19 Best Surgical Practices
Overview
Almost all patients with proximal femoral fractures require operative treatment, with the exception of those who are moribund or those at extremely high surgical risk.1 Surgical options include partial or complete joint replacement arthroplasty versus various intramedullary or extramedullary fixation techniques and implants. Careful preoperative planning must take into consideration the patient’s medical status, functional demands, social situation, bone quality, and fracture configuration before a surgical tactic can be articulated. Surgical risk of mortality must be weighed against expected functional outcome, as well as the consequences of possible nonlethal complications including the potential need for additional future surgery.
The concept of best surgical practice implies that an optimal surgical tactic for that particular patient is applied in expert fashion after consideration of all the relevant factors. Although surgical excellence and implant selection are the focal points of this chapter, it is important to understand that short-term and long-term patient outcome is influenced greatly by factors not directly related to the surgical technique. These factors include perioperative pain management and transfusion regimen, delay to surgery, the type of anesthetic regimen, the rehabilitation protocol, and secondary prevention strategies to improve bone quality and to prevent future falls and fractures. Finally, this chapter considers only proximal femoral fractures involving traumatic injury through normal or osteopenic bone. Stress fractures resulting from overuse or metabolic abnormality have characteristic patterns of failure and require additional considerations that are not covered in this chapter.2 The management of pending or completed fractures through metastatic lesions or around previous implants is also beyond the scope of this chapter.3
Optimal Surgical Tactic
Although it is important to contemplate the best available evidence from the literature when planning a surgical tactic, published reports and literature summaries are limited in their application to decision making for an individual patient. Whereas groups of implants (e.g., extramedullary versus intramedullary) can be compared for broad fracture groupings, the nuances of biomechanical fixation strategies for each of the fracture components are rarely articulated, although they are sometimes coincident with a specific implant. Moreover, very little evidence exists on the effects of various types of malunion (varus, extension, loss of hip offset, metaphyseal shortening, rotation) on functional outcome, although investigators have demonstrated that femoral neck shortening seems to be associated with compromised Short Form 36 (SF 36) physical functioning scores.4 Thus, it is difficult to choose between a surgical procedure that restores anatomic positioning of the articulation and a procedure with guaranteed malunion but less chance of nonunion and a systemic risk of morbidity and mortality (e.g., replacement arthroplasty or absolute stability in anatomic position with a locked screw or plate versus dynamic neck and metaphyseal sliding compression with a Medoff plate).
Postoperative Weight Bearing
Whatever strategy is chosen, it should enable the elderly patient to mobilize immediately without restricting weight bearing after the surgical procedure. It has long been accepted that early mobilization of elderly patients, including those with hip fractures, is critical to avoiding medical problems such as skin, cardiovascular, respiratory, and gastrointestinal complications.5 Moreover, immediate weight bearing after hip fracture surgery has been shown to decrease medical complications,6 decrease mortality,7 improve functional recovery,6,7,8–11 and accelerate discharge from the acute care hospital.9,12 Furthermore, evidence indicates that patients limit the amount of weight placed through the operated limb depending on the stability of the construct,13 and failure rates are not increased with an immediate weight-bearing protocol even in patients with unstable fracture patterns with traditional implants.14,15 Finally, careful surgical planning and the availability of a wide variety of implants allow for fixation or for replacement that is compatible with postoperative weight bearing in all fractures, including those previously considered biomechanically “unstable” after surgery with certain surgical strategies and older implants.16–21
Surgical Strategies
Intracapsular Hip Fractures
Overview
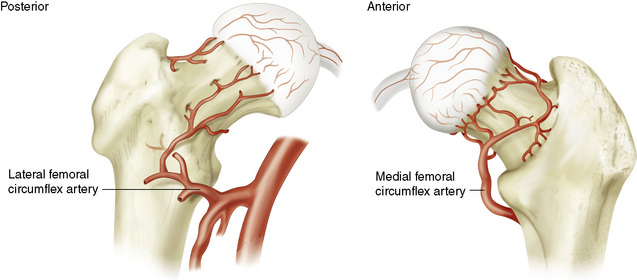
The blood supply to the femoral head originates from the medial and lateral femoral circumflex artery, the intramedullary blood supply, and with a small contribution from the obturator artery through the ligamentum teres in childhood (of limited importance in adults) (Fig. 19-1). An intracapsular fracture of the femoral neck with displacement of the fracture results in disruption of the intramedullary blood supply to the femoral head and jeopardizes flow through the vital terminal intracapsular branches of the medial and lateral femoral circumflex arteries by direct disruption, hematoma pressure, or spasm resulting from vessel distortion. The more displaced the fracture, the more damage these vessels will sustain. Avascular necrosis (AVN) and nonunion are therefore relatively common in femoral neck fractures with significant displacement and have been reported in more than 50% of patients in some series.22 According to published evidence, the incidence of AVN may be lower in men (4.9% in men versus 11.4% in women) and appears to decrease with advancing age (20.6% age <60 years versus 2.5% age >80 years).23
Femoral Neck Fractures: Definitions
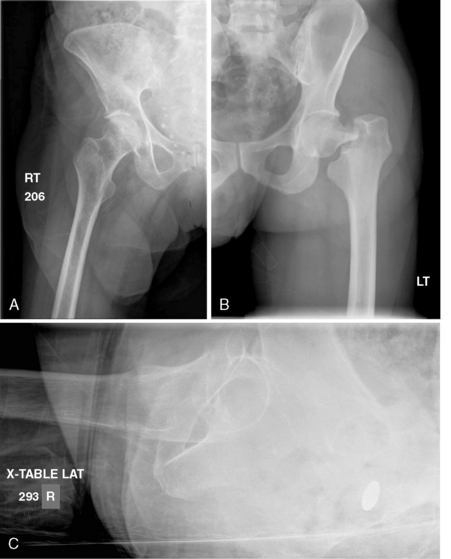
Intracapsular femoral neck fractures are best grouped into two categories to denote the degree of stability and displacement across the fracture site. Stable fractures have some structural continuity across the fracture site (i.e., fracture impaction) such that the two fragments would be expected to move as a unit with application of a small amount of external force such as hip rotation (Fig. 19-2A). Unstable fractures have no continuity across the fracture site such that the two fragments would be expected to move independently with application of minimal force24 (see Fig. 19-2B).
Alternatively, the terms undisplaced or displaced may be used to define stable and unstable fractures. However, there may be confusion with respect to fractures that have impaction and angular displacement across the fracture site (i.e., valgus impaction); some surgeons may consider the fracture to be displaced when it is in fact stable. In this chapter, the term displaced is used interchangeably with unstable to mean that no structural continuity connects the fracture fragments. Both the anteroposterior (AP) and lateral radiographs must be carefully scrutinized for signs of fracture gap, angulation, translation, and rotation before the fracture can be definitively categorized as stable or unstable (see Fig. 19-2C).
Stable Femoral Neck Fractures Should Be Fixed
Stable femoral neck fractures should be treated with surgical fixation and immediate unrestricted activity because nonoperative treatment has a high failure rate and the results of minimally invasive surgery are generally good, with a low risk of complications.25,26 Failure of nonoperative treatment resulting in fracture displacement would convert the previously stable subcapital hip fracture to the unstable femoral neck fracture category discussed in the next section, in which the surgical risks are higher. Multiple lag screw fixation and minimally invasive sliding hip screw insertion are both acceptable surgical treatment options for stable femoral neck fractures that result in dynamic compression across the fracture site.27
Important surgical and implant-related details are discussed here because they are similar to unstable intracapsular hip fractures. Replacement arthroplasty is associated with a higher risk of mortality and morbidity compared with fracture fixation for stable femoral neck fractures.23 However, some emerging evidence indicates that approximately 30% of stable fractures treated with internal fixation may be subject to femoral neck shortening and compromised SF 36 scores.28
Unstable Femoral Neck Fractures: Replacement Versus Fracture Fixation
There is considerable debate regarding the optimal treatment of displaced femoral neck fractures in active, high-demand older adults.18,29–32 Failure rates of surgically fixed unstable intracapsular hip fractures increase progressively from approximately 6% in patients in their 40s to 25% in patients more than 70 years old.33
Some high-quality randomized trials have suggested that replacement arthroplasty produces better results than fracture fixation in elderly patients with subcapital hip fractures.34–36 Moreover, replacement arthroplasty for intracapsular fractures that have failed after primary fixation is less successful than primary arthroplasty; this finding implies that it is optimal to make a definitive choice regarding treatment at the time of initial presentation.37,38 For these reasons, the trend has been for an increasing number of unstable femoral neck fractures to be treated with replacement arthroplasty, especially in elderly patients.39 Arthroplasty significantly reduces the likelihood of requiring revision surgery at 1 year.40
Even though arthroplasty is associated with an increased risk of infection, blood loss, and prolonged operating time, it does not appear to increase the mortality risk at 1 year.40 Mortality is driven mainly by the patient’s comorbidity, age, and gender with lesser contributions from other factors under the control of the medical team.41 However, evidence indicates that the surgeon and hospital environment and experience do contribute to patients’ morbidity and mortality.41–45 Whether primary fixation or primary replacement arthroplasty is chosen (cemented or uncemented), the postoperative rehabilitation protocol should involve immediate full weight bearing for the reasons mentioned earlier.
Fracture Fixation Tips, Tricks, and Controversies
In an active, high-demand, healthy older adult with good bone quality and a displaced subcapital hip fracture with minimal comminution (such that femoral neck length is likely to be maintained with fixation), fracture fixation may be the surgical procedure of choice.46 Anatomic reduction and stable internal fixation are essential to successful outcome.
Timing of reduction and fixation for displaced femoral neck fractures remains controversial.22,47 However, expeditious surgical treatment has the theoretical advantage of early restoration of femoral head blood supply that could decrease the risk of AVN.48 While the patient is awaiting surgery, the hip should be allowed to remain in a shortened and externally rotated position without traction. This has been shown to minimize both pain and intracapsular pressure.22,49,50
Reduction
Once the patient is anesthetized, a careful attempt at closed reduction should be carried out by gently flexing the hip to approximately 45 degrees while retaining the abducted and externally rotated position. Traction is then applied, and the hip is gently brought into a position of internal rotation, extension, and adduction to neutral. This maneuver can be performed with the patient on a fracture table, if desired, so that the limb can be immobilized in the traction boot without transferring from one table to another if the reduction is successful. Successful reduction is best judged fluoroscopically on both the AP and lateral views (Fig. 19-3). A symmetrical S-shaped curve on either side of the femoral head and neck on both views indicates that good reduction of the fracture has been achieved.22,51 Particular care should be paid to the inferior femoral neck area because anatomic integrity of this region is key to avoiding varus collapse and displacement.
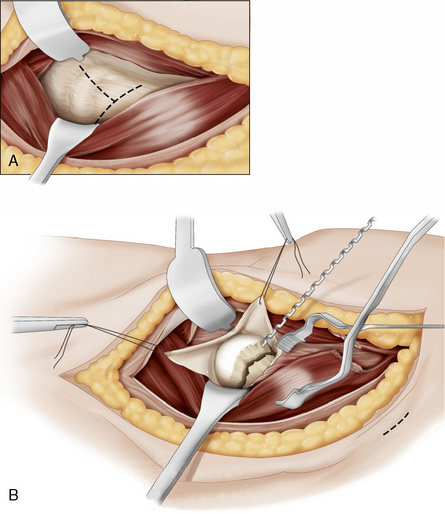
Failure to achieve an adequate closed reduction demands open reduction and internal fixation. This is easiest to perform with the leg out of traction on a radiolucent table.22 A Watson Jones or Smith Peterson approach can be used to treat the fractured femoral neck.22,51 When a Smith Peterson approach is used, femoral neck fixation is usually performed through a separate lateral percutaneous approach. The capsule can be opened in a T-shaped configuration, with the transverse release performed along the intertrochanteric ridge22 or along the acetabular margin, with care taken to avoid damage to the labrum (Fig. 19-4). Once the fracture is exposed, a small (2.5-mm) terminally threaded Kirschner wire drilled into the distal fragment can be used to manipulate the femoral head into alignment with the neck. The shaft fragment can usually be controlled by simple manipulation of the limb, but it may be augmented by insertion of a 4.5-mm Shantz pin into the femoral shaft.51 The subtrochanteric region should be avoided during this procedure, to minimize the risk of subsequent stress fracture through the hole. Depending on the obliquity of the fracture, pointed reduction forceps may be applied to hold the reduction. A sharp hook can also be useful to maintain the reduction of the medial calcar region, which is key to avoiding fixation failure and varus collapse.51 A temporary Kirschner wire can then be drilled across the fracture from the lateral cortex to allow for image confirmation of the reduction and definitive fracture fixation. Fracture reduction is facilitated by full muscle paralysis.
Fixation
Placement of multiple lag screws (cannulated or noncannulated) is the most popular form of fixation for displaced and undisplaced femoral neck fractures. The use of a single large screw as part of a sliding hip screw construct has the theoretical disadvantage of allowing the head to spin in the final stages of screw tightening (despite the use of derotation wires or screws), an action that could lead to further damage to blood vessels and loss of fracture interdigitation. However, the literature provides no evidence that AVN rates are related to the type of implant used, although multiple screw procedures are faster to perform and are associated with less blood loss than a sliding hip screw construct.52
The number and configuration of multiple screw fixation are debated. Biomechanical evidence supports the use of two or three screws placed parallel to one another and widely separated within the femoral neck. A lag screw along the calcar is key to minimizing the risk of neck displacement into varus. Because the lateral femoral cortex is under tension, drill holes in the subtrochanteric region should be avoided to minimize the risk of stress fracture. Thus, all screws should originate above the lesser trochanter. Some surgeons advocate the use of three screws in an inverted triangle configuration to minimize subtrochanteric stress.22
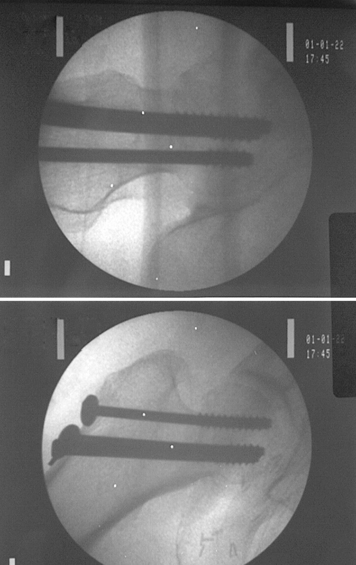
Lag screws should be placed deeply into the femoral head to engage the subchondral bone (Fig. 19-5). Fluoroscopically, placement can be evaluated by rotating the head or the image intensifier along the axis of the femoral neck and again transversely to it. Each screw should be seen to approach and then recede from the subchondral margin during rotation. If the screw is more than a few millimeters from the subchondral bone (at the closest position), a longer screw should be considered. Penetration of a screw beyond the cortex on any view must not be tolerated; 6.5-mm noncannulated or cannulated 7.0- or 7.3-mm screws are commonly used. The 32-mm threaded lag screws are preferred if possible, but all threads must end up within the femoral head. If there are threads crossing the fracture line, a 16-mm threaded screw is chosen. Occasionally, a fully threaded screw is used across a comminuted posterior neck fracture to prevent collapse in this region. These technique details have not been evaluated in randomized clinical trials.
Replacement
Controversy exists regarding the type of replacement arthroplasty that is optimal in patients with displaced subcapital hip fractures.40,53,54 Partial versus total hip replacement and cemented or uncemented stem fixation are the main points of debate. Current best evidence suggests that total hip arthroplasty reduces hip pain, may improve function, and decreases the risk of reoperation as compared with hemiarthroplasty.40 It has been difficult to demonstrate clinical differences between unipolar and bipolar hemiarthroplasty, but bipolar implants have a higher cost.55
A review of studies comparing cemented with uncemented stems for the treatment of unstable subcapital hip fractures noted better function and decreased pain with cemented implants, with no difference in mortality, but the stems compared were mostly of older design.56 More recent evidence suggests that when a modern stem design is used, there appears to be no functional difference between uncemented and cemented stems with respect to patient function.57
Uncemented implants are associated with less fat embolization and less pulmonary shunting.58 In healthy patients, the incremental fat embolization associated with cemented femoral stem insertion may be insignificant.59 However, the incremental pulmonary shunting associated with cementing of the femoral stem may be important in sicker patients with less cardiopulmonary reserve.60,61 If cement is used in a medically fragile elderly patient, care must be taken to prepare the canal adequately with thorough irrigation to remove marrow fat, and consideration should be given to supplementary techniques to decrease canal pressurization, such as bone vacuum application.62 Larger and higher-quality trials will be required before definitive guidelines can be provided regarding modern femoral stem insertion with or without cement in healthy and medically compromised elderly individuals with respect to mortality and functional outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree