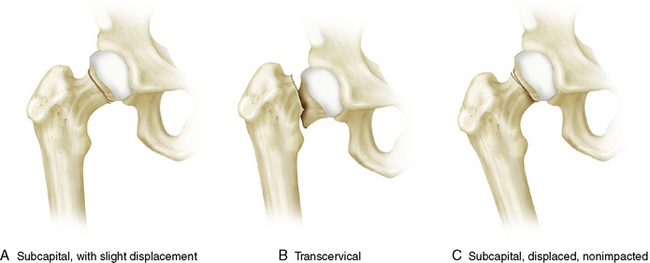
AO Classification
The AO (Arbeitsgemeinschaft für Osteosynthesefragen, Switzerland, 1958) developed a simplified classification for femoral neck fractures including three subtypes (31 B1 to 31 B3). This system is arranged in order of increasing severity of these injuries according to complexity of the fracture, difficulty in treatment, and prognosis. These fractures are finally categorized by fracture site (subcapital, transcervical), as well as by impaction and displacement of the femoral head. Subtype B1 describes subcapital fractures with impaction and slight displacement, subtype II fractures are transcervical, and the subtype III category includes subcapital and nonimpacted fractures with strong displacement (Fig. 6-3).
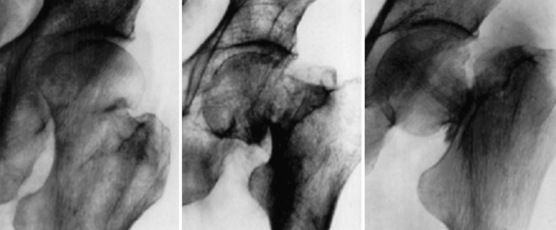
Classification System of Linton
In 1941, Linton presented his classification scheme, which included three different types of femoral neck fractures based on the angulations between the median femoral neck trabeculae and the femur’s medial cortical trabeculae. This angle is normally 160 degrees in the AP projection (Fig. 6-4). Linton also considered the displacement of the central axis of the femoral head to the central axis of the femoral neck in the axial view, which is usually in a straight line of 180 degrees. Fractures were finally divided into the following categories: (1) fractures in adduction, with varus displacement and an angle between the median femoral neck trabeculae and the femur’s medial cortical trabeculae much smaller than 160 degrees; (2) fractures in abduction, with valgus displacement and parallel median femoral neck and femoral medial cortical trabeculae; and (3) intermediate fractures, corresponding to displacement halfway between adduction and abduction.
Nonoperative Treatment
In some cases, nonsurgical treatment can also be an option in patients with undisplaced impacted valgus fractures classified as Garden type I or Pauwels type I. Impaction must be evident on both AP and true lateral radiographic views, and axial alignment of the femoral neck must also be intact. Nonoperative management begins with bed rest and exercises in bed until the pain subsides. Gradual mobilization begins with transfer to a chair, walking without weight bearing with crutches or other walking aids, and later walking with partial weight bearing. After 6 to 8 weeks, full weight bearing can be started. Radiographs should be taken regularly, especially at the beginning of mobilization, after partial weight bearing, and before full weight bearing. In literature, outcome after nonoperatively treated impacted fractures is still controversial. Raaymakers et al reported satisfactory results after conservative treatment, but they also reported a high rate of secondary fracture displacement, especially in elderly patients.11,12 These investigators found secondary instability in 41% of patients more than 70 years of age, but only in 7% of healthy patients less than 70 years of age. Shuqiang et al also found secondary displacement in 41% of their patients, and the highest displacement rate was at age 60 to 80 years.13 Bentley, Hilleboe et al, and Jensen and Hogh showed a fracture displacement or disimpaction rate of 10% to 27% with conservative treatment.14–16 Raaymakers et al also found a high correlation between comorbidity and secondary instability.11 Verheyen et al stated that the stability of the fracture depended on several intrinsic and extrinsic factors such as age, comorbidity, Pauwels angle, and retroversion.17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree