13 Subtrochanteric Fractures
Intramedullary Fixation
The first group comprises trochanteric fractures. In the literature, these fractures have been termed reversed intertrochanteric fractures, reverse obliquity fractures, reverse oblique and transverse intertrochanteric fractures, high subtrochanteric fractures, reversed Evans fractures, intertrochanteric-subtrochanteric fractures, and subtrochanteric fractures.1–9 In the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification,10 these fractures are termed intertrochanteric (Fig. 13–1). In addition, some investigators use the term intertrochanteric fractures for pertrochanteric fractures (31A1 and 31A2).11,12
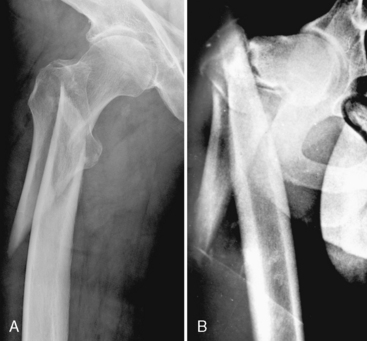
In the second group, the term subtrochanteric fracture is used by most investigators for fractures occurring between the lesser trochanter and the isthmus of the femoral shaft (i.e., approximately 5 cm distally from the lesser trochanter)13–15 (Fig. 13–2). Moreover, there is a continuum between these two groups. This situation has resulted in terminologic and morphologic confusion that may lead to discrepancies in the comparison of treatment type and outcome of these fractures.11,16–24
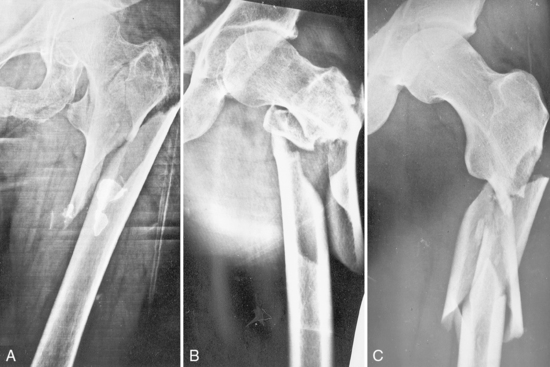
Figure 13-2 A to C, Fractures occurring between the lesser trochanter and the isthmus of the femoral shaft.
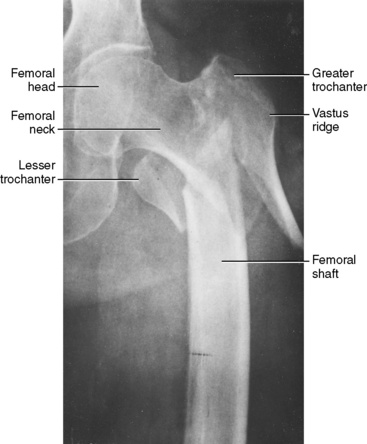
In both intertrochanteric and subtrochanteric fractures, the proximal fragment is formed by the femoral head, the femoral neck, and the greater trochanter, including its base with the vastus ridge (tuberculum vastoadductorium or innominate tubercle) (Fig. 13–3). The gluteus medius muscle (proximally) and the origin of the vastus lateralis muscle (distally) are attached on this tubercle. Tension in these muscles may cause displacement of the proximal fragment and complicate fracture reduction. This situation applies particularly to certain types of subtrochanteric fractures, in which a portion of the iliopsoas tendon is also attached to the medial cortex of the proximal fragment and pulls the fragment into flexion. The femoral shaft is the distal fragment, and another fragment can be formed as a result of avulsion of the lesser trochanter with the medial cortex. Secondary fracture lines may be present in the area of the greater trochanter or the femoral shaft. The subtrochanteric area of the proximal femur is composed mainly of cortical bone. This type of bone is less vascular and the fracture surface available for healing is smaller than in cancellous bone in pertrochanteric fractures.
In older patients, fractures result from low-energy trauma, as in a simple fall. Fractures from low-energy trauma usually have minimal comminution and are transverse, short oblique, or spiral (Fig. 13–4).
History
In the last 30 years, intramedullary nailing techniques underwent a process of rapid innovation, although the cornerstones of this process were set in 1940. For better understanding of the present state of intramedullary nailing, it is crucial to know when and how the individual construction principles were developed.25
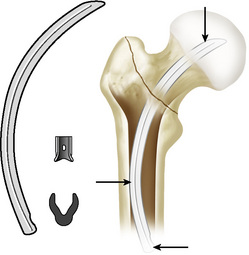
Küntscher Y-Nail, Detensor
The beginnings of intramedullary nailing of proximal femoral fractures are connected with the names of G. Küntscher and R. Maatz. In 1940, just after successfully introducing intramedullary nailing of femoral shaft fractures, Küntscher developed a conical nail for treatment of high subtrochanteric fractures. This nail was inserted from the apex of the greater trochanter. Shortly afterward, this advance was followed by the so-called Y-nail, a precursor to the reconstruction nails in present use (Fig. 13–5). From the apex of the greater trochanter, a U-shaped intramedullary nail 32 cm long was introduced into the medullary cavity of the femoral shaft. At a distance of 8 cm from proximal end, this nail had a hole for introducing a shorter (11.5-cm) transverse nail, with a double-T profile. This transverse nail was introduced into the femoral neck and head at an angle of 135 degrees with the help of a targeting device attached to the diaphyseal nail.26 The instruments Küntscher used were very advanced for the time. Küntscher later reported that he had successfully treated more than 150 pertrochanteric fractures with this technique.27
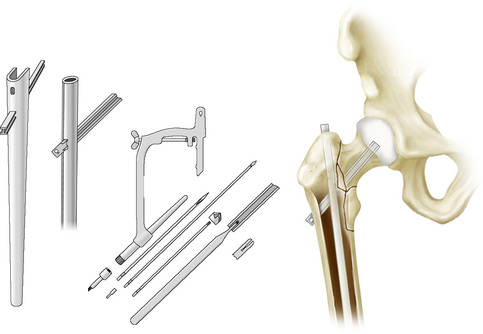
Figure 13-5 Küntscher Y-nail and nail insertion set.
(Redrawn from Küntscher G, Maatz R. Technik der Marknagelung. Leipzig: Thieme; 1945; and Küntscher G. Die Marknagelung. Berlin: Saenger; 1950.)
The Y-nail method had its advocates as well as its critics. In 1983, almost 40 years after its introduction, this technique was described in detail in a monograph by Maatz et al.28 This publication includes quotations from surgeons who had used the technique.
In 1962, Küntscher29 modified his approach. Indeed, he reversed it by introducing the transverse nail to the femoral neck first and then, through the opening in the transverse nail’s lateral widened part, inserting the intramedullary nail from the tip of the greater trochanter into the medullary canal.
Zickel Nail
In 1967, another intramedullary nail was described by Zickel.30 This device was intended for subtrochanteric fractures and resembled the Küntscher Y-nail in shape. The form of the Zickel nail followed the shape of the femoral medullary cavity, with its proximal portion curved in valgus as well as in anteversion. After reaming, a tri-fin nail was inserted into the femoral head at an angle of 125 degrees with the help of a targeting device and a guidewire. This nail was locked into position by a locking bolt inserted from the apex of the widened proximal part of the intramedullary nail (Fig. 13–6).
Russell-Taylor Nail
As a result of a combination of advantages of intramedullary nail and a principle of gliding screw of femoral neck, reconstruction nails (second-generation nails) were created. Reconstruction nails are antegrade femoral intramedullary nails designed to provide locking into the femoral head. They were originally designed for subtrochanteric femoral fractures, pathologic femoral fractures, and selected ipsilateral femoral neck and shaft fractures. The original reconstruction nail was the Russell-Taylor reconstruction nail introduced in 1986.31 It was a closed-section implant for piriformis fossa entry. A pair of cancellous bone screws is directed into the femoral head at an angle of 135 degrees through the proximal widened part of the nail. This device is a long reamed nail with distal locking.
Gamma Nail
The Gamma nail is a prototype cephalomedullary nail with serious implant-related complications, such as fractured shaft of the femur (17%),32–35 failure of fixation (7%),33,34,36 and complications of distal locking (10%),19,37 requiring reoperation. The shape of the proximal fragment in subtrochanteric fractures offers three areas for nail fixation: the subchondral bone of the femoral head, the lateral cortex below the vastus ridge for lag screws, and the apex of the greater trochanter for the proximal part of the nail. This firm fixation in the proximal fragment results in increased bending forces acting on the nail and in some cases also in its breakage.20,33,37–40 Excessive bending stress acting on the implant in subtrochanteric fractures was confirmed by biomechanical studies carried out by Mahomed et al41 and Rosenblum et al.42
Most the technical failures consist of collapse of the fracture area and cutting out of the neck screw as a result of the rotation potential of the femoral head-neck fragment. Nevertheless, the initially high incidence of complications was caused not by the design of the implant but rather by the lack of experience in the treatment of reverse intertrochanteric fractures with intramedullary hip nails. Therefore, the prevalence of complications decreased significantly with the number of nails implanted.37 Moreover, further progress in design gradually gave rise to the third generation of Gamma nail, which was associated with reduced prevalence and types of complications.37
Gliding Nail, Proximal Femoral Nail, Proximal Femoral Nail Antirotation, Targon-PF
In 1997, the AO/OTA developed the proximal femoral nail (PFN), which has two proximal screws, the lower load-bearing neck screw and an additional antirotation hip screw. Among the main benefits of the PFN is the possibility for dynamic locking, a longer nail (PFN, 240 mm; Gamma nail, 200 mm), and a shaped distal part of the nail. This shape distributes the bending forces over a longer part of the femoral shaft and, together with the position of the locking holes, significantly reduces the risk of femoral shaft fracture in the region of the nail tip.22,43 In addition, the PFN eliminates the necessity for distal reaming and thereby reduces the duration of the surgical procedure. The data published so far confirm the PFN to be a reliable implant with results comparable to other nails results in unstable proximal femoral fractures.18,24,44–47 However, various investigators have reported screw cutout of the femoral head-neck fragment.18,19,24,46
Wang et al48 conducted an experimental study comparing the efficacy of using a single femoral neck screw versus two femoral neck screws along with the intramedullary nail. These investigators concluded that two lag screw configurations should be avoided in patients who have a high risk of osteoporotic cutout. The recommendation of these investigators for intertrochanteric fractures in elderly patients with poor bone quality was to use the single screw nail design. In 2004, the AO/OTA developed the proximal femoral nail antirotation (PFNA), to improve rotational and angular stability with one single element. The PFN-A (Synthes, Solothurn, Switzerland) is based on a similar concept, whereby the load carrier for the femoral neck is a helical blade providing rigid rotational stability. This nail proved its value mainly in treating elderly patients with osteoporotic bone.
The special feature of the Gliding nail (Plus Orthopedics, Rotkreuz, Switzerland) lies in the geometric profile of the femoral head stabilizer, which is designed as a double-T blade.19
Entry openings for proximal screws are in anteversion of 8 to 15 degrees in relation to the plane of insertion of distal screws. Nail femoral neck-shaft angles vary between 125 and 135 degrees.49 One or two screws, or in some cases a helical blade (PFN-A) or double-T blade (Gliding nail), are introduced to the femoral neck and head to provide rigid rotational stability. The lag screws vary between 5 and 12 mm. Reconstruction nails are typically enlarged proximally to compensate for the higher stress in the subtrochanteric region. This feature must be taken into account during preoperative planning because additional reaming of the proximal fragment will be necessary.49 Distal interlocking screws vary from 4.5 to 6.4 mm in diameter. Especially when using the short version of the nail, a surgeon has a choice between static and dynamic distal locking.
Letzius Nail
In 1950, Letzius50 described treatment of pertrochanteric and subtrochanteric fractures using a curved nail that was introduced into openings in the diaphyseal medial cortex and trepanned 10 to 12 cm under the level of the lesser trochanter (Fig. 13–7). The author reported a group of 22 patients treated with this method.
Küntscher Condylocephalic Nail
In 1966, Küntscher51 described osteosynthesis of pertrochanteric fractures with a long, curved nail, 9 mm thick, that was inserted from medial femoral condyle with help of a guidewire. Küntscher noted that he elaborated the ideas of Letzius and Herzer.
Ender Nailing
Based on the principle of condylocephalic nailing and the ideas proposed by Hackethal, another method of intramedullary nailing was introduced into practice in 1969 by Ender and Simon-Weidner.52 This method was received with much enthusiasm, and in the 1970s and 1980s, many proximal femoral fractures (mostly pertrochanteric and subtrochanteric) were treated with Ender nailing. However, the analysis of outcome revealed unsatisfactory results, mainly in patients with unstable fractures, and the technique was gradually abandoned.
Classification
Several classification systems of subtrochanteric fractures have been suggested.
Boyd and Griffin
Boyd and Griffin53 originally called attention to subtrochanteric fractures as a variant of pertrochanteric fractures and noted a higher incidence of unsatisfactory results after operative treatment. These investigators divided all trochanteric fractures into four types (I to IV). In this system, type III represents subtrochanteric fractures, and type IV comprises subtrochanteric fractures with intertrochanteric extensions.
Fielding and Magliato
In 1966, Fielding and Magliato13 developed a classification especially for subtrochanteric fractures. This system recognized three types of fractures, based on the location of the primary fracture line in relation to the lesser trochanter. Type I includes fractures at the level of the lesser trochanter, type II signifies fractures within 1 inch (2.5 cm) below the lesser trochanter, and type III fractures are within 1 to 2 inches (2.5 to 5 cm) of the lesser trochanter. However, this classification does not address the problem of comminution, which is critical in fracture stability assessment.
Zickel
In 1976, Zickel suggested a six-part classification system that included long spiral fractures and trochanteric extension.31 He used his classification system to emphasize the need for adjunctive fixation with his cephalomedullary nail for prevention of rotational and length deformity.
Seinsheimer
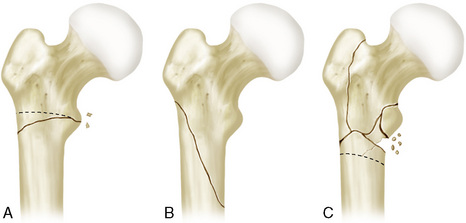
In 1978, Seinsheimer54 proposed a complex but concise classification, based on the number of major fragments and the location and shape of fracture lines (Fig. 13–8). This classification involves eight subgroups:
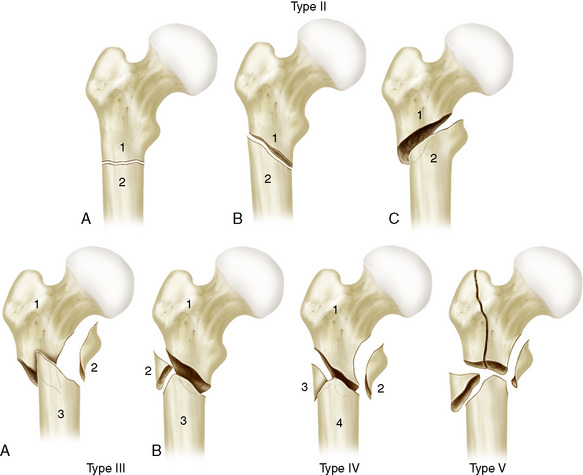
Figure 13-8 Seinsheimer classification of subtrochanteric fractures (see text for description).
(Redrawn from Seinsheimer F. Subtrochanteric fractures of the femur. J Bone Joint Surg Am 1978;60:300-6.)
Waddell
In 1979, Waddell55 recommended another classification with three major subgroups: transverse or short oblique fractures, long oblique fractures, and comminuted fractures with extension into the trochanteric mass (Fig. 13–9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree