1 Epidemiology/Population Studies
Scope of the Problem
Hip fracture represents a tremendous burden on the health care system and public health in general. More than 320,000 people were admitted to hospitals for hip fracture in 2004 in the United States.1 In 1996, the Centers for Disease Control and Prevention estimated the annual cost of hip fracture to be $2.9 billion.2 Today, by some estimates that include all direct and indirect costs, it is as high as $12 billion.3 Even more strikingly, in 1990 it was projected that by 2040 there will be between 530,000 and 840,000 incident cases of hip fracture per year in the United States.4 From an economic perspective, the cost of hip fracture is tremendous. The morbidity and mortality secondary to hip fracture are equally astounding. Roughly 20% of patients who have hip fracture, or 1 in 5, will die in the year following the fracture,5 and most of these patients will die in the first months of recovery.6 Disability increases substantially following hip fracture and is such that the attendant musculoskeletal dysfunction puts the patient at even higher risk for a second fracture or multiple fractures.
Frailty
Frailty represents a syndrome and therefore is recognized as a cluster of symptoms.7 The syndrome is expressed as diminished physiologic reserve, which is characterized by gait and balance abnormality, weight loss, muscle weakness, loss of energy, and diminished physical activity.7–10 Frailty is a serious public health burden because the syndrome is associated with increased risk of falls, low-velocity fractures, significant disability, and mortality.11 Indeed, these sequelae often follow this course directly as a chain reaction. Moreover, the syndrome components are generally highly correlated and interactive. For example, physical inactivity leads to increased muscle weakness and diminished gait performance, which in turn make physical activity, ambulation in particular, more difficult. This aggregation of risk through cumulative causal pathways hastens the progression of frailty and leads to more substantive disability, which may be directly related to, or entirely independent of, a traumatic event (e.g., hip fracture).
Consensus on the clinical designation of frailty has proven difficult, particularly because many clinicians consider frailty and disability synonymous. This viewpoint misses the relevance of preclinical frailty for the development of subsequent morbidity and disability and in turn causes the opportunity for early preventive intervention to be lost. For example, in the context of musculoskeletal dysfunction and hip fracture in particular, gait has been closely associated with frailty in clinical practice. Gait is defined as the pattern of movement during walking and is generally a key component to the frailty complex. The importance of walking to the overall maintenance of homeostasis cannot be overstated. Normal musculo- skeletal, cardiopulmonary, and neurologic functioning are mediated in no small part by the mechanics and chemistry of walking. Moreover, the components of gait strongly influence the mechanics of walking. These components are gait speed, walking cadence (the number of steps walked over a given time period), and stride length. The degeneration in gait speed associated with normal aging appears to result from a decrease in stride length rather than a reduction in cadence.12 This finding is important because diminished gait speed can be improved in aging individuals with proper physical conditioning.
The Frailty Task Force of the American Geriatric Society proposed a list of criteria to be used in classifying frailty that is now accepted as a working definition for clinical practice.7 According to this definition, the frailty syndrome is defined by three or more of the following symptoms: (1) unintentional weight loss (4–5 kg in year); (2) self-reported exhaustion; (3) weakness (grip strength <20% in the dominant hand); (4) slow walking speed (<20% for time to walk 15 feet); and (5) low physical activity (<20% for caloric expenditure).7 Important clinical manifestations of the frailty syndrome include, but are not limited to, gait and balance deficits, sarcopenia, osteopenia and osteoporosis, diminished maximum oxygen consumption (Vo2max), and potentially elevated or hypertensive blood pressure. Most of these disorders lie directly on the causal pathway to hip fracture and poor outcomes following fracture. Because the inability to respond to stress or physical insult typifies frailty, the frail patient with a hip fracture begins to recover from a baseline that is already in deficit, which retards the body’s adaptive response during convalescence. Consequently, frailty sets the stage not only for the hip fracture itself but also for the inability to recover from that fracture.
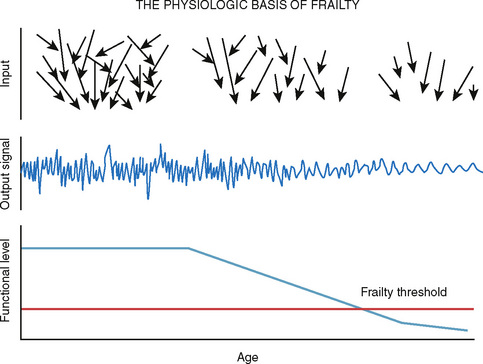
Lewis Lipsitz further developed the concept of frailty as a lack of complexity in dynamic systems that leads directly to a loss of what he called “reactive tuning.”13 Complexity underlies adaptive systems. It is what allows a system to adapt to the events that stress the system. Complexity allows for versatility and provides robustness in the presence of environmental challenge (Fig. 1-1).
For example, the autonomic nervous system, by way of sympathetic and parasympathetic activity, is responsible for the beat-to-beat variability in heart rate and blood pressure. Endocrine and temperature cues regulate heart rate and blood pressure on scales of minutes to hours, and circadian rhythms regulate across days. Although there may be large variability within any level of internal regulation, the patterning of heart rate and blood pressure is similar across these times scales, a characteristic known as self-similarity. Self-similarity is a key component to the fractal dimensions of complex systems and indeed is largely responsible for the robustness of complex systems.13 This is why they are adaptive, and this adaptiveness maintains equilibrium. For example, loss of heart rate variability has been recognized as an important trigger for arrhythmia and tachycardia in heart disease and is a common characteristic of aging.13 More precisely, the system’s complexity allows it to maintain a steady state by myriad self-similar processes. Whereas cardiovascular fitness is an important component of frailty, the adaptation of complex systems is also relevant to the musculoskeletal components of frailty. Specifically, the loss of trabecular bone architecture represents a breakdown of the architectural scale (i.e., a self-similar scale), which directly contributes to bone strength. Stride length, considered one of the most important aspects of gait that can lead to falls, becomes less variable over time. It thus represents a less complex system and therefore is less responsive to environmental or physical challenges.
Center of pressure (COP) is also greatly affected by loss of complexity. COP and posture are strongly related to balance and stability. However, to produce stability, COP requires ongoing displacements (sway). Thus, as greater complexity is introduced into the system, greater stability will result from the system’s need to adapt continuously. All the foregoing examples highlight reactive tuning in complex systems and identify clear pathways to frailty and its consequences when the tuning fails.13 In other words, we can think of complexity in a system as an ongoing process of challenge or stimulation.
Falls and Fractures
In 1989, Steven Cummings and Michael Nevitt, two prominent researchers in frailty and fracture, wrote a hypothesis article on the causes of hip fractures.14 This hypothesis mapped falling onto fracture and essentially detailed the causal association between two distinct but strongly associated clinical events. These researchers outlined four necessary conditions that must be present for the hip to fracture on falling. First, the fall must be oriented to land on or near the hip. Second, protective responses must be inadequate to reduce the energy of the fall below a critical threshold for fracture. Third, the soft tissue surrounding the joint must be inadequate to absorb enough of the fall’s energy to prevent the fracture. Fourth, bone strength must be insufficient to resist the residual energy transferred to the hip during the fall (Fig. 1-2).14
Before this hypothesis was proposed, conventional thought in hip fracture prevention directed practice to focus primarily on the integrity of bone. As a result, interventions often took the reductionist approach of trying to improve bone mineral density with calcium supplementation. By elucidating a theoretical framework for hip fracture risk that was more systemic, Cummings and Nevitt were able to ground hip fracture in a continuum of declination associated with frailty. Orientation of a fall, for example, is highly dependent on forward momentum or, more specifically, on gait speed during walking. Slower gait speed or shorter stride length, therefore, is more likely to cause an individual to fall down rather than forward while walking. Muscle strength is also directly relevant in fall orientation during transfer motion, and balance, with its associated corrective posturing (reactive tuning), is relevant for falls and their downward orientation when there need not be any movement at all. Poor protective responses include slowed reaction times and decreased muscle strength, both of which may lead to an increased likelihood of falls and diminished capacity to recover from the fall as well as a redirection of the forces involved to obviate a hip fracture. In addition, age-related comorbidity (e.g., distal polyneuropathy, dementia, syncope) can easily reduce responsiveness to one’s environment and can thus inhibit protective responses.14 Soft tissue, which reduces the energy transferred to the bone on impact, is very important for absorbing the energy of a fall.14 Weight loss, which can include loss of both fat and lean muscle mass, is a nontrivial component of frailty and often attends the aging process for many individuals. These soft tissues are invaluable as shock absorbers. Their loss removes an individual’s last line of defense in a fall. Moreover, a frail person is likely to have diminished reactive responses to falls, as described earlier, and will hit the ground in an unfavorable orientation with no extra padding to protect from fracture. Finally, the last associative link between falls and fractures outlined by Cummings and Nevitt is the composition of the bone itself. Bone’s ability to endure insult is a composite of mineral content (bone mineral density) and bone architecture (number of trabeculae and width and diameter of cortical bone). These aspects of bone strength are a function of hormonal regulation of bone turnover, nutrition, and mechanical loading by the musculature and overall body mass. Importantly, all these factors are strongly associated with aging. Moreover, frailty is characterized by weakened bone precisely because of hormone dysregulation, undernutrition, and diminished loading of bone resulting from weight loss, muscle weakness, and functional dependence.14
Inertia is a prominent theme in our discussion of frailty and falls. Indeed it is central not only to the understanding of hip fracture risk, but also to its outcomes, as described in the next section. There is a strong body of evidence for the role played by activity in hip fracture risk. In the 1980s, Boyce and Vessey conducted a study on all femoral neck fractures in patients admitted to all hospitals in the city of Oxford in the United Kingdom.15 This study is significant because (1) it was population-based and (2) it was composed of a relatively healthy and mobile group of patients because 139 of 333 of these patients passed the cognitive and functional screening test. As such, although we would expect that an activity effect in this group would be attenuated toward the null because the cases would be more similar to controls, the investigators found a strong, significant association between physical inactivity and risk for hip fracture.15
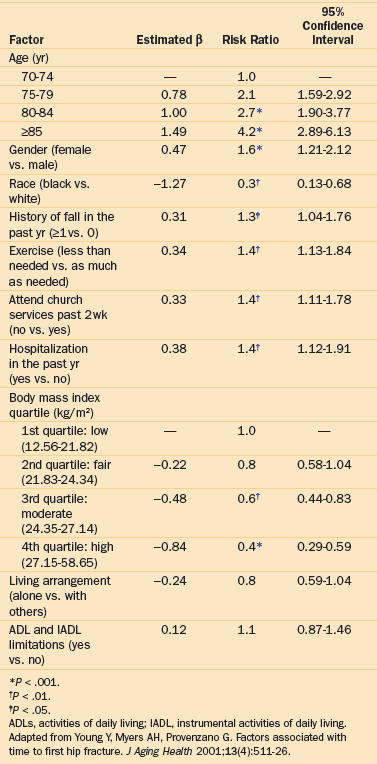
Another population-based study was conducted in the United Kingdom 5 years later in the borough of Newcastle.16 This study identified a similar number of hip fractures in the municipality (N = 312), although 65% of patients passed the mental screening examination for this study (197 of the 303 eligible subjects). The results showed that patients who did no walking each day were three and a half times more likely to fracture their hip even after adjusting for body mass index (BMI), smoking, and dependence in activities of daily living (ADLs) (odds ratio [OR] = 3.4; 95% confidence interval [95% CI], 1.7 to 6.8).16 The Longitudinal Study of Aging, a population-based study in the United States that was part of the National Health Interview Survey, identified 334 incident fractures among the 7153 eligible community participants.17 This important study identified a history of previous falls in the past year (OR = 1.3; 95% CI, 1.04 to 1.76), lack of exercise (OR = 1.4; 95% CI, 1.13 to 1.84), social engagement (OR = 1.4; 95% CI,1.11 to 1.78), and hospitalization in the previous year (OR = 1.4; 95% CI, 1.12 to 1.91) as predictors of hip fracture, all independent of age, gender, race, and BMI, which were also strong predictors of hip fracture (Table 1-1).17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree