Fig. 4.1
(a) Normal positioning for PA view of the second digit. (b) Normal PA radiograph of the second digit
Lateral View
The lateral view of the finger is obtained by turning the finger 90° from the PA position. The second and third digits are internally rotated, and the fourth and fifth digits are externally rotated. It is important that the lateral view of the injured finger be free from overlap with the other fingers. Any overlap will create difficulty in evaluating displacement or angulation of fractures, especially at the base of the proximal phalanx (Fig. 4.2).
Fig. 4.2
(a) Normal positioning for lateral view of the second digit. (b) Normal lateral radiograph of the second digit
Oblique View
In the oblique view, the affected finger is rotated externally 45° from the PA position. In this position the interphalangeal and metacarpophalangeal joints are open. If multiple adjacent fingers are imaged, they must be spread apart to avoid overlap (Fig. 4.3).
Fig. 4.3
(a) Normal positioning for oblique view of the second digit. (b) Normal oblique radiograph of the second digit
4.1.2.2 Radiographic Evaluation of the Metacarpals
Radiographic evaluation of the metacarpals should include a standard three-view radiographic examination, which will reveal most fractures and dislocations [2]. Metacarpal fractures are common and account for up 30–40 % of all hand fractures [4]. These fractures are typically the result of direct trauma, but fatigue fractures can occur in athletes due to repetitive stress.
PA View
The PA view is obtained with the hand opened, pronated, and placed flat against the cassette. The fingers are spread apart so that the lateral soft-tissue margins do not overlap. Care should be taken to assure that the interphalangeal, metacarpophalangeal, and carpometacarpal joints are projected open. The entire hand should be included from the distal phalanges through the distal forearm (Fig. 4.4).
Fig. 4.4
(a) Normal positioning for PA view of the hand. (b) Normal PA radiograph of the hand
Lateral View
In the lateral view, the hand is positioned with the ulnar side down, radius and ulna superimposed. For foreign body localization, the hand is placed in extension, with all bones superimposed (Fig. 4.5).
Fig. 4.5
(a) Normal positioning for lateral view of the hand. (b) Normal lateral radiograph of the hand
In the fan (flexion) lateral view, the fingers are flexed and spaced like a fan. This allows visualization of the interphalangeal and metacarpophalangeal joints. In a well-positioned fan lateral view, the second through fifth metacarpals should be superimposed (Fig. 4.6).
Fig. 4.6
(a) Normal positioning for fan lateral view of the hand. (b) Normal fan lateral radiograph of the hand
Oblique View
The oblique view is obtained by obliquing the hand externally 45° to the tabletop. An accurately positioned oblique view will demonstrate the heads of the second and third metacarpals without superimposition and slight superimposition of the fourth and fifth metacarpal heads. In addition, the phalangeal joints should be open without overlap of the proximal and distal articulations (Fig. 4.7).
Fig. 4.7
(a) Normal positioning for oblique view of the hand. (b) Normal oblique radiograph of the hand
4.1.2.3 Radiographic Evaluation of the Thumb
The thumb’s distinct osseous structure including its specialized basilar joint and its natural position causes unique injury patterns. Most fractures of the thumb will be visible on a two-view radiographic examination. Moreover, studies have shown an increased diagnostic yield when an oblique projection is added [2], which can be obtained together with a PA examination of the whole hand. Some practices will include the PA and lateral views described by Kapandji [5].
Anteroposterior (AP) View
The AP view (Robert’s view) of the thumb is obtained with the hand internally rotated so that the thumbnail rests against the cassette. There should be no rotation of the phalanges and metacarpals. In this position the interphalangeal, metacarpophalangeal, and carpometacarpal joints should be opened (Fig. 4.8).
Fig. 4.8
(a) Normal positioning for AP view of the thumb. (b) Normal AP radiograph of the thumb
Lateral View
The true lateral view (Bett’s view) requires the hand to be flexed and slightly rotated externally to achieve a true lateral. All views of the thumb should demonstrate the carpometacarpal joint through the distal phalanx (Fig. 4.9).
Fig. 4.9
(a) Normal positioning for lateral view of the thumb. (b) Normal lateral radiograph of the thumb
Oblique View
The oblique view is obtained with the thumb in its natural position with the hand in the PA position and flattened against the cassette (Fig. 4.10).
Fig. 4.10
(a) Normal positioning for oblique view of the thumb. (b) Normal oblique radiograph of the thumb
Kapandji PA and Lateral Views [5]
For the PA view described by Kapandji, the hand is positioned with a routine lateral view. The wrist is pronated 15° and extended 15°. The thumb is in the axis of the radius, and the surface of the nail is parallel to the cassette. The X-ray beam is centered on the trapeziometacarpal joint using a 30° cranial inclination. On the X-ray, the sesamoids project symmetrically on the head of the first metacarpal. The scaphoïdo-trapezial joint line is well visible (Fig. 4.11a).
Fig. 4.11
(a, b) Normal positioning for PA and lateral Kapandji views of the thumb and corresponding normal AP radiographs
For the lateral view described by Kapandji, the hand is positioned as with a routine PA view of the hand. The wrist is ulnar deviated till the thumb lies in the axis of the radius. Then the hand is pronated, till the surface of the nail is perpendicular to the cassette. The vertical X-ray beam is centered on the trapeziometacarpal joint. On the X-ray, the first metacarpal and the phalanges of the thumb are in strict lateral view, and the two sesamoids are superimposed (Fig. 4.11b).
4.1.3 Role of Radiography in the Setting of Acute Finger Trauma
In patients with trauma to a finger, radiographs alone provide important diagnostic information and guidance for the treating physician. In many cases, enough information can be obtained to determine if surgery is indicated. The standard three-view radiographic examination will reveal most fractures and dislocations of the metacarpals and phalanges [2]. Plain radiography should be the initial imaging modality in the setting of acute trauma to the finger to exclude any possible avulsion fracture or malalignment. Listed below are examples of how plain radiographs play an important role in the acute setting of finger trauma.
4.1.3.1 Classification
Radiography alone in many instances allows accurate classification of fractures and dislocations. Radiographs can assess the degree of displacement, angulation, shortening, and rotation of fractures. They also allow classification of the fracture type (transverse, oblique, spiral, comminuted, impacted, or avulsion) and if there is extension to the articular surface (Fig. 4.12).
Fig. 4.12
(a, b) A 17-year-old athlete injured fifth digit after fall. Lateral (a) and oblique (b) views of the fifth digit show comminuted intra-articular fracture at the base of the middle phalanx
Close inspection of an apparent extra-articular fracture is required to ensure that no portion of the fracture line involves the joint surface. The majority of thumb metacarpal fractures occur at the base, and the classification system includes whether the fracture is intra-articular versus extra-articular (Fig. 4.13). Discerning whether the articular surface is involved in the fracture is critical as this dictates management. CT scanning is helpful at times, particularly with regard to potential impaction injury and to define the carpometacarpal (CMC) joint and fracture fragment position in intra-articular injuries. Usually the information obtained from radiographs can be enough to determine if surgical treatment is warranted or not.


Fig. 4.13
(a, b) A 22-year-old skier injured thumb after fall. Lateral (a) and oblique (b) views of the thumb show an oblique intra-articular fracture at the base of the first metacarpal (Bennett fracture)
Dislocations of the fingers can be accurately classified by the direction of displacement with dorsal proximal interphalangeal (PIP) joint dislocation being the most common (Fig. 4.14). Despite the inherent stability of the thumb joints, the vulnerable anatomic position of the first phalanges often subjects the joints to mechanical strain that lead to subluxation or dislocation of the metacarpophalangeal (MCP) and interphalangeal (IP) joints. The interposition of the sesamoid within the joint is pathognomonic of a complex dislocation (Fig. 4.15).



Fig. 4.14
A 27-year-old male who sustained a jamming type finger injury. Radiograph demonstrates dorsal dislocation at the PIP joint (Courtesy G. Chick, MD)

Fig. 4.15
A 26-year-old who fell on his thumb. Preoperative radiograph demonstrates dislocation at the first metacarpal phalangeal joint with interposition of the sesamoid bone (Courtesy G. Chick, MD)
4.1.3.2 Mallet Finger
The most common closed tendon injury of the finger is disruption of the extensor tendon of the DIP or mallet finger [6]. In this setting, standard three-view radiographs are important to evaluate for the possible presence of volar subluxation of the distal phalanx as well as a significant intra-articular fracture (greater than 30 % of joint surface). These two observations are important to describe because both are indications for surgery; they are best assessed on a true lateral view (Fig. 4.16). This type of injury usually results from a direct blow to the tip of the finger causing forced flexion of the distal phalanx and extensor tendon injury. The tendon may be partially torn, completely torn, or associated with a distal phalanx avulsion fracture.


Fig. 4.16
A 22-year-old basketball player who injured his middle finger during game. Lateral view of the middle finger demonstrates avulsion fracture from the dorsal base of the distal phalanx (mallet finger)
4.1.3.3 Jersey Finger
In the setting of flexor digitorum profundus tendon injury (jersey finger), which is disruption of the flexor digitorum profundus tendon from its distal attachment, standard three-view radiographs should be obtained to rule out avulsion fractures and intra-articular injuries. This injury occurs when a flexed DIP joint is suddenly and forcefully hyperextended, leading to rupture of the flexor digitorum profundus tendon. This is most commonly seen in contact sports, such as American football and rugby, when an athlete’s finger catches on another player’s jersey [7]. The ring finger is involved in 75 % of jersey finger cases [8] (Fig. 4.17).
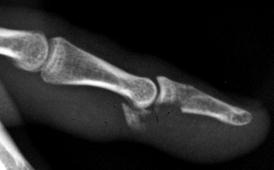
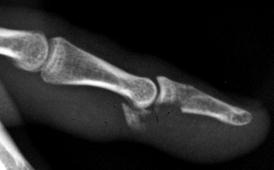
Fig. 4.17
A 24-year-old rugby player injured his middle finger during game. Lateral radiograph demonstrates avulsion fracture from the base of the distal phalanx
4.1.3.4 Central Slip Extensor Tendon Injury
Central slip extensor tendon injuries occur when the PIP joint is forcibly flexed while actively extended or with volar dislocation of the PIP joint. Standard three-view radiographs should be obtained to rule out an avulsion fracture. If the fracture involves more than 30 % of the joint, then orthopedic referral is indicated. In most cases of central slip injuries, the plain radiographs are negative. If there is a delay in treatment, the intact lateral bands of the extensor tendon can slip inferiorly, resulting in a boutonniere deformity [6] (flexion of the PIP joint with hyperextension of the DIP and MCP joints) (Fig. 4.18).


Fig. 4.18
A 25-year-old who sustained a central slip extensor tendon injury. Lateral radiograph shows the boutonniere deformity with flexion at the PIP joint and hyperextension at the DIP and MCP joints
4.1.3.5 Gamekeeper’s Thumb
A gamekeeper’s thumb (skier’s thumb) occurs when there is forced abduction and hyperextension of the thumb resulting in injury to ulnar collateral ligament of the first metacarpophalangeal joint. In a suspected gamekeeper’s thumb, radiographs should be obtained to exclude fracture, prior to performing a stress test (Fig. 4.19). If there is a bony fragment with greater than 2 mm displacement or involving greater than 10–20 % of the articular surface, orthopedic referral is indicated [9]. Unless there is an associated bony avulsion, the injury will be radiographically occult. In these cases, a stress examination with manual abduction may show subluxation compared to the contralateral uninjured thumb [10]. However, there is a theoretical risk of converting a nondisplaced ulnar collateral ligament tear into a displaced one as a result of a stress examination [11, 12]. Among skiers, the frequency of thumb injuries is second only to knee injuries [13].
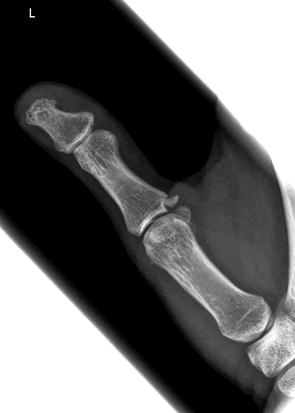
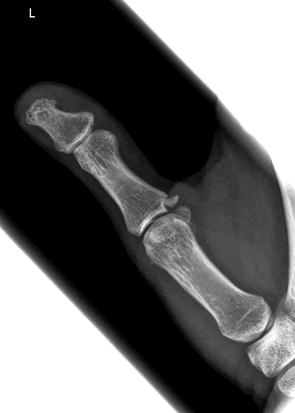
Fig. 4.19
A 28-year-old female skier who injured her thumb after fall. AP view of the thumb demonstrates avulsion fracture from the ulnar base of the proximal phalanx
4.1.3.6 Foreign Body
Plain radiographs will also identify the presence of radiopaque foreign bodies. Metallic objects (except aluminum) and all glass foreign bodies are opaque on radiographs (Fig. 4.20). Most plastic and wooden foreign bodies are not opaque on radiographs [14]. It is important that all patients be thoroughly screened for foreign bodies before undergoing an MRI (Fig. 4.21).



Fig. 4.20
Single PA view of the hand demonstrates radiopaque densities in the soft tissues between the third and fourth metacarpals

Fig. 4.21
Single lateral view of the digit demonstrates a silastic band implant placed during the first stage of flexor tendon reconstruction
4.1.3.7 Role of Radiography After Conservative Treatment
Plain radiographs provide important information when conservative management of fractures or dislocations is indicated. In some clinical scenarios, the operative treatment of fractures is not indicated or possible, and conservative procedures remain the treatment of choice. Plain radiographs are used to check the correction of fracture displacement and for early callus development (Fig. 4.22). They also assess for proper alignment following closed reduction.


Fig. 4.22
26 year-old male who fracture his fourth metacarpal 8 months ago and elected conservative therapy. Single oblique view of the hand (a) demonstrates healed fracture deformity of the fourth metacarpal (malunion). Single intraoperative view (b) demonstrates malunion takedown and fixation with plate and screws
4.1.3.8 Intraoperative and Postoperative Setting
Intraoperative fluoroscopy and postoperative X-rays provide valuable information to the surgeon both during operative stabilization of fractures-dislocations and in the postoperative setting. Surgeons rely on imaging to check the placement of hardware and bony alignment.
4.1.4 Role of Radiography in the Setting of Chronic Finger Trauma
As in the acute setting, radiographs provide important diagnostic information in the setting of chronic finger injury. Again, the standard three-view radiographic examination of the affected digit will reveal significant information to the treating physician, and most physicians agree that imaging evaluation should begin with radiographs. This simple, relatively inexpensive study could be enough to establish a specific diagnosis of arthritis, complications such as infection, nonunion, or malunion.
Imaging plays an important role in evaluating the postoperative patient. Although assessment of hardware can involve a multimodality approach, plain radiographs remain the most commonly used modality. The accessibility, cost, relatively low radiation dose compared with computed tomography, and the provision of positional information are all factors influencing radiography’s utility. In the postoperative setting, plain radiographs allow for evaluation of common postoperative complications, including infection, hardware failure, and incomplete fusion.
Listed below are examples of how plain radiography plays an important role in the setting of chronic finger trauma.
4.1.4.1 Nonunion and Malunion
In addition to the clinical examination, radiographs are important to assess for nonunion or malunion.
Malunion is a frequently encountered complication in hand fractures [15]. Malunion fractures are those that heal with a deformity of angulation, rotation, or overriding of the fragments. This is caused by failure to reduce the fragments into proper alignment or failure to hold them in position until union.
Nonunion occurs when the healing process is incomplete and stops around 6–9 months with no possibility of complete healing; however, it is extremely unusual to achieve nonunion in the metacarpals and phalanges. There are two types of nonunion: atrophic and hypertrophic. The overwhelming majority of nonunions in the hand are of the atrophic type. Radiographically, there is sclerosis of the fracture surface and closure of the medullary canal in the hypertrophic type. There is osteoporosis and tapering of fracture ends in the atrophic type.
4.1.4.2 Infection
Infection may be a complication seen following finger trauma. The diagnosis of osteomyelitis is based primarily on clinical findings, with data from the initial history, physical examination, and laboratory tests serving as benchmarks against which treatment response is measured [16]. Plain radiography is the primary initial diagnostic study.
Radiographic evidence of bone destruction by osteomyelitis may not appear until approximately 2 weeks after the onset of infection. The radiographs may reveal osteolysis, periosteal reaction, and sequestra (segments of necrotic bone separated from living bone by granulation tissue) [17].
4.1.4.3 Posttraumatic Osteoarthritis
Posttraumatic osteoarthritis occurs when the joint surface wears away following an injury to the joint cartilage. Most commonly, this occurs when the fracture involves the cartilage surface of the joint. If the fracture extends into the joint surface, the cartilage can become uneven and prone to osteoarthritis. Plain radiography is an excellent modality to assess for joint space loss and osteophyte formation (Fig. 4.23).


Fig. 4.23
A 38-year-old male who had a prior history of injury to his thumb and presents with pain. Single PA Kapandji view nicely demonstrates the osteoarthritic changes with loss of joint space and osteophytosis
4.1.4.4 Unexpected Findings
In addition to helping evaluate the clinical concern, radiographs may reveal unexpected findings. These findings may include arthritides, congenital malformations or tumor (Fig. 4.24).


Fig. 4.24
A 17-year-old male table tennis player who injured his thumb. Single view did not reveal a fracture, however revealed a triphalangeal thumb and pseudoarticulation between the scaphoid and trapezium
4.1.5 Radiography of the Finger in the Pediatric Population
Hand and wrist injuries are common in the pediatric population, in part due to skeletal immaturity. Early recognition and accurate diagnosis is important to achieve a satisfactory outcome. This depends on a thorough history, good physical examination, and adequate radiographic imaging. As in the adult population, the standard three-view examination of the affected digit is recommended for accurate assessment.
In the pediatric population, most finger injuries can be treated nonoperatively; however, several fractures require prompt surgical intervention. These include Seymour fractures (open Salter I or II fractures of the distal phalanx physis) and injuries with residual deformity, intra-articular extension, displacement, and unacceptable alignment [18]. A poorly treated injury can have significant functional consequences and may result in chronic pain, stiffness, or deformity.
Salter-Harris fractures are injuries through a growth plate and, therefore, unique to pediatric patients. The growth plate is an area of weakness and can be damaged by either chronic repetitive trauma or a single acute high-energy injury event. These fractures are categorized according to the involvement of the physis, metaphysis, and epiphysis and known as the Salter-Harris classification (Fig. 4.25). The classification of the injuries is important because it dictates patient treatment and provides clues to possible long-term complications. Plain films help accurately classify the fractures (Fig. 4.26). The Salter-Harris classification is as follows:
Fig. 4.25




Salter-Harris fracture classification. (a) Metaphysis. (b) Physis. (c) Epiphysis (G. Chick © 2012, all rights reserved)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








