Fig. 7.1
Topography and types of the most common metacarpal fractures observed in ball athletes
Fractures of the base are usually minimally displaced owing to the stabilizing proximal intermetacarpal ligaments, intrinsic muscles, and fascia. Careful physical examination is required to rule out malrotation because at this level, a slight malrotation is greatly magnified at the fingertip. Radiographs must be carefully evaluated for intra-articular extension, which when displaced can lead to carpal–metacarpal arthritis.
A relatively uncommon injury at the base of the second metacarpal is an avulsion fracture of the extensor carpi radialis longus. This fracture is the result of forced flexion of the wrist with simultaneous extension of the arm [8].
The fractures of the fifth metacarpal base are pathomechanically similar to the Bennett fracture of the first metacarpal base. These fractures can be the result of either direct trauma to the metacarpal base or as a result of an indirect trauma as striking a hard object with a firmly clenched fist. Sometimes the fracture of the base of the metacarpal is associated with luxation of one or more neighboring carpal–metacarpal joint and could be misdiagnosed (Fig. 7.2).


Fig. 7.2
Left: displaced intra-articular fracture of the fifth metacarpal base (reverse Bennett). Center: closed reduction and percutaneous pinning. Right: radiographic control 5 years after surgery
Fractures of the shaft may be transverse, oblique or spiral, and comminuted. Fall on the hand, crushing, shots, and tackles, which occur in contact sports, are common mechanisms reported by patients [1]. Oblique and comminuted fractures are more likely to result in metacarpal shortening than transverse and spiral fractures.
Fractures of the distal metaphysis are the most frequent and affect the neck of the fourth and fifth metacarpal. These are most commonly seen in young males involved in activities of punching, although true boxers rarely sustain this injury [9]. The fracture typically has a dorsal apex angulation and is inherently unstable secondary to the deforming muscle forces and a frequent volar comminution [1].
Head fractures are typically intra-articular and caused by significant axial loading.
Open metacarpal neck/head fractures can present insidiously from a fight-bite injury in which the pugilist ignores the wound for several days. When the patient finally appears in the emergency room with a purulent infection, operative incision and drainage must be performed. Care must be taken to retrace the route of the puncture because the fingers are typically flexed during the injury and extended in the operating room. Therefore, the level of injury is actually different within the subcutaneous, tendons, and joint levels.
Metacarpal fractures in ball-sport athletes affect generally one or two metacarpals and are caused by low-energy trauma. Most frequent type is oblique shaft fractures, followed by shaft and neck fractures with transversal fracture line. Less seen are fractures of the metacarpal base and of the head. Comminuted fractures and open fractures with large soft tissue injury are unusual.
7.1.1.5 Nonoperative Management
Allowed Parameters of Displacement
Fracture stability is a function of fracture configuration, periosteal disruption, muscle forces acting at the fracture site, and additional external forces, such as impact in contact sports. Instability frequently parallels the amount of fracture displacement. Shortening, angulation, and rotation may occur independently or in some combination. The instability can be further complicated in the case of multiple metacarpal fractures [10].
When a single metacarpal is fractured, metacarpal shortening is usually limited to less than 4 mm by intermetacarpal ligaments [11]. Approximately 7° of extensor lag occurs for each 2 mm of residual metacarpal shortening after fracture healing. As extrinsic digital extensor tendons can normally slightly hyperextend the metacarpophalangeal joint; fingers with metacarpal shortening up to 4 mm can maintain complete or near complete metacarpophalangeal joint extension [12].
Metacarpal shaft fractures tend to angulate dorsally because of the unbalanced forces of the extrinsic muscles and extrinsic flexor tendons that tend to flex the distal fragment. The closer the fracture is to the metacarpophalangeal joint, the less obvious the amount of angulation in clinical and radiologic evaluation. Measurement on lateral X-ray may be enough to define the precise amount of angulation [10].
The second and third carpometacarpal joints are rigid, with limited mobility; they form the fixed unit of the hand that is why most authors agree that angular deformities in these metacarpals should not be allowed to exceed 10° in sagittal plane [13].
The fourth and fifth carpometacarpal joints have a mobility of 15 and 30° of flexion/extension, respectively. It means that it is possible to compensate certain angular deformities. This fact has created controversy over the degree of acceptable angulation deformity allowed in these metacarpals. In the extreme case of boxer’s fracture, depending on the authors, from 20 to 70° may be admitted as an acceptable angulation of the fragments. Ali et al. [14], in a biomechanical study in 1999, concluded that 30° was the highest permissible limit of final angulation. Above this, angulation may interfere with normal dynamics tension of intrinsic muscle and begin to cause weakness, loss of endurance, cramping, or clawing, as well as altered dorsal knuckle contour.
The metacarpals may tolerate 10–15° of lateral angulation in the frontal plane and still avoid impingement on an adjacent finger during synchronous flexion. The lateral angular deformity of the metacarpal and its effects may be seen best with the fingers in full extension [10].
The rotational deformity, most commonly seen in oblique and spiral fractures, is poorly tolerated. The border metacarpals (of the index and small fingers) are more likely to became rotated and shortened because they do not have the suspensory effect of adjacent intermetacarpal ligaments acting as supports on both sides. A small amount of rotational deformity may be unnoticed with the fingers extended, whereas it may cause impingement and overlapping when they are flexed to make a fist because this tightens the collateral ligaments of the metacarpophalangeal joint.
Each degree of metacarpal fracture rotation corresponds to approximately 5° of rotational deformity at the fingertips [15]. Rotational deformity is suspected when a gap is seen between the fragments of an oblique or spiral fracture on a frontal view. The oblique fracture configuration is unstable by nature, but real instability only occurs if periosteal disruption is substantial enough to allow fracture displacement.
Technique
Initially dorsal and volar splints, in intrinsic plus position that includes all fingers, are the most effective method of immobilization. This is followed by an Orthoplast splint including only the one affected digit and a neighboring one at 2 weeks and then buddy taping and active motion at 4 weeks after injury.
Three to 4 weeks of immobilization are typically required to generate enough healing for initiation of motion, and thus, in this time, it could lead to stiffness due to adhesion formation. Clinical healing, as always, is based on absence of tenderness. The fracture callus may not be visible on X-ray auntil 4–6 weeks after injury. Persistent stiffness of the joint may result from closed reduction and immobilization, but this does not necessarily overrule the advantages of being a low-cost and noninvasive treatment to the patient (Fig. 7.3).
Fig. 7.3
(a) Rotational deformity of the index 1 month after plaster removal. (b) Fracture of the second metacarpal head and of the proximal phalanx shaft
Nondisplaced fractures of the index and middle fingers and minimally displaced fractures of ring and small metacarpals can be treated by external immobilization alone. Fractures that require reduction are difficult to maintain with external immobilization alone, but this may be attempted.
The closed reduction maneuver for neck fractures was described by Jahss [16], in 1938. The reduction is achieved first by disimpacting the fracture by digital traction. The metacarpophalangeal and the interphalangeal joints are then both fully flexed. Dorsally directed pressure is applied axially along the shaft of the proximal phalanx through the flexed metacarpophalangeal joint, and volarly directed pressure is supplied by another digit placed directly over the dorsal apex of the fracture. This takes advantage of the tightness of the metacarpophalangeal collateral ligaments in flexion, which stabilizes the loose metacarpal head fragment.
The fracture should never be immobilized in the Jahss position, as significant interphalangeal joint contractures will ensue. It is immobilized with a short-arm gutter splint with the fingers in the safe position and the wrist in neutral to tighten the dorsal extension mechanism to act as a tension band. The splint is continued for 14 days, followed by active motion with buddy taping to an adjacent digit.
Fractures of the head with minimal to no displacement can be treated by splinting in the intrinsic plus position, but this is an uncommon presentation for this injury [13].
Recommendation for Ball Athletes
Conservative treatment may be recommended in ball athletes only when there is no or minimal displacement, and the fracture is stable. In athletes, we have to be more demanding than in the normal population; they present three major problems with this treatment: (1) the prolonged recovery time, as the physiotherapy cannot begin until immobilization is removed; (2) malunion is poorly tolerated by athletes; and (3) the stiffness that may occur may have implications on their future careers.
In stress fractures, the only effective solution is to discontinue play or to protect the hand from impact until symptoms resolve [10].
7.1.1.6 Surgical Management
Surgical Options
The percutaneous fixation with Kirchner wires is a useful technique that is relatively easy to perform and useful in many types of fractures (unstable neck, long oblique). These are typically crossed or inserted in parallel. The transfixion wires should be inserted with the metacarpophalangeal joints flexed to prevent intrinsic muscle tightness. Two wires are necessary distal to the fracture site. This prevents rotation to the distal fragment on a single wire. However, Kirschner wires do not provide truly rigid fixation, and a period of immobilization must always follow to avoid loss of reduction. Infection at the entrance of the pins may be another problem, when they are left outside the skin. That is why many surgeons leave them buried under the skin, and these are removed after fracture healing (4 weeks or more), in the clinic setting. Nevertheless, many studies have published excellent results with minimal complications for metacarpal fractures fixed with Kirschner wires [17] (Figs. 7.4 and 7.5).



Fig. 7.4
Fractures of the second metacarpal head and the fifth metacarpal shaft: (a) PA view (b) oblique view. Different types of fixation: plate fixation, adjacent metacarpal K-wire fixation, intramedullary pin fixation. (c) Lateral view (d) PA view

Fig. 7.5
Spiral fracture of the fourth metacarpal with established malunion, despite the presence of a single metacarpal fracture. This complication could be avoided by performing a simple percutaneous K-wire fixation
Intramedullary fixation of the metacarpal is another technique described for transverse and short oblique fractures [18]. Although this technique was not very common, there is an increasing number of publications with very good results [19–21].
This technique uses a small incision at the base of the metacarpal and then an awl to create a window in the metacarpal cortex, through which a single central large wire (1.6 mm) or several small wires (0.8 a 1 mm) are inserted. Some authors leave the ends of the wires buried in the metacarpal bone to prevent irritation of the soft tissues. However, they do not provide a rigid fixation or compression and contribute little to control of rotation at the fracture site, which is why there is some debate as to initiating mobilization immediately or after 2–3 weeks of cast immobilization. Intramedullary K-wires is more frequently used in diaphysis and neck fractures of the fourth and fifth metacarpal bones [22, 23].
Tension band wiring also provides relatively rigid fixation and is not as bulky as plate fixation. However, it requires extensive dissection and is not as stable as fixation with plate and screws; that is why most hand surgeons do not perform this technique frequently [13].
Interfragmentary screws are useful in long oblique fractures (at least twice the diameter of the bone) and for capturing large isolated intra-articular fragments. Some studies have demonstrated that fixation with two lag screws provides greater rigidity than either crossed Kirschner wire or dorsal plating [24]. This fact allows for early motion of the fingers, thereby avoiding the postoperative stiffness that often characterizes the use of Kirschner wires. Screw fixation, however, is technically demanding and leaves little margin for error. The surgeon usually gets only one shot with screw fixation [13].
A plate and screws provides a rigid fixation, which permits early mobilization, similar to screw fixation. Due to its buttress support, plate fixation is ideal for comminuted fractures [25]. However, plates require extensive dissection to provide adequate exposure, which could result in extensor lag, and even if we use low-profile plate, prominence of the plate could be a problem. Plate fixation, similar to screws fixation, is technically demanding and, according to many studies, fraught with complications such as contractures, extensor lag, infection, tendon rupture, plate prominence, plate loosening or breakage, and unsightly dorsal scars [26, 27]. Most studies have shown approximately 220° of total active motion after plate fixation, with complication rates approaching 20 % [25].
Bioabsorbable miniplating, although it appears to offer the same resistance to hold the fracture in the beginning and can obtain good healing of the fracture, poses the problem of foreign body reaction, which can cause long-term complications, with follow-up needed at least two years after implant placement [28].
External fixation is another tool that has been used in open fractures and those involving segmental bone loss and or infection. This method avoids extensive dissection and leaves periosteum over fracture fragments to promote healing. As in Kirschner wires, pin entry site is a possibility, and the bulky fixation unit can be bothersome to patients. Other potential complications include osteomyelitis, loosening of the pins, fracture through the pin sites, and damage to the extensor tendons [29].
Bone grafting can be useful for obtaining adequate reduction and greatly accelerating healing in high-energy injuries. Cancellous grafts can be obtained from the distal radius or iliac crest; allografting may be considered. Bone grafting has been classically used in secondary reconstruction procedures for complex injuries, but it has gradually gained acceptance for use in primary surgical procedures, with very good results, no infections, and return to original work for all patients as in the series published Saint-Cyr and Gupta [30] in 2006.
Recommendation for Ball Athletes
As explained above, when making the surgical decision, we must take into account that these fractures are often one unique metacarpal fracture without major soft tissue injuries and without much displacement [1, 4].
Metacarpal Base Fractures
In the second and third metacarpal when displacement is minimal, early return to sports is allowed with a short-arm splint that holds the metacarpophalangeal joints in flexion and keeps the interphalangeal joints free [1].
While there is no consensus for the treatment if significant displacement or instability is present, there is a tendency to favor operative treatment, with percutaneous Kirschner wires that can reach into the carpus, lag screws, or even plate and screws [31].
In avulsion fractures, although reestablishment of the joint surface might not prove vital, due to the relative immobility of the second carpal–metacarpal joint, surgical treatment is recommended on the grounds that the extensor carpi radialis longus insertion should be restored for optimal stability during gripping and that a displaced or rotated fracture fragment could impinge upon nearby uninjured tendons and lead to secondary irritation or even rupture [8].
The management of fractures in the base of the fourth and fifth metacarpals remains a continuous topic because multiple reports in the literature reveal that regardless of the choice of surgical versus nonsurgical management, approximately 40 % of these patients will likely experience long-term pain [31] (Fig. 7.6).


Fig. 7.6
Top: fracture of the fourth metacarpal base with dislocation of the fifth carpometacarpal joint. Below: plate fixation of the fourth metacarpal base
In case of fracture of the base associated with dislocation of carpometacarpal joint, reduction of the fracture–dislocation and internal fixation with Kirschner wires and/or plate (depending on stability) is compulsory because secondary displacement frequently appears due to deforming forces of the extensor tendons.
Metacarpal Shaft Fractures
The treatment decision in metacarpal shaft fractures is made depending on three factors: fracture configuration (transverse, oblique, or spiral), fragment displacement, and number of metacarpal fractures.
Transverse Fractures
In fractures of only one metacarpal, our choice is the fixation technique described by Orbay, in 2005, for transverse fractures and short oblique. The fracture is fixed with only one thick antegrade intramedullary wire and another locking pin to a neighboring metacarpal.
Open reduction and internal fixation with plates is reserved for multiple closed metacarpal fractures and most not highly contaminated open fractures. Kirschner wires alone are inadequate to provide sufficient rigidity to begin early motion. Nevertheless, we must not forget the aforementioned major complications of plates [26, 27].
Oblique and Spiral
Isolated minimally displaced metacarpal fractures (less than 4 mm of shortening and less than 10° of angulation in any direction) can be treated orthopedically [1]. If reduction can be obtained but not maintained, percutaneous pinning techniques are used to hold reduction [32]. If acceptable reduction cannot be obtained, open reduction is required. Our opinion is to use lag screws only in oblique fractures with a long fracture line (at least twice the diameter of the bone) and never less than three screws; if not, fixation should be with plate and screws.
When we have to treat a patient with two or more displaced metacarpal fractures, regardless of the reduction potential and the type of fracture, treatment should be surgical, using the most stabilizing osteosynthesis possible, most times it will be plate and screws (Fig. 7.7).


Fig. 7.7
Oblique fractures of the third and fourth metacarpals. Radiological evaluation of the hand at 9 years after surgery (plate and screws). Even after a long postoperative period, the hump on the dorsal surface of the hand due to the presence of the plate remains visible
Metacarpal Neck Fractures
Several methods of percutaneous fixation with Kirschner wires are available for these fractures: oblique cross, transverse parallel through to adjacent metacarpals, only one intramedullary thick wire, and several thin intramedullary [17–23]. We prefer an antegrade thick intramedullary Kirschner wire (1.5 mm), slightly curved at the end, supplemented in the event of instability, with another Kirschner wire (1.5 mm) between the metacarpal heads to prevent rotation, if the fracture is unstable. This method also provides sufficient fracture fixation to play sports with the help of a protective splint.
The neck fracture must be opened only in case of soft tissue entrapment, irreducibility, or high-energy trauma. Fixation can then be accomplished with Kirschner wires, tension band wiring, or plate. The 2-mm minicondylar plate is inserted in the dorsal or lateral aspect of the distal metacarpals. The contraindications to its use are an open physis or a distal fragment narrower than 6 mm [33]. If Kirschner wires are used and sporting activities are initiated, the wires should be cut to lie subcutaneously to lessen skin irritation and facilitate application of a protective splint [1].
Metacarpal Head Fractures
Open reduction and internal fixation is required to achieve adequate alignment of the joint surface. We need to be strict with articular fractures, and as a general rule, we must not allow a step-off of more than 1 mm if the fragment involvement is greater than 25 % of the articular surface or is located in a strategic area of joint loading [3].
Operative reduction is achieved through a linear or curvilinear incision dorsally over the metacarpophalangeal joint, with dissection carried down through the sagittal band that should be reflected off the extensor tendon along its ulnar border. The tendon is retracted and a longitudinal incision over the joint capsule used to enter the joint. Hemarthrosis and debris are carefully removed, and the fragments reduced to provide a joint surface as smooth as possible. Bone grafting may aid in the reconstruction of the joint. Small cortical screws can then be used to fix the fragments into place. The wound is irrigated, the sagittal band repaired, and the wound is closed.
7.1.1.7 Post-immobilization Care and Return to Sport
Post-immobilization treatment of fractures of the metacarpals in ball athletes should be guided by the early return to the sport, hence the need to accelerate the recovery process, using physical therapy, magnetic therapy, and electrotherapy combined with protective splints to prevent displacement of the fracture.
When orthopedic treatment is used, rehabilitation of immobilized regions should start 3 weeks after the fracture date, although the fracture callus is not visible and must be intensive to avoid propensity for swelling with tendinous adhesions and joint stiffness.
With a stable or rigid fixation, splint protection is only required at night or for sports. Active use without straining is permitted in 3–5 days. For early competitive play, a functional splint (Galveston) has been developed, which provides free motion of fingers and wrist. The brace, that applies three-point fixation, is adjustable to provide one pad over the dorsal apex of the fracture and two volar pads on either side of the fracture. Skin irritation can be a problem, and patients are instructed to loosen the pressure through the Velcro straps if problems develop [34]. Special gloves and buddy taping of adjacent fingers may cushion impact and dissipate twisting forces and may be added to the treatment regimen, so that hands are protected during play [10] (Fig. 7.8).
Fig. 7.8
Football player treated with buddy taping for a metacarpal fracture
Kirschner wires alone are inadequate at providing sufficient rigidity to begin early motion. If Kirschner wires are used and sports activities are initiated, the wires should be cut to lie subcutaneously to lessen skin irritation and facilitate application of a protective splint [1].
7.1.1.8 Directions for the Future
The pillars on which rests the future of treatment are: stabilization and healing of the fracture and management of injured soft tissue. We agree with Stern [18] in which physicians will be able to biologically manipulate (accelerate the time to fracture union) and they will be able to rapidly stabilize the fracture by direct injection of a substance (organic mineral compound) into the fracture site. The management of soft tissue injury is a more difficult problem and is likely to be the major impediment to full recovery for decades to come. Perhaps improvements and refinements in immunotherapy and allotransplantation of bone and soft tissue parts may provide a future solution.
Key Points
Metacarpal fractures in ball-sports athletes generally affect one or two metacarpals and are caused by low energy trauma.
The most frequent type is oblique shaft fracture, followed by transverse shaft and neck fractures.
The metacarpals may tolerate 10 to 15° of lateral angulation in frontal or sagittal planes, but rotational deformity is poorly tolerated.
Conservative treatment may be recommended in ball athletes only when there is no or minimal fracture displacement and the fracture is stable.
A displaced and unstable fracture may be reduced by open or closed methods, depending on the location and the fracture line.
Surgical techniques include percutaneous or intramedullary fixation with Kirchner wires,interfragmentary screws, rigid fixation with plate and/or screws and external fixation.
Immobilization after treatment of metacarpals fractures in ball athletes should be guided by early return to the sport, hence the need to accelerate the recovery process, using physical therapy.
Suggested Readings
Capo JT, Hastins H II (1998) Metacarpal and phalangeal fractures in athletes. Clin Sports Med 17:1–23
With the increasing demands placed on physical fitness by today’s society and the financial significance of professional athletes’ performance and playing time, the physician may be pressured to alter management of hand fractures in the athlete. A physician may be encouraged to proceed with a more aggressive therapy that will more quickly return an athlete to play, or a player may insist on deferring treatment until after the end of a particular season. The physician should have a variety of methods available to him or her and make treatment decisions that keep the patients overall athletic career and future hand performance in mind. This article deals with the treatment of the most common extra-articular fractures of the metacarpals and phalanges typically seen in athletes and the most effective and straightforward methods that permit rapid and effective return to athletic activity.
Chin SH, Vedder NB (2008) Metacarpal fractures. Plast Reconstr Surg 121:1–13
Metacarpal fractures are the most common injuries seen in the emergency room and a staple in the office of the hand surgeon. The different types of injury patterns must be recognized by the surgeon, and appropriate treatment then executed to serve both the patient and the surgeon optimally. Closed reduction and cast immobilization, Kirschner wires, lag screws, plate fixation, and other techniques are all available to the hand surgeon. Bone grafting in highly comminuted fractures also deserves consideration. The majority of metacarpal fractures can be treated closed and do well with compliant hand therapy. Those fractures requiring operative intervention likewise do well, provided that the appropriate technique is used for the situation. For example, long oblique shaft fractures are optimally treated with lag screws, whereas short oblique do better with plate or Kirschner wires. When the correct therapy is tailored to the injury, most metacarpal fractures can be treated with predictable good results.
Singletary S, Freeland AE, Jarrett ChA (2003) Metacarpal fractures in athletes: treatment, rehabilitation, and safe early return to play. J Hand Ther 16:171–179
When fractures occur, athletes must be protected from contact until healing has progressed to a point where reinjury or complications are unlikely and performance standards and expectations can be met. This article outlines a program of fracture management principles and progressive graduated rehabilitation that phase the hand-injured athlete first into general conditioning and non-ball-handling drills and then into return to hand activities, body contact, ball handling, and catching with the use of protective hand gear. At this point, specialty gloves and buddy taping of adjacent fingers may cushion impact and dissipate twisting forces, and may be added to the treatment regimen, so that hands are protected during play. The importance of the particular sport, the position played, and hand dominance are factored into the decision-making processes.
7.1.2 First Metacarpal Fractures
Carlos Henrique Fernandes3 , Jorge Raduan Neto3, João Baptista Gomes dos Santos3 and Flavio Faloppa3
Abstract
Hand injuries are common in athletes probably because the hand is characteristically in front of the athlete and frequently absorbs the initial contact. These injuries usually result from accidents and are therefore difficult to prevent. Fractures of the first metacarpal occur at all athlete levels, and the initial management is crucial for early return to sports. Thumb fractures result in pain and loss of function, including inability to grip, weakness, and reduced range of motion (ROM). Radiographic assessment of the thumb includes standard posteroanterior (PA), lateral, and oblique views. Thumb metacarpal fractures can be subdivided into distal fractures, fractures of the metacarpal neck, metacarpal shaft fractures, and fractures of the metacarpal base. The fractures that affect the base of the metacarpal are the most frequent. Metacarpal base fractures were first classified by Green and O’Brien in 1972 into four patterns. Type 1 is known as Bennett’s fracture. In 1954, Gedda classified Bennett fractures into 3 types. Type 2 is the Rolando fracture. This fracture has remained the subject of much debate. In our opinion, because of the instability of these fractures and frequent complications, closed reduction and plaster casting is an inappropriate treatment for athletes. In our view, closed reduction and pinning are still the best treatment, and reduction by arthroscopy will improve the results in the future. The extra-articular fractures frequently result in a retraction of the first web, and an open reduction and internal fixation with screws and plate avoids this complication. A pure traumatic dislocation of the first carpometacarpal joint and an injury involving the proximal physis are very rare.
7.1.2.1 Natural History
First metacarpal fractures make up almost 25 % of all metacarpal fractures, and over 80 % of these fractures involve the base of the first metacarpal. The fracture predominates in adult males and usually occurs in the dominant hand. Fractures of the first metacarpals result from rotation, bending, direct blows, indirect forces, or any combination of these forces. Hand injuries are relatively common during sports practice, probably because the hand is characteristically in front of the athlete in most sports and frequently absorbs the initial contact. Fractures of the first metacarpal occur at recreational level or at top athlete level, and initial injury management is crucial. Finger and thumb injuries are common in sports with a high risk of falling, such as skiing, biking, in-line skating, and gymnastics. In many competitive team sports, the thumb is one of the areas most often injured. Football also results in a high percentage of hand and wrist injuries, accounting for 15 % of all injuries. In football, first metacarpal fractures affect mainly the goalkeeper from trauma caused by the ball. Other causes are a fall to the ground and physical contact with other athletes.
On the other hand, finger injuries in volleyball occur mainly during blocking [35].
7.1.2.2 Physical Findings
Patients with thumb injuries classically present with pain and loss of function of the thumb including inability to grip, weak pinch, and reduced range of motion. On inspection, there may be a local swelling, volar, and dorsal ecchymosis (Fig. 7.9). Sometimes the thumb will appear shortened or with an angular deformity. A careful examination will reveal bony crepitus and tenderness to palpation over the first metacarpal.
Fig. 7.9
(a) Palmar ecchymosis (white arrow) and (b) dorsal swelling in a patient with a Bennett fracture
It is also important to remember to appropriately examine trauma patients for any other injuries. A differential diagnosis with injury to the scaphoid, trapezium, or distal radius should be made.
7.1.2.3 Imaging
Imaging should begin with radiographs of the entire hand and should include three views: posteroanterior (PA), lateral, and oblique. Because the thumb sits out of the plane of the rest of the hand and fingers, special radiographic views are necessary for appropriate evaluation. Radiographic assessment of the thumb includes standard posteroanterior (PA), lateral, and oblique views. A true anteroposterior view of the thumb requires that the hand be hyperpronated so that the dorsum of the thumb lies against the radiographic plate (Robert’s view). A true lateral of TM joint (Bett’s view) is where the sesamoids of the thumb MP joint overlap each other. This view can be obtained with the palm on the cassette, and the hand then pronated 15–20° and the tube angled proximally 15°. Both views are helpful when evaluating fracture displacement and joint congruency of TM joint and the three additional articulations of the trapezium with the trapezoid, the scaphoid, and index metacarpal.
Radiographic evaluation of fractures includes the location and direction of the fracture line, the presence or absence of comminution, displacement of the fracture, articular involvement, and associated soft tissue injury. Pay attention to the center of ossification of the base of the metacarpal of the thumb because it unites with the body at about the 20th year.
CT remains the best modality for evaluation of the bony architecture. It is particularly helpful for articular fractures of the head and base that may not be evident on radiographs.
7.1.2.4 Classification
The first metacarpal bone is the shortest and the most mobile. It can be divided into four anatomic regions: a head, a neck, a shaft, and a base (Fig. 7.10). Fractures can be subdivided by these four regions.
Fig. 7.10
First metacarpal bone divided into four anatomical regions: 1 head, 2 neck, 3 shaft, 4 base
The head of the first metacarpal differs from that of the other metacarpals. Fractures are common in the long finger metacarpal but rare in first metacarpal because any longitudinally directed force which might produce this fracture is dissipated at the trapeziometacarpal joint. Distal metacarpal fractures are by definition intra-articular, and most are avulsion fractures with radial collateral ligament injuries. On the other hand, four cases of intra-articular shearing fracture of the radial condyle of the metacarpal head in association with ulnar collateral ligament injury were reported.
Metacarpal neck fractures usually result from direct trauma. The fracture occurs just below the metacarpal head, which is displaced in a volar direction (Fig. 7.11). Injuries such as this commonly occur in throwing athletes, when the thumb strikes an object with a ball.
Fig. 7.11
Metacarpal neck fracture: the importance of two views. (a) In posteroanterior view, it is not possible to see the displacement of distal fragment. (b) In the lateral view, the distal fragment is seen deviated
Metacarpal shaft fractures are uncommon sports injuries. These fractures usually occur at the metaphyseal–diaphyseal junction and are referred to as epibasal fractures. The fragments are typically displaced with an apex dorsal angulation. The distal fragment is deviated in supination, flexion, and adduction, per share of adductor pollicis, flexor pollicis brevis, and abductor pollicis brevis. The proximal fragment is deflected by the action of the abductor pollicis longus.
The first metacarpal base fractures are classified by Green and O’Brien [36] into four patterns (Fig. 7.12). Types 1 and 2 are intra-articular fractures and types 3 and 4 are extra-articular. Type 1 is the Bennett fracture. It is a fracture–dislocation of the base of the metacarpal. Type 2 is Rolando fracture, a comminuted version of type 1 fracture. Type 3 fracture is either transverse or, less commonly, oblique. Type 4 fracture is an injury involving the proximal physis.
Fig. 7.12
Classification of Green and O’Brien: type 1 Bennett fracture, type 2 Rolando fracture, type 3 extra-articular fracture (3a: transverse fracture, 3b: oblique fracture), type 4 proximal physis fracture
Type 1 (Green and O’Brien)
This is the most common type. Edward H. Bennett was the first author to describe this fracture of the volar, ulnar portion of the proximal aspect of the thumb metacarpal in 1882. From this early account, this fracture pattern now carries his name.
With these fractures, the small proximal and ulnar fragment of the first metacarpal continues to articulate with the trapezium via the volar ligament. The distal aspect of the metacarpal is supinated and dislocated radially by the adductor pollicis, whereas the abductor pollicis longus, inserted on a radial tubercle of the base, pulls the shaft fragment in a dorsal, radial, and proximal direction. The abductor pollicis longus also imparts some supination to the shaft of the thumb metacarpal. This muscular action results in a dislocation of the first carpometacarpal joint.
Gedda [37] classified Bennett fractures into 3 types (Fig. 7.13), with type 1 representing a fracture with a large single ulnar fragment and subluxation of the metacarpal base. A type 2 fracture represents an impaction fracture without subluxation of the thumb metacarpal. Finally, a type 3 fracture represents an injury with a small ulnar avulsion fragment in association with metacarpal dislocation.
Fig. 7.13
Gedda’s classification for Bennett fractures: type 1: fracture with a large single ulnar fragment and subluxation of the metacarpal base, type 2: impaction fracture without subluxation of the thumb metacarpal, type 3: small ulnar avulsion fragment in association with metacarpal dislocation
Type 2 (Green and O’Brien)
The type 2 is the Rolando fracture. It is a specific tripartite intra-articular fracture of the base of the thumb metacarpal in which the fragments may form a T or Y pattern. They include the palmar and ulnar Bennett fragment in addition to a dorsal radial fragment at the base of the first metacarpal (Fig. 7.14). However, the term has since been used to describe any comminuted intra-articular fracture of the base of the first metacarpal.
Fig. 7.14
Rolando fracture, open reduction and internal fixation with screws and plate. (a) PA view (b) lateral view (c) surgical approach (d) internal fixation (e) lateral view after internal fixation
Type 3 (Green and O’Brien)
Extra-articular fractures of the first metacarpal base are less more serious than those occurring in the metacarpal bones of long fingers. There are two types: transverse fracture or, less commonly, oblique fracture (Fig. 7.15).
Fig. 7.15
Type 3 of Green and O’Brien, (a) a transverse fracture and (b) an oblique fracture
Type 4 (Green and O’Brien)
This fracture is an injury involving the proximal physis. Rang and O’Brien classified in three types. Group A corresponds to pure metaphyseal fractures, group B to Salter–Harris type II injuries with a metaphyseal fragment at the medial metaphyso-epiphyseal angle, and group C to Salter–Harris type II injuries with the metaphyseal fragment at the lateral metaphyso-epiphyseal angle.
A pure traumatic dislocation of the first carpometacarpal joint is very rare, compared to Bennett fracture. The treatment for thumb carpometacarpal joint dislocations will be analyzed in a different chapter.
7.1.2.5 Nonoperative Management
In metacarpal neck fractures, casting or splinting for 3 weeks is helpful to avoid further instability and to promote healing with stability at the fracture site.
Due to the compensatory motion of the trapeziometacarpal joint, some displacement and angulation can be tolerated in the thumb metacarpal shaft fracture. These cases can be treated conservatively.
Since its first description, the treatment of Bennett’s fracture has remained the subject of much debate. Biomechanical studies noted that 2 mm of residual displacement at the articular surface resulted in an overall increase in contact area at the TM joint, with a dorsal shift in contact pressures over the trapezial surface. The authors concluded that a 2-mm articular step-off is acceptable and should be well tolerated as long as the metacarpal was reduced [38].
The treatment of Rolando’s fracture depends on the severity of comminution of the fragments and the degree of displacement. The methods of treatment suggested are soft dressing with early motion, closed reduction and casting, closed reduction and percutaneous Kirschner wire fixation, and oblique traction. The two first described methods are unacceptable in athletes.
The conservative treatment is recommended in type 3 fractures if there is no displacement. The thumb is immobilized for 6 weeks.
The treatment in type 4 fractures is nonoperative, consisting of closed reduction and application of a thumb spica cast including the entire first ray.
7.1.2.6 Surgical Management
Displaced intra-articular fractures of the metacarpal head often require open reduction and internal fixation, particularly if an articular step-off is present. In malunited intra-articular fractures of the metacarpal head, an intra-articular osteotomy and rigid internal fixation was described with significant improvement in the articular anatomy and function. In failed cases, the arthrodesis of the first metacarpal phalangeal joint after fixation with a low-profile titanium plate, using a cup-and-cone technique, gives a high rate of union, a short period of immobilization and rehabilitation, and a reliable position at the site of fusion.
Metacarpal neck fractures that are markedly comminuted or angulated may occasionally require open reduction and internal fixation with Kirschner wires or screw and plates. A plaster cast immobilization is used by for 3 weeks.
Metacarpal shaft fracture with angulation greater than 30° is an indication for reduction. Closed reduction may be accomplished through axial traction, extension, and pronation with direct pressure over the fracture dorsally and skeletal fixation with percutaneous pins. Open reduction and internal fixation with plates and screws is reserved for high-energy trauma, irreducible fracture, fracture with excessive angulation, or multiple fractures. It can be performed through a dorsal longitudinal incision. Careful blunt dissection should be performed to preserve the terminal branches of the superficial radial nerve and radial artery. For adequate exposure of the first metacarpal, the extensor pollicis longus is retracted to the ulnar side and the extensor pollicis brevis to the radial side.
The closed reduction technique for treatment of Bennett’s fracture was described by Wagner. It can be done under adequate analgesia. It involves axial traction on the thumb to pull the metacarpal distally, palmar abduction, and pronation while applying external pressure, with the thumb pulp over the metacarpal base medially to return it to its anatomical position. To hold the reduction, a Kirschner wire is placed through of the metacarpal across the joint and into the trapezium. Subsequently, to prevent shortening and adduction of the thumb, another K-wire with a diameter of 1.5–2 mm is inserted between the metacarpal diaphysis of the thumb and the index finger. Closed reduction and percutaneous fixation with intermetacarpal Kirschner wires can be used. The K-wires are positioned approximately 2 cm apart, through the first metacarpal with a 90° angle and also through the second metacarpal. Edmunds [39] wrote that this practice using the hitchhiker position (to take the pull off the abductor pollicis longus) is based on the myth that the abductor pollicis longus is a deforming force in a Bennett fracture. He considers it to be a grossly incorrect reduction technique. He recommends the passive screw-home-torque technique method of reduction in which the surgeon places the patient’s trapeziometacarpal joint into a full passive opposition and then torques the thumb metacarpal into maximum passive screw-home-torque, such that the plane of the thumb tip pulp is rotated opposite the pulp of the index and long digits in the three-jaw chuck power pinch position. This technique can be performed closed for percutaneous fixation, or it can be performed open with a K-wire in the metacarpal as a “twisting joystick” to aid in the torque before internal fixation of the Bennett fracture. When the proximal fragment is too big, we prefer fixation with a percutaneous cannulated screw.
Open reduction and internal fixation should be considered when the fracture is irreducible or where greater than 2 mm of articular step-off persists despite closed reduction attempts or a Kirschner wire cannot be passed across the fracture into uninjured bone at the base of the thumb.
The open reduction of the metacarpal is performed through a Wagner incision. The incision is made at the junction of the volar skin and dorsal skin over the trapezoid–metacarpal joint. Careful blunt dissection should be performed to preserve the terminal branches of the superficial radial nerve and radial artery. The extraperiosteal elevation of thenar muscles is performed to permit exposure of fracture site. The choice of fixation technique depends on the size of the fragment. If the base length of the fragment is greater than 25 % of the length of the first metacarpal base, we can choose the compression screw fixation. If less than 25 %, we should use Kirschner wires.
The decision for open reduction, as opposed to closed reduction and pinning, is still a matter of debate. Lutz et al. [40] studied 32 patients with a Bennett’s fracture who were treated either by open reduction and internal fixation or closed reduction and percutaneous transarticular Kirschner wiring. After a mean follow-up of 7 years, they found that the type of treatment did not influence the clinical outcome or the prevalence of radiological posttraumatic arthritis. The percutaneous group had a significantly higher incidence of adduction deformity of the first metacarpal. This however did not result in an inferior outcome.
On the other hand, Capo et al. [41] showed significant discrepancies in step-off and displacement measurements between fluoroscopic examination and open visualization and in displacement values between radiographic and direct visualization. They recommend open reduction and internal fixation if the reduction is deemed unsatisfactory and if any doubt exists about the residual articular malalignment.
To avoid these problems, the visualization of reduction by arthroscopy is advocated by Culp and Johnson [42]. The surgical technique is not difficult if the surgeon is familiar with the arthroscopic technique and appropriate instruments are available. The patient is placed supine on the operating table under general or regional anesthesia. A single finger trap is applied to the thumb, and 4.5 kg of traction is applied using a traction tower. The 1-radial portal is established just radial to the abductor pollicis longus tendon at the level of the carpometacarpal joint. The 1-ulnar portal is located just ulnar to the extensor pollicis brevis, again at the level of the trapeziometacarpal joint. An 18-gauge needle is inserted into 1-radial portal, and the carpometacarpal joint is inflated with 2–3 ml of normal saline to distend the joint. A small incision centered over the carpometacarpal joint at the 1-radial portal is made, and a small, curved hemostat is used to spread the subcutaneous tissue. After this, the trocar and sleeve are inserted, then the trocar is removed, and the 1.9-mm arthroscope is inserted. The 1-ulnar portal is then established by same steps for 1-radial portal. A 2.0-mm shaver may be used to remove any frayed tissue or cartilaginous fragments. Once the joint is clearly visualized, the fragment is then manipulated using the intra-articular probe, adjustments in traction, and 1.5-mm Kirschner wires. Usually, the metacarpal shaft fragment is extended and supinated. This may be accurately reduced using Kirschner wires as joysticks. Once reduction of the fragment is obtained, fixation is completed using either Kirschner wires or 1- or 1.5-mm screws. A bulky dressing and forearm-based thumb spica splint are applied after portal sites are closed using 4–0 nylon simple sutures.
Fig. 7.16
The simultaneous Bennett fracture and trapezium treated by open reduction and internal fixation with a lag screw. (a) PA view and (b) PA view after ORIF
Cases of simultaneous Bennett’s fracture and trapezium are reported [43] in which open reduction and internal fixation was required to stabilize an unstable first carpometacarpal joint with simultaneous fracture of the trapezium and Bennett’s fracture. The results were good in terms of range of movement and radiological appearance, all of them returning to normal activities, including heavy manual work. We have six unpublished cases (Fig. 7.16). No patient required further surgery.
The Rolando fractures are quite difficult to treat but, fortunately, are a rare type of first metacarpal fracture. When the two fragments are large, without considerable comminution, open reduction and internal fixation with Kirschner wires or lag screws placed through a Y, T, or L plate may be attempted. Again we preferred the Wagner incision.
However, if there is severe comminution, distraction and reliance on ligamentous reduction of the fragments may be necessary, but the treatment of choice is controversial because attempts at operative restoration of the articular surface are frustrating, if not impossible, with ligamentotaxis alone.
Distraction can be achieved with oblique traction pinning, but this method was bulky, required a long period of fixation, and decreased the range of motion. Closed reduction and percutaneous Kirschner wires were used, but the results were satisfactory.
Alternatively, the fracture can be spanned and distracted using external fixation with different configurations described. The use of external fixation for Rolando fracture provides several advantages to alternative techniques for fixation, including ease of insertion with minimal dissection and devascularization of soft tissue and bone, and preservation of bony length.
In cases of displacement, surgical treatment is indicated in type 3 fractures. Internal fixation is performed with intramedullary pinning or intermetacarpal K-wires. These techniques usually require postoperative immobilization for 6 weeks.
Internal reduction should be done via dorsal approach. A Y, T or L plate is placed on the dorsal aspect or lateral edge of the first metacarpal (Fig. 7.17). Careful closure of the periosteum is carried out to protect the extensor system. Skin is closed without a drain. Diaconu et al. [44] reported that T-shaped plates do not provide sufficient strength to allow early mobilization of the thumb after fixation. They thus recommend the use of double-row plates.


Fig. 7.17
Extra-articular base fracture of first metacarpal treated by internal fixation with a T plate
Unstable type 4 fractures require K-wire stabilization of the first and second metacarpals across the first web using Iselin’s technique and application of a cast including the thumb.
7.1.2.7 Postoperative Care
If secure internal fixation can be achieved, early motion may be initiated in intra-articular fractures of the metacarpal head.
Open reduction and internal fixation of metacarpal shaft fractures restores structural integrity so that early return to sports with a protective splint is often possible. Swelling can be controlled with massage, proper elevation, icing immediately after therapy, and compression gloves. Digital and wrist tenodesis and individual joint-blocking exercises are excellent nonresistive exercises to regain maximum ROM in all joints [45].
In the Wagner technique, a plaster cast immobilization is used by for 4 weeks. Rehabilitation involves early active and passive mobilization of interphalangeal joints. After Kirschner wires are removed, mobilization of carpometacarpal joint is started. Mobilization is early with internal fixation as well. Resistive exercises for strengthening thumb intrinsic and extrinsic muscles, pinch and grip, weight bearing on the palm with thumb in radial abduction, and return to usual routines without a hand-based opponens splint should be considered only when there is evidence of stable fracture healing. Progressive training to full return can be expected at around 4–6 weeks or when the fracture is nontender and shows radiological evidence of union.
In type 3 fractures with internal fixation with plate and screws, the first web is immobilized in a splint for 3 weeks, followed by hand therapy.
7.1.2.8 Outcomes and Return to Sport
Unfortunately, the management of injuries of the thumb in a recreational or professional sports team is sometimes not the best and often leads to detrimental consequences for ball-sport practice.
The estimate for an athlete’s return to sports should be as fast as possible. Surgery may be necessary to reach these goals for athletes because of the demands of their sport. Even with miniplate fixation, the fracture needs protection until there is evidence of healing by fracture callus on X-ray or resolution of local signs of injury on clinical examination. Although many manual laborers who are injured at work are reluctant to return until they are fully healed and pain-free, athletes are different. The desires and motivation of the player, coaches, and parents may pressure the physician to return the patient to play more quickly than is safely possible. Preventing a sports-related hand injury may not always be possible, but there are steps to reduce their impact if they do occur.
7.1.2.9 Complications
Locked metacarpophalangeal joint due to an intra-articular fracture of the metacarpal head was described.
A malunion of a metacarpal shaft fracture will result in compensatory hyperextension at the metacarpophalangeal joint. Open reduction and internal fixation of the metacarpal shaft fracture with plates and screws provides excellent stability but may cause extensor tendon adhesions with a scar on the dorsal aspect of the thumb.
Bennett’s fracture is unstable, and concern exists as to whether inadequate reduction/fixation leads to long-term consequences such as osteoarthritis, weakness, or loss of function of the first carpometacarpal joint. The disadvantage of the Wagner technique is possible exudate from pin site and a pin-tract infection. If it is observed, we recommend oral administration of antibiotics. In severe case, we recommend K-wiring.
Joint instability following Bennett fracture–dislocation is rare. Stability is assumed as long as the fragment is fixed properly to the shaft. If subsequent instability occurs, the rational choice of treatment is the Eaton method because this method, although originally introduced to strengthen and reconstruct the anterior oblique ligament, also has a stabilizing effect on the dorsal radial ligament.
The Rolando fracture can be associated with significant posttraumatic arthritis if there is significant incongruity at the articular surface of the base of the first metacarpal. Marked decrease in hand function can result if proper fixation is not achieved [46].
The complications of type 3 are frequent and include retraction of the first web, persisting pain, decreased thumb mobility, and strength.
Despite the reported incidence of arthrosis and accompanying pain, and limitation of motion in the long term, we have seen few cases.
7.1.2.10 Preferred Method of Treatment for Athletes
In our opinion, because of the instability of this fracture and for complications, the closed reduction and plaster casting is an inappropriate treatment for athletes.
The treatment of Rolando fracture depends on the severity of comminution of the fragments and the degree of displacement. Two methods of treatment of Rolando Fracture are unacceptable for treatment in athletes: soft dressing with early motion and closed reduction and casting.
7.1.2.11 Directions for the Future
As in all articular fractures, the key to success is anatomical reduction. We believe that reduction of articular fractures of the head and the base of the first metacarpal should be helped by arthroscopy in the future. For this to happen, further development of arthroscopic equipment is needed. The current 1.9-mm scopes are very fragile and break easily. This weakness implies more expensive and difficult access to this treatment.
Extra-articular fractures should be treated so as to enable early motion with a treatment as least aggressive as possible.
Key Points
Fractures of the first metacarpal occur at all athlete levels, and the initial diagnosis and treatment are very important to return to sports.
The treatment of intra-articular fractures presents a challenge due to deforming forces acting at the base of the thumb.
Anatomical reduction, either by the open or closed method, should be the aim of treatment.
Athletes must be protected from contact until healing has progressed to a point where reinjury or complications are unlikely and performance standards and expectations can be met.
Osteoarthrosis is correlated with the quality of reduction of the fracture.
Suggested Readings
Culp RW, Johnson JW (2010) Arthroscopically assisted percutaneous fixation of Bennett fractures. J Hand Surg 35A:137–140
Arthroscopic evaluation of reductions has suggested that the joint surface may not be completely reduced. The authors propose a method of arthroscopic reduction and stabilization of Bennett fractures of the first metacarpal base.
Green DP, O’Brien ET (1972) Fractures of the thumb metacarpal. South Med J 65(7):807–814
Green & O’brien in 1972 described a classification to first metacarpal base fractures. This classification is still used nowadays. They listed different methods of treatment for each type fracture.
Lutz M, Sailer R, Zimmermann R, Gabl M, Ulmer H, Pechlaner S (2003) Closed reduction transarticular Kirschner wire fixation versus open reduction internal fixation in the treatment of Bennett’s fracture dislocation. J Hand Surg 28B(2):142–147
The authors compared open reduction and internal fixation with closed reduction and percutaneous transarticular Kirschner wiring. The type of treatment did not influence the clinical outcome or the prevalence of radiological posttraumatic arthritis.
7.2 Phalangeal Fractures
7.2.1 Extra-articular Phalangeal Fractures
Abstract
Phalangeal fractures are the most common sports-related hand fractures. The author discusses the physical findings, imaging, and treatment options based on fracture configuration, associated lesions, and type of sport activities. Conservative and operative treatments are discussed. Each athlete with an extra-articular phalangeal fracture should be approached as an individual case as no single set of treatment guidelines applies to all injuries or all athletes.
Phalangeal fractures are the most common sports-related hand fractures [47]. Even subtle injuries, such as a simple finger jam, can lead to a phalanx fracture, and therefore, many are initially undiagnosed. An undiagnosed phalanx fracture can significantly affect the athletes’ career.
7.2.1.1 Physical Findings
The classical symptoms and signs of finger fractures are constant pain, swelling, deformity, hematoma, and/or skin abrasion.
In athletes, the proximal phalanx is fractured more frequently than the middle or distal phalanx [47].
The mechanism of injury will influence the fracture pattern and consequently the finger deformity [48]. Generally, a direct blow on the dorsum of the finger will yield a transverse fracture with various degrees of comminution. A twisting injury will cause a spiral fracture, while an axial compression in combination with a torque will usually lead to a short oblique fracture.
Proximal phalangeal fractures will usually angulate with a volar deformity (Fig. 7.18) because the proximal fragment is flexed by the interossei muscles, while the distal fragment is pulled into hyperextension by the central extensor slip acting at the basis of the middle phalanx.


Fig. 7.18
Angulation of a proximal phalanx fracture
Middle phalanx fractures are less predictable with regard to angulation. A distal third fracture will angulate with the apex in volar deformity due to the action of the flexor superficialis tendon (FDS) on the proximal fragment. A proximal third fracture usually angulates dorsally because the FDS tendon flexes the distal fragment and the central slip extends the proximal one.
Distal phalanx fractures are generally comminuted and often associated with nail bed laceration and/or subungual hematoma.
Care must be taken to evaluate the digit for rotational deformity (Fig. 7.19). This is best accomplished by flexing the fingers and viewing the nail bed. Comparison with the contralateral uninjured hand is mandatory.


Fig. 7.19
Rotational deformity
Key Point
Check for rotational deformity!
7.2.1.2 Imaging
A minimum of three X-ray views is necessary: posteroanterior (PA), oblique, and lateral views. The oblique view is necessary since a PA view or a lateral view alone can miss an oblique spiral fracture. When assessing an individual digit, one should obtain a radiograph of the digit only. The amount of initial displacement, fracture location, and orientation are indicators of stability [49].
Key Point
Three X-ray views are necessary– PA, oblique, and lateral views.
7.2.1.3 Classification (Table 7.1)
Table 7.1
Fracture classification
Fracture pattern | Fracture location | Soft tissue damage |
|---|---|---|
Transverse | Neck | Closed |
Oblique | Shaft | Open |
Spiral | Base | |
Comminuted |
Classification criteria of extra-articular fractures include fracture pattern (transverse, oblique, spiral, comminuted), fracture location (neck/shaft/base and proximal, middle, or distal phalanx), and the extent of soft tissue damage (open, closed).
7.2.1.4 Nonoperative Treatment [48, 50, 51]
The goal in hand fracture management is to achieve fracture stability. Stability is achieved when a fracture maintains its reduction and does not displace either spontaneously or with motion. Most phalanx fractures are functionally stable, either before (intrinsic stability) or after closed reduction, and amenable to nonoperative treatment.
Key Point
Most extra-articular fractures are functionally stable and amenable to nonoperative treatment.
Distal Phalanx Fractures
Fractures of the distal phalanx are common hand fractures, and the thumb and the middle finger are the most frequently injured.
Tuft and shaft distal phalanx fractures are usually treated by splinting for a short period (10–15 days) with or without percutaneous pinning (Fig. 7.20). Distal fractures most commonly result from a crush injury with associated nail bed lesions and subungual hematoma. Nail bed repair is indicated in the presence of nail laceration, while hematoma decompression provides a rapid pain relief.


Fig. 7.20
Percutaneous pinning of a distal phalanx fracture
Key Points
Distal phalanx fractures are common.
Nail bed repair is indicated in the presence of nail laceration.
Proximal and Middle Phalanx Fractures
Proximal and middle phalanx fractures can be displaced or not displaced. For undisplaced and stable fractures, conservative functional treatment can be proposed with buddy taping with or without a finger splint.
For displaced fractures, the surgeon should make one attempt at closed reduction, under local anesthesia by gentle axial traction with the metacarpophalangeal (MCP) joint flexed to 90° in order to relax the intrinsic muscles. Traction may be difficult to maintain. Once the reduction is performed, the digit is checked to determine stability of the reduction and rotational alignment. No more than 10–15° of angulation should be accepted in adults, otherwise digital motion will be impaired with a loss of equilibrium between flexor and extensor tendons. Rotational deformity is unacceptable.
Postreduction radiographs should be obtained at two orthogonal incidences.
Fractures with potential instability should be protected with a splint and controlled weekly to confirm the maintenance of the alignment.
Digital stiffness can be prevented by a correct immobilization. The intrinsic plus position (IPP) is the safest position for hand splinting. In the IPP, the metacarpophalangeal (MP) joints are flexed and the interphalangeal are fully extended. MP joints recover well from flexion, while interphalangeal joints recover well from extension due to the difference in the shape of metacarpal head and collateral ligament anatomy. When MP joints are flexed, collateral ligaments tighten preventing ligament retraction.
For cooperative and compliant patients, a conservative functional treatment can be proposed with good results. The wrist and metacarpophalangeal joints are immobilized in a dorsopalmar splint. The wrist is dorsiflexed 30°, and the metacarpophalangeal joints are flexed 70–90°, while the IP joint are in full extension. In this intrinsic plus position, the extensor aponeurosis is taut and stabilizes the proximal phalanx fracture.
Early active motion is essential. Exercises are supervised by a hand therapist, and, as fracture consolidation occurs, buddy taping and strengthening exercises with silicone putty are introduced.
Return to play is guided by the patient’s symptoms, radiological healing, and potential for reinjury. If the fracture can be adequately protected and immobilized, without interfering with the patient’s ability to play, then participation can be allowed, providing the patient has adequate pain control.
For uncooperative and noncompliant patients, a static and nonremovable splint in IPP is often necessary.
Average time for clinical union is 4–6 weeks for proximal phalanx fractures and longer for middle phalanx or transverse fractures and in smokers.
Key Points
For displaced fractures, make one sole attempt at closed reduction.
No more than 15° of residual angulation should be tolerated.
Control weekly the maintenance of the alignment.
The intrinsic plus position is the safest for hand splinting.
Early active motion is essential.
7.2.1.5 Operative Treatment
The primary indications for surgical treatment are to provide stability to an unstable fracture with minimal damage to the surrounding soft tissues. If the extension deformity exceeds 15–20° or in case of shortening of more than 2 mm, operative treatment is recommended. Additional indications include irreducible fractures, open fractures, multiples fractures, and fractures with associated tendon, nerve, or vascular damage. Rotational deformity requires operative treatment.
The ideal treatment of unstable phalangeal fractures remains controversial [47, 48, 50–57]. Despite conceptual advantages of open reduction in providing anatomical alignment and stability, closed methods offer a worthwhile alternative. A stable construct is only one of many factors influencing the outcome, while the invasiveness of the fixation technique is among other determinants.
There are several implants and techniques available for stabilization of extra-articular phalangeal fractures, allowing the surgeon to tailor the fixation to the fracture pattern, patient’s exigencies, and surgeon’s preferences.
Closed Reduction and Pinning (Coaptive Fixation) [47, 48, 50–53]
Percutaneous pinning allows the conversion of an initially unstable fracture to a more stable configuration capable of tolerating early motion.
The main advantage of percutaneous pinning is to minimize the additional iatrogenic soft tissue injuries; avoiding periosteal stripping during fracture reduction helps to ensure bone healing, and, with experience, operative time and radiation exposure can be reduced. The main disadvantage of this technique lies in the absence of a rigid internal fixation, and the wires could bend with strong flexion forces. Stability of fixation depends on Kirschner wire (KW) diameter and placement.
This technique is mainly useful in transverse or short oblique shaft fractures.
For transverse fractures, crossed wires produce the best resistance to torsion. The distal fragment can be reduced by gentle external manipulation, and the KW can be inserted in a crossed anterograde or retrograde manner. An extra-articular mini-invasive lateral approach is preferable with introduction of the KW retrograde in the retrocondylar fossa or anterograde for proximal phalanx fractures (Fig. 7.21).


Fig. 7.21
Anterograde percutaneous pinning of a comminutive basal fracture in association with a carpometacarpal dislocation in a rugbyman
A functional treatment with protected early active motion is started promptly [47, 48, 50–53]. Controversy does exist regarding the initiation of motion with coaptive fixation. Risk of infection, pain, nonunion, and fracture displacement have been cited as reasons to delay motion. Weiss [51] investigated initiation of motion at 1, 2, 3, and 4 weeks for patients with proximal phalanx fractures and KW fixation. Results showed no difference in final results when motion was started between 1 and 21 days. However, when motion was delayed more than 21 days, there was a significant loss of mobility.
For oblique or spiral fractures, percutaneous pinning is an alternative to screw fixation (Fig. 7.22). The KWs, engaging both cortices, are cut 3 mm from the skin edge. It is recommended to avoid lateral band transfixation. In my opinion, screw fixation with a mini lateral approach is most suitable for these inherently unstable fractures.


Fig. 7.22
Percutaneous pinning of an oblique phalanx fracture
Key Points
Main advantage: minimally invasive
Main disadvantage: absence of rigid internal fixation
Closed Reduction and Percutaneous Screw Fixation (Fig. 7.23) [47, 52, 53]

Fig. 7.23
Percutaneous screw fixation in a football player allowing immediate and unrestricted motion. (a) PA view (b) lateral view
In highly motivated patient with spiral or long oblique fractures, a percutaneous screw fixation may be performed. Reduction can be obtained by longitudinal traction with a finger trap. Through a small lateral incision and under fluoroscopic control, the fracture is reduced and fixed with a reduction clamp. It is mandatory to check for malrotation before inserting the titanium self-tapping screws. Functional treatment is started immediately after the stabilization.
Key Point
Perform percutaneous screw fixation in high motivated patients with spiral or long oblique fracture.
Closed Reduction and External Fixation
Indications for external fixation of extra-articular phalangeal fractures include open fractures, highly comminuted fractures, and fractures with significant bone loss. External fixation is particularly useful in case of severe associated soft tissue lesions in order to reduce further damage. The technique is relatively simple, and greater precision is added by the use of C-arm image intensifier. Predrilling has the advantage that the site and the direction of the pins are better controlled. The insertion of the pins in a transverse plane helps to obtain the best hold on bone but may hinder the patient or restrict exercises.
In general, the complexity of these fractures influences the final functional results.
If the fracture cannot be adequately reduced and stabilized by closed means, open reduction and internal fixation is recommended.
Key Point
External fixation is useful in open fractures with soft tissue lesions, massive comminution, and significant bone loss.
Open Reduction and Internal Fixation (ORIF) [47, 48, 50–54, 56–58]
Restoration of bony anatomy is a prerequisite for return to normal function; however, anatomical reduction should not be obtained at the cost of soft tissue scarring. This concept is essential in the open approach to extra-articular phalangeal fractures.
Open reduction can be achieved via a dorsal or a lateral approach.
ORIF via Dorsal Approach
The skin incision may be straight or curved. With a straight incision, venous drainage is better preserved, while a curved incision has the main advantage that the skin and the tendon scarring are not in the same plane. The extensor tendon is split longitudinally. It is important to protect the periosteum, which should only be elevated close to the fracture line.
ORIF via Lateral Approach
Following the AO recommendations to plan the lateral line of incision, the finger should be fully flexed and the ends of the joint skin creases should be marked with dots. The lateral incision line is obtained by connecting the dots with the extended finger. Nerve branches are identified and protected. Oblique fibers of the lateral band are retracted or resected unilaterally to allow visualization of proximal fractures.
When possible, this lateral approach is preferable in order to reduce extensor tendon manipulation and postoperative adhesions.
There are numerous implants and techniques available for fixation, and it is recommended to become familiar with all of them in order to tailor a specific fixation to the type of patient and fracture pattern.
Key Point
The lateral approach reduces extensor tendon manipulation and postoperative adhesions.
Screw Fixation [47, 48, 50, 52, 53, 58]
Screw fixation is indicated for displaced long oblique or spiral fractures where the goal of fixation is compression between fragments. For phalangeal fractures, screw diameter generally ranges from 1.1 to 2.0 mm. A minimum of two screws must be used. In case of short fracture lines, a single lag screw is used in combination with a protection plate. The fracture is cleared of interposed tissues, reduced by gentle traction, and temporarily held with one or two small forceps. At this stage, it is mandatory to check digital alignment.
Lag screws should be inserted perpendicular to the fracture plane. Screw orientation and bicortical fixation are determinant for stability. The recommended AO technique [58] of screw placement is to drill, measure, and insert lag screws. The use of lag screws requires a gliding hole in the near cortex and a threaded hole in the far cortex. One should avoid inserting screws too close to the fracture apex and countersinking in the metaphysis where the cortex is very thin. Countersinking is indicated in the diaphyseal bone to reduce tendon irritation and to increase the contact area between the screw head and the bone.
Key Points
Screw fixation is indicated in long oblique and spiral fractures.
A minimum of two screws should be used.
Screw orientation and bicortical fixation are determinant for stability.
Plate Fixation (Figs. 7.24 and 7.25) [47, 48, 50, 52–56, 58, 59]

Fig. 7.24
Plate and screw fixation

Fig. 7.25
Condylar plate fixation of a comminutive para-articular fracture
There are several plate configurations (straight, unicondylar, T plate, eight-hole) and thicknesses ranging from 1.0 to 2.0 mm.
The miniplate system has many attributes making it ideal for the internal fixation of extra-articular phalanx fractures. The plate provides rigid fixation allowing early motion, and its low profile is suited to the small bones of the hand. Lu and coworkers [54] tested five fixation techniques on comminuted phalangeal fractures. They showed that plates offered the most rigid construct in torsion and palmar bending.
Obliquity of the fractures determines plate position. If the obliquity is visible in the PA view, a lateral plate should be applied so that screws can be inserted perpendicular to the fracture line. If the obliquity is visible on the lateral view, the plate should be applied dorsally. Straight plates should have at least five holes and should be centered over the fracture.
The minicondylar plate, with its blade angled at 90°, is an elegant solution for comminuted or periarticular fractures (Fig. 7.25). In the series of Ouellette [56], complication rate is significantly high and the functional results do not correlate with severity of soft tissue injury, fracture location, and complication.
The role of soft tissues in plate fixation of proximal phalanx has been well analyzed by Ouellette and coworkers [55]. Soft tissues increased the stability of lateral minicondylar plates by 163 %, lateral straight plates by 157 %, dorsal minicondylar plates by 126 %, and dorsal straight plates by 104 %, providing a dorsal tension band effect. The results suggest that a laterally placed straight or minicondylar plate may provide as much stability to a phalanx with a midshaft fracture as does the traditional, more invasive, dorsally placed minicondylar or straight plate.
Experience shows that plate fixation of unstable and complex phalangeal fractures is very efficient and reliable but not free of potential problems. Plate fixation demands meticulous handling of soft tissue and does not allow for any technical error. Despite the advances in plate design, plate fixation of phalangeal fractures can be fraught with complication and unsatisfactory results [59, 60].
Key Points
Obliquity of the fracture determines plate position.
Straight plates should have at least five holes and should be centered over the fracture.
The minicondylar plate is an elegant solution for periarticular or comminuted fractures.
Tension Band Wiring [53, 57]
Tension band wiring (TBW) provides stability with minimal fixation and soft tissue dissection. Wiring can be used alone or in association with KW. Our experience with TBW is limited, and even if good results are described in phalangeal transverse fractures, we reserve this expeditive technique for replantation (Fig. 7.26).


Fig. 7.26
Tension band wiring and internal pinning
7.2.1.6 Postoperative Care [47, 48, 50–53, 55, 57, 58, 61]
Postoperative care varies with the patient, the condition of the soft tissues, and the stability of the fracture. Successful rehabilitation of phalangeal fractures addresses the need of maintaining fracture stability for bone healing, introducing soft tissue mobilization, remodeling any restrictive scar from injury or surgery, and preventing contracture of the joint capsule. As pointed out by Hardy [61], it is important to recognize the intimate relationship between these three tissues (bone, soft tissue, and scar) in the rehabilitation of phalangeal fractures.
Reliable patients can be managed with early protective motion. Static splints can be used between hand therapy sessions to prevent contractures. Dynamic splinting and serial finger casting are used in recalcitrant, severe, and late presenting cases.
Associated soft tissue lesions require modification of the postoperative therapy. Emphasis is placed on initial hand positioning to protect the fracture reduction, on exercise to maintain or regain joint range of motion, and on specific tendon-gliding exercises to prevent restrictive adhesions.
As little as 1.7 mm of flexor tendon, excursion during the first 4 weeks after reduction may substantially diminish peritendinous adhesions at the fracture site [52]. Synchronous wrist and digital exercises may also reduce peritendinous fracture adhesions. Freeland and Orbay showed that early motion of adjacent joints in extra-articular fractures expedites recovery of motion and strength without adversely affecting fracture alignment and leads to earlier return to work.
Patient education for edema control is an essential component of the initial therapy. Rest, ice, compression, and elevation (R.I.C.E) are emphasized.
The final functional outcome is determined both by the surgeon’s supervision of the appropriate hand therapy and by the surgeon’s skill in fracture managing. It is important that hand therapists understand the role and intent of various forms of fixation as they dictate the course of rehabilitation. Ideally the therapist should have access to the radiographs and the operative report.
Key Points
Start with early protective motion ASAP in adequate and cooperative patients.
R.I.C.E (rest, ice, compression, elevation) is essential for edema control.
7.2.1.7 Outcome and Complications [48, 58–61]
With improvement in rigid fixation techniques, outcomes have improved but complication rate is still high. Several factors have been shown to affect the success or failure of stabilizing techniques. In a large prospective study, Pun et al. [58] identified open fractures, comminuted fractures, and associated soft tissue injury as unfavorable prognostic factors in digital fractures of the hand fixed with KWs. In a series of fractures treated with plate fixation, Page and Stern [59] showed 57 % complications. In the study by Kurzen [60], we found complications in 31 out of 54 patients after plate fixation where stiffness was the most frequent complication despite active early motion. According to the classification of the American Association for Hand Surgery, only 21 % of our patients had good or excellent mobility. However, in most of our patients that underwent secondary tenolysis, range of motion improved substantially and beyond the limits defining stiffness.
Key Points
Complication rate should not be underestimated.
Open fractures, comminuted fractures, and associated soft tissue injury are unfavorable prognostic factors.
Stiffness is the most frequent complication in plate fixation.
7.2.1.8 Return to Sport Activities
There are no consensus guidelines [47] or agreed-upon criteria for safe return to ball sports following extra-articular phalangeal fractures, with complete elimination of complication risks and increased performance. The goal of the treatment strategy is to allow earlier return to play accepting a moderate risk of complication. Age, patient’s expectations, type of fracture, hand dominance, and type of sport are among the many issues that must be considered when discussing treatment strategy for a particular athlete. The player’s position and the type of grip need to be integrated into the decision-making process. The increasing pressure that elite athletes experience to return to play should not be underestimated.
In conservative treatment, emphasis is placed on initial hand positioning to protect fracture reduction and on functional exercises to maintain or regain articular motion and prevent complications.
Internal fixation can provide optimal stability to the fracture, which allows early return to play. Potential complications of the surgical strategy should be always discussed with the patient, the coaches, and the sideline hand therapists. This situation is particularly relevant if there are complications or if, at the end of the operation, fixation is not stable enough to allow the promised rehabilitation protocol. A final decision must be individualized for each athlete considering the basic anatomy and biomechanics.
A progressive and graduated rehabilitation is begun followed by non-ball-handling exercises and use of protective hand splints, gloves, or taping. Athletes must be protected from direct contact until healing has progressed to a point where complications are unlikely and objective performance meets athletes’ and coaches’ expectations for a return to competition.
Key Points
There are no consensus guidelines for returning to sport activities.
Returning to sport activities must be individualized for each athlete according to age, expectations, type of fracture, hand dominance, and type of sport.
7.2.1.9 Preferred Method of Treatment for Athletes
(a)
Stable fractures → conservative functional treatment, dorsal splint, and buddy taping.
(b)
Displaced fractures → single attempt at closed reduction. If successful, treat as stable with weekly clinical and radiological controls. In case of recurrent instability, treat as unstable fracture.
(c)
Unstable fractures:
Transverse or short oblique → plate
Long oblique–spiroid → percutaneous or open screw fixation
Comminuted or periarticular → condylar plate.
Suggested Readings
Kozin SH, Thoder JJ, Lieberman G (2000) Operative treatment of metacarpal and phalangeal shaft fractures. J Am Acad Orthop Surg 8(2):111–121
A detailed review of operative possibilities of metacarpal and phalangeal shaft fractures. In addition to providing a useful review of basic science and biomechanics, the authors accurately discuss operative treatment in terms of advantages, disadvantages, and complications.
Kurzen P, Fusetti C, Bonaccio M, Nagy L (2006) Complications after plate fixation of phalangeal fractures. J Trauma 60(4):841–843
The authors show a high incidence of complications after plate fixation of phalangeal fractures; in spite of early mobilization, stiffness is the most frequent complication. Plate fixation is not to be condemned, but it demands meticulous managing of soft tissue and does not permit any technical error.
Pun WK, Chow SP, So YC, Luk KD, Ngai WK, Ip FK, Peng WH, Ng C, Crosby C (1991) Unstable phalangeal fractures: treatment by A.O. screw and plate fixation. J Hand Surg 16A(1):113–117
A prospective study of 284 digital fractures. The article brings attention to the poor prognostic factors including open fractures, comminuted fractures, and soft tissue injury.
7.2.2 Metacarpophalangeal Finger Joint Fractures
Abstract
The metacarpophalangeal (MCP) joint is located at the base of the finger. Trauma to this joint affects function of the entire finger. A ball strike is one of the main causes of hand injuries, and specifically MCP joint fractures, in athletes. The mechanism of injury is through avulsive, torsional, and axial forces. The avulsive fracture is most common. Usually the athlete complains of pain and dysfunction in one or more fingers. The most common signs of a fracture are swelling, subcutaneous hematoma, and deformity of the finger. A routine X-ray of the MCP joints includes anteroposterior, lateral, and oblique views. The treatment goals are to achieve a congruent, stable, and mobile joint. With athletes, the goal is return to sport as soon as possible. Most of the athletic finger fractures can be treated conservatively by buddy taping or extension-blocking splint. Surgical management is indicated only for displaced, unstable fractures that cannot be stabilized or reduced otherwise. There are minimally invasive surgical techniques using cannulated screws and classical ORIF with miniscrews or plates. Uncontrolled edema and poor initial diagnosis and treatment will ultimately impede the achievement of normal digital motion. Premature return to sports can prolong the recovery phase and provoke complications.
7.2.2.1 Natural History
The metacarpophalangeal (MCP) joint is located at the base of the finger. Trauma to this joint affects the function of the entire finger. MCP joint fractures constitute approximately 23 % of all metacarpal (MC) fractures [62]. The mechanism of injury varies; however, sport is the primary cause of MC fractures between the ages of 10 and 39 [63]. In athletes, a ball strike is one of the main causes of hand injuries. Approximately 50 % of all sports-related MC fractures are intra-articular. Most often, the index, ring, and fifth fingers are injured [64]. There is no typical MCP joint fracture type with respect to ball strikes.
7.2.2.2 Anatomical Peculiarities
Metacarpophalangeal joints connect two anatomical and functional zones of the hand: the compact palm and the mobile digits. Compared to the more distally located interphalangeal (IP) joints, the MCP joints are more protected as they lie within the palm. On the other hand, they are more mobile and, in some positions more prone to fractures. It is noteworthy that the MC head is asymmetrical; it widens from dorsal to volar and, on the lateral head side, the horizontal radius is shorter than the vertical (Fig. 7.27). The collateral ligament origin lies dorsal to the axis of rotation and thus is tightest in full MP joint flexion. Additionally, in this position, the articular joint congruity is greater, thus making the flexed position the most stable. Conversely, in full extension, joint congruity is limited, and thus abduction, adduction, and rotation are possible.
Fig. 7.27
The collateral ligaments are tight in full MP joint flexion (a) and relaxed in extension (b)
7.2.2.3 Pathogenesis
An athlete positions the hand to receive or throw the ball. At that moment, the hand is stable as a result of the dynamic balance between the muscles and ligaments. When the ball is caught incorrectly, with only some of the fingers, the force of impact targets a small surface increasing the likelihood of injury. The mechanism of injury for intra-articular fractures of the MCP joint is through avulsive, torsional, and axial forces. The avulsive force is most common and occurs when the ball hits the interdigital space and deviates one of the fingers producing a shearing force and pulling out part of the articular surface (Figs. 7.28 and 7.29). If the impact force causes torsion, the fracture line may continue from the articular surface to the diaphysis (Fig. 7.30). An axial compression force may result from a hit to the longitudinal axis. This force produces a multifragmental fracture with partial depression of the articular surfaces (Fig. 7.31) [65]. The combination of angular and axial forces produces a die-punch fracture which causes an interphalangeal plateau depression, expansion and breaking of the articular ring, and blocking of the joint [66] (Fig. 7.32a). When the force of the impact is great, this can provoke a simultaneous fracture of the MC head and base of proximal phalanx (Figs. 7.33, 7.40, and 7.41). In most cases, articular fractures of the MCP joints are accompanied by lesions of the surrounding structures: collateral ligaments, volar plate, and sometimes sagittal fibers of the extensor hood. In some cases, the articular fractures are complicated with joint dislocation (Figs. 7.33 and 7.34).
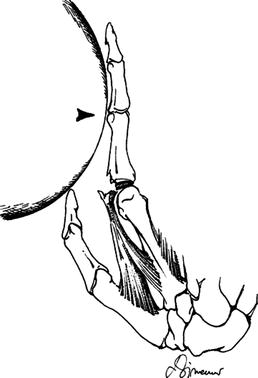


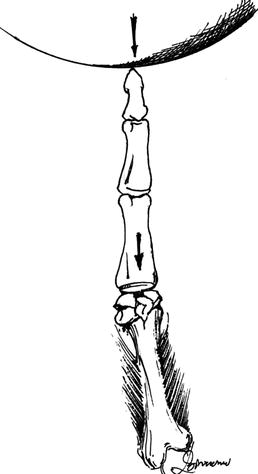


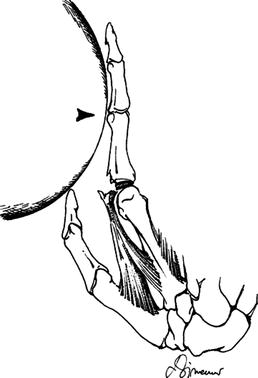
Fig. 7.28
When the ball hits and deviates one of the fingers, it produces a shearing force and pulls out part of the articular surface

Fig. 7.29
Avulsion-type articular fracture of the proximal base. Screw is applied to fragments including at least 25 % of articular surface

Fig. 7.30
The impact force causes torsion, and the fracture line continues from the articular surface to the diaphysis
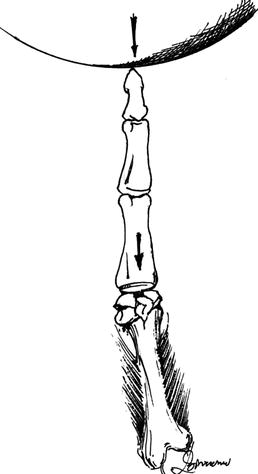
Fig. 7.31
The axial compression force produces a multifragmental fracture with partial depression of the articular surfaces
Fig. 7.32
(a) A die-punch fracture which causes an interphalangeal plateau depression, expansion, and breaking of the articular ring. (b) Open reduction by elevation of the depressed part of the articular surface, filling with cancellous bone graft, and fixation with two screws

Fig. 7.33
Fracture of MC head and proximal base combined with volar MCP joint dislocation

Fig. 7.34
Fracture of MC head combined with dorsal MCP joint dislocation
7.2.2.4 Physical Findings
A thorough history of the mechanism of injury is important. The following information is needed:
1.
At what angle did the ball hit the hand?
2.
What were the shape, weight, and approximate speed of the ball?
3.
What was the status of the hand immediately following the trauma and what motion was possible?
4.
What was the main complaint?
5.
Was there previous surgical/nonsurgical treatment?
The athlete usually complains of pain of varying intensity and dysfunction of one or more fingers. The most common visible changes are swelling, subcutaneous hematoma, skin abrasion, and deformity of the finger. Very rarely, there may be an open fracture. The examination must include assessment of the stability and mobility of all fingers. Both active and passive digital range of motion may be limited and painful. Angular or rotational deformity must be identified. A rotational deformity is diagnosed by asking the patient to flex the digits. If the fingertips flex toward the scaphoid tubercle, the fracture is undisplaced. Rotational deformities are poorly tolerated. A small deformity which may be invisible with the fingers extended may cause overlapping of the digits when the fingers are flexed (Fig. 7.35). A rotational deformity of less than 5° will cause a 1.5-cm finger overlap when the digits are flexed [67]. When testing for a rotational deformity, posttraumatic swelling and pain may make finger motion difficult. In this case, the test should be done under local anesthesia. During sports activities, a coach or trainer who inspects and manipulates the digit following a ball strike in order to return the athlete promptly to the field can miss the initial injury. The fracture may thus be missed as well as the opportunity to minimize posttraumatic swelling and more serious sequelae. Up to 30 % of hand injuries are misdiagnosed or mismanaged [68].


Fig. 7.35
A small deformity which is invisible with the fingers extended may cause overlapping of the digits when the fingers are flexed
7.2.2.5 Imaging
A routine X-ray of the MCP joints includes anteroposterior (AP), lateral, and oblique views. A true AP view can only be obtained for the middle finger. This is because the skeletal arch of the hand causes the X-ray of image of each ray to be superimposed. Therefore, the Brewerton projection is recommended for a view of the MC heads. In this view, the dorsum of the palm and the fingers lie on the plate with the MCP joints in flexion of 60–65° (Fig. 7.36) [69]. Multiple fragment fractures require a CT scan and 3D reconstruction.
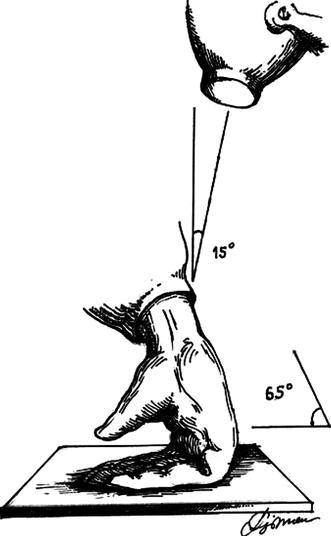
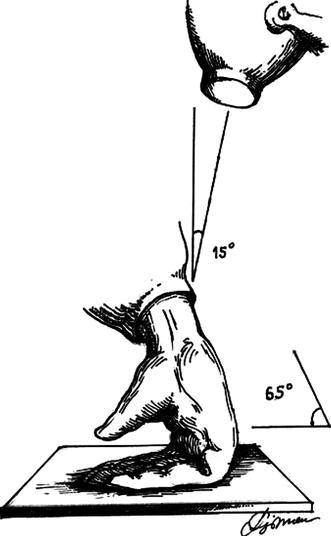
Fig. 7.36
In the Brewerton projection, the dorsum of the fingers lies on the plate with the MCP joints in 60–65°of flexion
7.2.2.6 Classification
There are two approaches to classifying articular fractures of the MCP joints. One approach considers the articular surfaces of the MC heads and base of proximal phalanges separately, while the other classifies fractures of both articular surfaces together [70, 71]. As the MCP joints are an integrated structure, the general classification of Pechlaner is more appropriate. The classification presents 6 types of fractures involving the surface of the MC head and 5 types of articular fractures of the base of proximal phalanx [62].
Fig. 7.37
(a) Fractures involving the articular surface of MC head. (b) Fractures involving the articular surface of the base of proximal phalanx. 1 Avulsion fractures, 2 oblique shaft fractures, 3 osteochondral fractures, 4 T-fractures, 5 comminuted fractures, 6 bone loss fractures
Fractures involving the articular surface of MC head (Fig. 7.37a):
Type MCH 1 – Avulsion fractures
Type MCH 2 – Oblique shaft fractures
Type MCH 3 – Osteochondral fractures
Type MCH 4 – T-fractures
Type MCH 5 – Comminuted fractures
Type MCH 6 – Bone loss fractures
Fractures involving the articular surface of the base of proximal phalanx (Fig. 7.37b):
Type PPB 1 – Avulsion fractures.
Type PPB 2 – Oblique shaft fractures involving the base
Type PPB 3 – Osteochondral fractures
Type PPB 4 – T-fractures of the base
Type PPB 5 – Comminuted fractures
Type PPB 6 – Bone loss fractures
7.2.2.7 Treatment
Appropriate treatment starts on the sports field where the injured finger is immobilized, elevated, and ice applied until the patient reaches the hospital.
The treatment goals are to achieve:
1.
Congruent articular surfaces
2.
Stable fracture fixation
3.
Restoration of full range of digital motion
4.
Timely return of the athlete to competition or training
7.2.2.8 Nonoperative Management
Most athletic finger fractures can be treated conservatively [72]. The indications for nonoperative treatment are:
1.
Undisplaced stable fractures
2.
Partially displaced stable fractures
Stable fractures remain undisplaced during active and passive movement. Partially displaced fractures are those with fragment dislocation of 0.5 cm [73]. Fractures of relative stability are fractures prone to displacement with any finger activities. Undisplaced MCH1 and PPB1 fractures must be immobilized by buddy taping for a period of 5 weeks. Buddy taping preserves the stability of the fracture while allowing joint motion (Fig. 7.38). The athlete can return to a modified training regime 1 week after treatment.


Fig. 7.38
Buddy taping preserves the stability of the fracture as well as allowing joint motion
Undisplaced, unstable fractures with a fracture line into the diaphysis, or minimally displaced fractures types MCH2 and PPB2, are prone to dislocation. They require temporary immobilization with an extension-blocking splint for 3 weeks. In the splint, the MCP joints should be flexed between 75 and 85°, but the IP joints left free to move (Fig. 7.39) [74]. Usually after the third week, the risk of dislocation decreases and the splint is replaced with buddy taping for 2 weeks. If the sport requires contact with the ball, the athlete can return to the field after 6 weeks. They should wear a forearm radial or ulnar gutter splint for protection while playing and then remove it when not playing.
Fig. 7.39
In the extension-blocking splint, the MCP joints should be flexed between 75 and 85°, but the IP joints are left free to move
7.2.2.9 Surgical Treatment
The goal of operative treatment is to achieve anatomical reduction, rigid internal fixation, and early mobilization. Due to potential complications, surgical management is indicated only for displaced, unstable fractures. There are two types of surgical techniques: classical and minimally invasive.
Minimally invasive techniques involve closed reduction and percutaneous fixation with K-wires or cannulated screws. K-wire fixation is less desirable as the fixation is only partially rigid requiring cast immobilization, thus delaying early mobilization of the digit. Recently, the trend is toward using mini-cannulated screws to achieve rigid fixation with minimal soft tissue exposure and allow mobilization 24 h after surgery [75]. Additionally, postoperative swelling and pain are reduced compared with other techniques. Unfortunately, the minimally invasive technique is applicable only for uncomplicated fractures.
7.2.2.10 Classical Technique
Depending on the location and type of fracture, the surgical approach to the MCP joint is dorsal or volar. Surgical treatment goals are in accordance with the basic AO principles for internal fixation of small fractures: anatomical reduction, rigid internal fixation, and early mobilization [76]. Additionally, especially for athletes, the implant should not impede sport activities.
Miniscrews and plates are the preferred implants for fracture fixation. Screws are applied to fractures with larger fragments including at least a quarter of the articular surface (Fig. 7.29). The diameter of the screw should be up to 25 % of the size of the fragments. Screws with a diameter of 1.0, 1.2, 1.3, 1.5, 1.7, and 2.0 mm. are employed. They create maximum compressive force when placed perpendicular to the fracture line (Figs. 7.33, 7.34, 7.40, and 7.41).



Fig. 7.40
Fractures involving the articular surface of the base of proximal phalanx and multifragmental fracture of the MC head

Fig. 7.41
A large force can provoke a simultaneous fracture of the MC head and base of proximal phalanx
Indications for fixation with plates are mostly T-shaped and multifragmental fractures. The most appropriate is a 1.5-, 1.7-, or 2.0-mm plate [73] (Figs. 7.42, 7.43, 7.44, and 7.45). The new low-profile locking plates expanded the options for rigid fixation of comminuted fractures.





Fig. 7.42
(a) Fracture of the proximal base and collateral avulsion. (b) Open reduction and internal fixation by condylar plate

Fig. 7.43
T-fracture of the proximal base treated by condylar plate

Fig. 7.44
(a) Complicated oblique shaft fractures involving the base. (b) Open reduction and internal fixation by plates and lag screws

Fig. 7.45
(a) T-fracture of the proximal base with comminution of the radial diaphysis. (b) Open reduction and plate fixation. (c) Bone healing
Intra-articular fracture–dislocations are too difficult for closed reduction due to soft tissue interposition into the fracture line. This type of injury must be managed by open reduction and internal fixation (Figs. 7.33 and 7.34).
Die-punch fractures provide special challenges as they usually consist of several small fragments that are difficult to reposition and secure. The surgical intervention includes elevation of the depressed part of the articular surface, filling the subchondral defect with cancellous bone graft, and fixation with screws or a plate (Fig. 7.32a, b) [66].
7.2.2.11 Postoperative Care and Return to Sports
Postoperative care targets early initiation of a rehabilitation program that should include:
(a)
Reduction of edema through elevation, compression bandages, the use of physical agents such as ultrasound and electrical stimulation, and early controlled mobilization. Uncontrolled edema will impede ultimate normal digital motion.
(b)
Pain reduction in order to prompt early motion.
(c)
The initiation of motion to the involved joint, when appropriate.
(d)
Maintaining motion in all noninvolved joints and soft tissues around the fracture. Special splinting techniques may be required to achieve these goals, and thus, the patient should be referred to a hand therapist or physical therapist with experience in treating hand fractures.
The ultimate goal is for the athlete to return to sport after a full recovery. The exact time frame for return to sports will depend on various factors including the sport, the hand involved, the type of fracture, and the fracture treatment. Athletes with uncomplicated fractures may expect to return to sport activities after 6 weeks. For complicated fractures and those with a longer postoperative recovery period, the time frame is more than 8 weeks. Premature return to sports can prolong the final recovery and provoke complications.
7.2.2.12 Complications
The most common complications after MCP joints fractures are:
1.
Loss of normal range of motion of the digit(s)
2.
Rotational or angular deformities
3.
Tendon adhesion or rupture
4.
Prominence of the implant and loosening of the osteosynthesis
5.
Osteoarthritis
Metacarpophalangeal joint fractures resulting from ball sports do not differ from those with other etiologies. Specificities of their treatment in the athlete respond to the need to return him/her to competitive sport or training as quickly as possible. This objective does not contradict the basic principles for treatment of articular fractures. With early diagnosis, prompt prevention of edema, stable fixation with minimal operative trauma, and early rehabilitation, these objectives of treating the athlete can be met.
Key Points
In athletes, a ball strike is one of the main causes of hand injuries. The mechanism of injury for the fractures of MCP joint is through avulsive, torsional, and axial forces. The avulsive mechanism is most common. Upon physical exam, the athlete complains of pain and dysfunction of one or more fingers. The most common visible changes are swelling, subcutaneous hematoma, skin abrasion, and deformity of the finger. The classification presents 6 types of fractures involving the surface of the MC head and 6 types of fractures of the base of proximal phalanx. The indications for nonoperative treatment are undisplaced stable and partially displaced stable fractures. The goal of operative treatment is to achieve anatomical reduction, rigid internal fixation, and early mobilization. There are classical and minimally invasive types of surgical techniques. The ultimate goal in post-op period is for the athlete to return to sport after a full recovery. Metacarpophalangeal joint fractures resulting from ball sports do not differ from those with other etiologies. Specificities of treating the athlete with an MCP joint fracture arise due to the need to return him/her as quickly as possible to competitive sport or training.
Suggested Readings
Margles SW (1988) Intra-articular fractures of the metacarpophalangeal and proximal interphalangeal joints. Hand Clin 4:67–74
This article discusses the treatment of intra-articular fractures of the MP and PIP joints. It reminds us of the specific anatomy of the MCP joints and the mechanism of intra-articular fractures. Most of these fractures represent avulsion injuries or compressive force. Radiographic examination of the fractured joint is mandatory. The routine views are AP and lateral. The author pointed out that the lateral view is difficult to interpret and thereafter recommended the Brewerton view in some metacarpal head fractures. According Margles, the two axioms of treatment of intra-articular fractures of the MP and PIP joints must be:
1.
Near anatomic and stable position of fracture fragments with or without open reduction
2.
Early active motion exercises
The need for early exercises dictates the need for rigid internal fixation. The author recommended dorsally placed screws for the MC head fractures. Both axioms have been illustrated with two cases. The most serious complications after treatment for intra-articular fractures of the MCP and PIP joints result from stiffness secondary to scaring to ligamentous structures or inadequate reduction or loss of position of fracture fragments. “Meticulous surgical technique and rigid fixation will decrease the possibility of inadequate reduction or loss of position of facture fragments,” concluded Margles.
Pechlaner S (1999) Intra-articular fractures of the metacarpophalangeal joint. In: Bruser P, Gilbert A (eds) Finger bone and joint injuries, 1st edn. Martin Dunitz Ltd., London
The chapter by Sigurd Pechlaner covers the topics of intra-articular metacarpophalangeal joint fractures. Pechlaner’s statement at the beginning of the text nicely summarizes the inherent problem with treatment of these injuries: “For these multiple lesions, it is necessary to create a concept for therapy which, with respect to the lesion in question, aims for an exact repositioning, to achieve maximum stability and to start the functional treatment as soon as possible. Even when the treatment has been optimal, good result is not always obtained.” The processes of diagnoses of these fractures are a combination of clinical awareness, careful examination, and accurate radiographs. The general classification Pechlaner presents is 6 types of fractures involving the surface of the MC head and 6 types of fractures of the joint surface of base of proximal phalanx. The author presented relatively high incidence of MCP joint fractures – 23 %. The subchapter of treatment includes conservative and operative treatment. Conservative treatment is appropriate for none or slightly dislocated avulsion fractures and oblique shaft fractures involving the metacarpal head, without major soft tissue damages. The goal of operative treatment is primary stabilization of the fractures. Optimal stability must be accomplished with a minimum of osteosynthesis material. The author characterized every fracture type mentioned in the classification and defined most appropriate type of treatment. There were illustrations and photographs intervention to show the intervention type and result of treatment.
Wolfe S, Katz LD (1995) Intra-articular impaction fractures of the phalanges. J Hand Surg 20A:327–333
Wolfe and Katz discuss management of impaction fractures of the metacarpophalangeal and interphalangeal joints. The authors report the outcomes of a small group of patients with impaction fractures treated with open reduction and internal fixation with or without bone grafting and immediate range-of-motion exercises. Nine patients, 3 fractures of MCP joint, and 6 fractures of PIP joint were evaluated. Average age was 29 years. Seven out of nine injuries occurred due to sporting activities. CT imaging was performed to help delineate the fracture configuration. The PIP impaction fractures were of two types. The MP joint fractures were alike and consisted of a central depression of a portion of the articular surface with disruption of the articular rim. Metaphyseal bone grafting was necessary to support the articular surface in six cases. Rigid internal fixation, most frequently employing a composite wire tension band technique, allowed postoperative active range-of-motion exercises. At an average follow-up period of 21 months, the authors reported excellent range of motion for all acute patients. There was no loss of articular congruency. The impaction fractures are unique and should be considered separately from the other intra-articular fractures of the fingers.
7.2.3 Articular Fractures and Fracture–Dislocations of the PIP Joint
Abstract
Proximal interphalangeal (PIP) articular fractures and fracture–dislocations are common injuries in ball sports. Inappropriate management of these injuries may lead to a rapid loss of function, chronic pain, or premature joint arthritis and thus definitely compromise an athlete’s career. Principles of treatment are based on a comprehensive classification of these lesions as presented here and include achieving congruent articular surfaces, stability of the repair, and early mobilization to avoid stiffness. In addition, management should adjust to the specific needs of each athlete at different levels (sport objectives, role on the field, hand dominance, specific requirements during play, etc.). It is the responsibility of the hand surgeon not to minimize these injuries, to fully evaluate them and to treat them with the best standards of care, in order to achieve the earliest possible return to sports without compromising later activities. A thorough understanding of the anatomy and biomechanics of the PIP joint is prerequisite to accurate management of these injuries. Intrinsic stability of each injury pattern as well as the potential operative risks must be carefully appreciated in order to decide whether a fracture has to be managed conservatively or operatively. If surgery appears to be the best option, then it should be as least invasive as possible to minimize additional injury to soft tissues. Additionally, it should provide and maintain enough stability to allow early and safe postoperative motion.
7.2.3.1 Natural History and Prognosis of Untreated Lesions
Mechanisms of Injury
Due to their high involvement, low protection, long lever arm, and low lateral and rotational mobility, the long fingers and especially the PIP joint are prone to a whole spectrum of injuries, especially in ball sports [77, 78]. Most of these injuries result from a fall, direct contact with opponent when fighting for the ball, or a direct blow from a ball when catching it. Axial load, coronal or sagittal deviation, and rotation are the basic vector forces implied in these injuries. Additionally, shear forces mostly depend on the position of the joint at the time of impact, and forces applied by the flexor and extensors tendons, usually tightened at various degrees during play, are present. The moment force (the amount of energy delivered as a function of time) also determines to a great extent the type of lesions that will occur: High energy during a very short time will tend to produce « pure » bone lesions like shear fractures, whereas a rather low impact force is likely to be followed by lesions involving both hard (bone) and soft (ligament) structures. Summarized, all these forces and their vectors act in combination to produce a variety of lesions from simple sprains to comminuted PIP fracture–dislocations. In practice, these notions remain mostly theoretical, as it is rarely possible to deconstruct/reconstruct the mechanism of injury for a specific lesional pattern.
Injuries Left Untreated
The healing potential obviously depends on the amount of articular damage, more specifically on the extent of lesions to the cartilage, their bony support, and the degree of dislocation, which mirrors ligamentous damage. In general, compared to the DIP joint, the PIP joint has a limited, although not absent [79], remodeling capacity, and it is prone to stiffness after trauma or immobilization longer than 3 weeks [80]. The posttraumatic evolution of untreated lesions varies according to the type of lesions. Articular injury patterns can be categorized into two groups: articular fractures of the (distal) condyles of the proximal phalanx and fracture–dislocations of the proximal interphalangeal joint.
Undisplaced or minimally displaced condylar fractures can heal with little or no functional impairment. However, the degree of cartilage damage can be difficult to assess, especially in shear fractures (see classification below), and so the risk of degenerative arthritis. The most common unicondylar oblique fractures tend to be primarily displaced or to displace secondarily, leading to lateral deviation of the middle phalanx and/or some degree of malrotation. PIP flexion is also impaired to some extent in this situation. Depending on the finger involved and the side of deviation, malalignment can be more or less accepted by the athlete. Later, posttraumatic arthritis will develop, due to either malalignment or articular step-off or both. Limitations will then be mainly due to pain and progressive stiffness.
For PIP fracture–dislocations, the prognosis is essentially defined by two factors. One is the degree of dislocation, depending itself on the size of the fragment left attached to the palmar and lateral joint stabilizers. Instability increases dramatically when the size of this fragment is more than 40 % of the middle phalanx base [81]. The second is the degree of comminution. Arthritic changes in the mid- to long term depend on the amount of cartilage damage, which is usually unknown. Left untreated, minimally displaced (less than 1 mm in the anteroposterior plane), slightly comminuted fractures may heal primarily provided they are unloaded for the critical four first weeks. Other unreduced, more displaced fractures will invariably be followed by pain, functional impairment, and progressive arthritis, which can occur within a few months [79]. Multifragmented fractures at the base of the middle phalanx are similar to a pilon tibial fracture and have the same potential of destruction. They may end with a painful and stiff joint quite rapidly, thus signifying the end of competitive sports. Thus, rapidly recognizing and optimally treating this potentially devastating injury cannot be overemphasized.
7.2.3.2 Condylar Fractures of the Proximal Phalanx
Because of their convex shape and more solid bony architecture, fractures of the condyles are much less common than fractures of the base of the middle phalanx. They usually occur in young sportsmen, mainly males and predominantly in ball sports, during rapid axial loading of an outstretched finger by a ball. Coronal shear fractures occur in hyperflexion or extension with forces exerted at some angle to the finger axis (Fig. 7.46).
Fig. 7.46
Comprehensive classification of condylar fractures. Arrows indicate direction of forces/displacement for coronal fractures
Classification
Most condylar fractures occur mainly in the sagittal plane and were classified by London [82] according to the fracture lines into monocondylar (transverse or box fracture type 1, short and long oblique type 2) and bicondylar fractures with a T or Y pattern (type 3). Less common fractures occur in the coronal plane and were later described by Weiss and Hastings [77]. The condylar fragment can be displaced dorsally (type 4a), resulting from palmar forces, or volarly (type 4b), resulting from an axial–dorsal impact. In their series, half of the fractures were sustained when playing a ball sport.
Transverse monocondylar or box fractures are usually stable and can be treated conservatively provided they are undisplaced with only minimal step-off at the joint level.
Even if initially undisplaced, oblique fractures are potentially unstable, and three-fourths of them displace secondarily.
The stability of type 3 bicondylar fractures depends on the displacement and the fracture pattern; an oblique component and metaphyseal involvement makes them less stable.
Type 4 coronal fractures are usually displaced initially as they result from direct and often violent blows.
The classification depicted in Fig. 7.46 accounts for approximately 95 % of all fractures of the condyles, the remaining 5 % being either comminuted fractures or osteochondral (chip) fractures. Up to 75 % of all condylar fractures are of type 2.
Displacement can be graded as (0) no displacement, (1) no visible deformity, (2) causing visible deformity, and (3) range or direction of movement altered.
Further elements to be taken into account in decision-making are the associated injuries and whether it is an open clean or an open dirty (not unusual when happening on the field) wound.
Physical Findings
Pain, swelling of the PIP joint, and functional impairment are the most common and usual findings. Deformity may be almost unnoticeable when occurring in the sagittal plane, whereas lateral deviations are usually obvious. Sideways angulation in particular is by itself suggestive of a condylar fracture. Rotational deformity is also possible. Joint mobility is restricted by pain, swelling, and angulation. Careful spot palpation elicits pain over one or the other condyle, possibly over the whole head of the phalanx in bicondylar or coronal fractures. A painful joint with an hemarthrosis and without any visible deformity should raise the suspicion of an osteochondral fracture.
Imaging
In addition to the clinical findings, plain radiographs are sufficient in most cases to make the diagnosis and to orient the treatment. They should be true posteroanterior and true lateral and well centered on the PIP joint, so that overlapping of the two condyles can be confidently appreciated. In type 2 fractures, oblique views may help to more accurately determine the actual fracture plane, as it is rarely purely sagittal but rather often inclines toward the volar side of the phalanx. This has to be recognized so as to plan the approach correctly, in particular when considering percutaneous fixation.
When doubtful, CT scans with 3D reconstructions can help in choosing the best appropriate management. They also have their indications in comminuted and osteochondral fractures that can be otherwise difficult to assess.
Nonoperative Management
Decision-making is based upon a careful weighing up of the risks and advantages of operating or not a specific fracture in a specific athlete. Considering the fracture features is not sufficient. Hand dominance and use in play, injury location with regard to the actual ball sport, age, athletic perspectives, and season timing are all important issues and must be taken into account, especially in professional athletes. Sportsmen are keener to undergo surgery than others. They hope to resume sport earlier, often to the detriment of mid- or long-term outcome, which can negatively influence their career. Careful balance of all these elements is mandatory.
Once this has been outlined, nonoperative treatment of condylar fractures of the middle phalanx can be an option in the following situations, an extremely close follow-up being warranted:
As a rule, the only true stable condylar fracture amenable to conservative management with success is the box or type 1 fracture.
Undisplaced oblique or bicondylar fractures can be treated conservatively, provided they are closely and weekly followed with good comparative X-rays. Any displacement is an indication for surgery.
Minimally displaced (less than 1 mm) osteochondral and chip avulsion fractures can be managed conservatively as well, as long as the athlete is ready to wear a digital splint for the required time. This has to be weighed against the technical difficulties and postoperative risks of an intra-articular fixation of such fractures.
Once decided, the PIP joint is immobilized for 3–4 weeks in a thermoformed, well-adjusted splint in a neutral or near neutral (10° flexion) position. For oblique fractures, the MP joint is maintained in 70° flexion to release further tension. Immobilization longer than 4 weeks has been shown to decrease final range of motion [83]. Gentle, progressive, passive, and active mobilization is started at 4 weeks. Sports are allowed from 6 weeks on, after having checked bone healing by X-rays. Earlier return with strapping to an adjacent finger may be a matter of discussion, but it would be difficult to justify loss of reduction due to premature return to competition.
Surgical Management
Most (and all displaced) condylar fractures require an operative stabilization, with the aim of early mobilization and return to sports. The following points should be born in mind:
Orientation of fracture line(s) must be carefully checked to choose the most appropriate approach.
Fixation must be anatomic and able to resist the anticipated forces encountered during the specific sport activity. Two, rather than one, screws or Kirschner pins are mandatory to secure fixation.
Difficulties in operative management of condylar fractures, particularly of type 3 fractures that are often comminuted, should not be underestimated.
Short oblique fractures receive their blood supply almost exclusively through their single attachment to the collateral ligament. Osteonecrosis of the condylar fragment may ensue from operative injury to this area.
Small Kirschner pins and lag screws whenever possible are best suited to fix condylar fractures in most cases. Extensive soft tissue dissection leads to more stiffness and should be kept to a minimum. Mini-invasive methods with short incisions and hardware of appropriate size (1.3- to 1.5-mm screws) are mandatory whenever applicable. Plates are associated with more joint stiffness and should be the last – rather salvage – option. External fixation is usually ineffective and not well accepted by sportsmen. Infection rates may be increased as the patients usually keep on training while wearing the device. Intramedullary pins can be an option for selected cases (type 4 fractures).
Postoperative Care
Active and passive motion should be initiated as soon as postoperative edema has improved, usually after 5–7 days. When not exercising, the PIP joint is splinted in full extension or slight flexion (no more than 10°). Position of hardware and fracture reduction should be regularly checked with radiographs. Pins should be removed at 4 weeks; screws can be left in place. From then on, therapy and activities can be intensified. Progressive return to sports with appropriate protective splinting may then be allowed.
Outcome
The prognosis of condylar fractures is closely related to the type of injury, associated lesions, and type of fracture. Type 1 and 2 fractures have a better outcome than type 3 and 4 fractures. Results also depend on the patient’s ability and willingness to follow the splinting and postoperative therapy program.
In the short term, initially stable and appropriately fixed simple fractures may achieve bone healing within 4 weeks; full or near full active mobility can be expected within 3 months from injury or surgery. More complex fractures may require up to 6 months of intensive therapy to achieve a useful – if not complete – range of motion.
Long-term prognosis depends on the quality of the reduction and the stability of the fixation. Articular step-off over 1 mm and/or articular damage, as well as malunion with unequal length of the condyles, are associated with the development of arthritis, which may occur within a few years, depending on the following applied constraints during play.
Complications
Stiffness may occur mainly after type 3 fractures, extensive approach to the joint, splinting in excessive flexion of the joint, or delayed mobilization. Tenoarthrolysis may be required after 3 months if therapy is not successful.
Devascularization of the condylar fragment in type 2a fractures may follow injury to the collateral ligament, ensued by bone necrosis and nonunion. This is a very serious, difficult to deal with issue. If recognized early enough, addition of autologous bone graft may be attempted. Later on, only salvage procedures might be considered, according to the finger involved and the specific sport conditions.
Intra-articular malunion modifies joint loading and mechanics. When clinically relevant (impairment of function/play, painful motion, or high risk of arthritis), an intra-articular corrective osteotomy has to be considered. It is a technically demanding procedure, requiring a dorsal approach through the extensor mechanism and exposure of the joint. A preoperative CT scan is mandatory to best determine the osteotomy plane.
Preferred Method of Treatment for Athletes
Type 1 fractures are treated conservatively by a digital splint and early mobilization.
Type 2a, short oblique fractures are treated by a mini-invasive approach to reduce the risk of fragment necrosis and osteosynthesis with one or better two 1.3-/1.5-mm lag screws, alternatively a screw and a Kirschner pin.
Type 2b, long oblique fractures are managed with an open midlateral approach (often slightly volar when the fracture plane faces volarly) and two to three lag screws (Fig. 7.47).
Type 3 fractures are treated either by lag screws, K-wires, or a combination of both, with the aim of minimizing injury to soft tissues and allowing early mobilization. A lateral or dorsal plate is the last option. In this case, the fixation must be stable enough to allow for early and intensive full range-of-motion exercises (Fig. 7.48).
Type 4 fractures are treated by intramedullary K-wires according to the method described by Cuénod (personal communication). The approach is through the base of the middle phalanx between the sagittal and lateral bands in a way similar to intramedullary pinning of metacarpal head fractures. The technique avoids opening the joint, spares the blood supply to the condyles, and provides stable fixation with noninterfering hardware (Fig. 7.49).
Illustrative Cases

Fig. 7.47
Condylar fracture type 2b (long oblique) in a basketball player. Pre- and postoperative views. Stable fixation with three lag screws. Active and passive mobilization after 5 days. Return to sports at 4 weeks

Fig. 7.48
Type 3 (bicondylar) fracture in a volleyball player. Mini-invasive fixation with two lag screws. Return to competition after 6 weeks
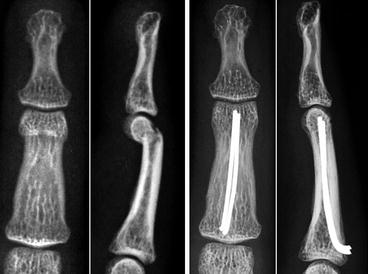
Fig. 7.49
Type 4a (coronal) fracture. Intramedullary fascicular K-wires (preoperatively and at 3 months) (Courtesy of Ph. Cuénod, MD)
Key Points
Pearls
Highly unstable fractures – stabilization most often required.
Indication of Surgery
Any displaced condylar fracture.
Preoperatively
Careful clinical evaluation for malrotation or angulation with PIP flexion
True posteroanterior and lateral views to assess any displacement
Oblique views to check for orientation of fracture line
Technical Points
Always try to minimize soft tissue damage – try percutaneous fixation if possible.
If percutaneous fixation is uncertain, do it open – there is no place for a second chance.
Lag screws of appropriate size are the first choice in most type 2 and possibly in type 3 fractures.
Reduction must be anatomic: no articular step-off, exact fit of the proximal apex into the phalanx.
Anterograde intramedullary K-wires are the primary choice for fixation of type 4 fractures.
If a plate has to be used, then it must be stable and allow early mobilization.
If open reduction is required, try not to open the joint, and if inevitable, take care not to detach the central slip.
Pitfalls
Fracture may be oblique rather than purely sagittal – adapt the approach accordingly.
One screw or pin may not be enough to maintain reduction in short oblique fractures.
Detachment of the collateral ligament may lead to bone necrosis of the condylar fragment.
Postoperatively
Initiate active and active-assisted range of motion at 5–7 days.
Splint the PIP joint in full extension between the exercising sessions.
Check regularly with radiographs.
Do not allow strenuous exercises if bone healing is uncertain.
7.2.3.3 Fractures and Fracture–Dislocations of the Base of the Middle Phalanx
Generally speaking, these fractures are seen more often than condylar fractures. The same is true for ball-sports athletes. They are typical sports injuries and are most commonly seen in young male athletes [84]. The middle and ring fingers are more frequently affected. There is a whole spectrum of lesions involving the bone and its ligamentous attachments, starting from easy-to-treat chip avulsions to devastating comminuted osteocartilageous injuries. The great functional importance of the PIP joint in hand motion and grip is key to bear in mind in the management strategy for each specific athlete.
Classification
Three main groups should be distinguished, as therapeutic measures will be tailored accordingly: (a) avulsion fractures, (b) intra-articular fractures with no dislocation, and (c) fracture–dislocations.
(a)
Avulsion fractures are chip fractures involving a small bone fragment attached to the lateral ligaments, the volar plate, or the dorsal extensor slip tendon (see Fig. 7.50 for a typical example). Most commonly one or sometimes two bony attachments are avulsed. When undisplaced and clinically stable, conservative treatment is recommended. When displaced and/or unstable, fixation is mandatory (see Fig. 7.51. Note that the real size of the fragment is larger than what is usually suspected from the radiographs).
(b)
Undislocated intra-articular fractures are the counterpart of condylar fractures on the other side of the joint. They are usually monofragmental, oblique fractures with no or little displacement, resulting from an axial quick loading with average energy. Depending on particular demands and potential risk of displacement, they may be treated conservatively or require operative fixation. If treated conservatively, close follow-up of these fractures is mandatory in order to switch to an operative management if displacement occurs. Two examples of such cases are shown in Figs. 7.52 and 7.53.
(c)
Classification of true PIP fracture–dislocations is based on:
The direction of dislocation, dorsal or volar
The stability, depending on the number and size of avulsed bony attachments
The degree of comminution at the base of the middle phalanx (shear component)
Three basic patterns are defined accordingly (Fig. 7.54):
Type 1: Volar fragment and dorsal dislocation. It occurs secondary to hyperextension of the PIP joint. Stability depends on the size of the fragment and decreases significantly when more than one-third of the articular surface is involved [85]. In this case, the main and accessory collateral ligaments remain attached to the volar fragment. Instability is the result of both the lack of volar lip and collateral ligament support. The rest of the phalanx base can be more or less impacted or comminuted. Type 1 is the most common fracture–dislocation of the PIP joint [80]. Surgery is indicated in unstable lesions (most cases).
Type 2: Dorsal fragment and volar dislocation. Stability greatly depends on the size of the fragment and the associated comminution. This is much less common than the type 1 [86]. Surgery indicated as in type 1 lesions.
Type 3: Dorsal and volar fragments or multifragmented/comminuted base of the middle phalanx, also described as pilon fractures. It results from high-energy axial load with tendons under tension when trying to catch a ball. The osteocartilagenous and impacted nature of these fractures makes them particularly difficult to treat. Surgery is required in most instances (see details below under sections Surgical Management and Preferred Method of Treatment).
Physical Findings
The main complaint is usually pain and consecutive functional loss. The affected joint is diffusely swollen and, in contrast with condylar fractures, deviations are often absent or almost unnoticeable. Accurate well-centered posteroanterior, lateral, and possibly oblique radiographs are required before attempting any manipulation, e.g., for testing stability – which could aggravate the lesions. Similarly, stability assessment after digital anesthesia should be avoided: it is unnecessary, difficult to grade usefully, and will be advantageously replaced by a careful examination of the radiographs, which provide all the information required to choose the proper treatment. It is much more important and sufficient for decision-making to have knowledge of the pertinent anatomy and of the lesional mechanisms than to elicit painful spots.
There is one exception to this rule: In case of a lateral and displaced avulsion fracture, stability must be checked – under anesthesia if too painful without – as an unstable fragment should be fixed in order to allow for early mobilization and to permit primary bone healing without secondary instability.
Imaging
Plain well-centered PA and lateral views are usually sufficient for an appropriate therapeutic decision. Although most of the time obvious, subluxation can be subtle, and careful assessment is mandatory to rule out tiny displacements indicative of potential instability. The “V” sign (loss of parallelism between the condyle curvature proximally and the dorsal basis of the middle phalanx distally) is a useful indicator. Comparison with an adjacent PIP or the contralateral one can be useful. CT scans are rarely indicated, except for type 3 pilon fractures, where they can assist in choosing the surgical approach or to evaluate central comminution.
Management Strategies
Based on the previously described classification, Table 7.2 gives an overview of the current management strategies for fractures of the base of the middle phalanx and fracture–dislocations of the PIP joint.
Table 7.2
Management strategies based on the classification of fractures and fracture–dislocations of the base of the middle phalanx
Type | Description | Stability/comminution | Treatment |
|---|---|---|---|
A | Avulsion fractures (small fragments) | Undisplaced/stable | Functional: digital splint 5–10 days followed by active motion and buddy tape |
Displaced and/or unstable | Miniscrew fixation and early active motion | ||
B | Intra-articular fractures (undislocated joint) | Undisplaced/stable | Digital splint in extension (dorsal fragment) or in slight flexion (volar fragment) for 3–4 weeks, followed by active range of motion |
Displaced and/or unstable | Screw(s) fixation and early active motion | ||
C1 | Volar fragment with dorsal dislocation | <30 % of articular surface no or little comminution | Extension block (splint or K-wire) |
30–50 % of articular surface no comminution | ORIF with small screws or small K-wires + extension block pinning | ||
30–50 % of articular surface with comminution | Primary volar plate arthroplasty or dynamic external fixation | ||
>50 % of articular surface no comminution | ORIF (volar or dorsal approach) | ||
>50 % of articular surface with comminution | Hemihamate reconstruction | ||
C2 | Dorsal fragment with volar dislocation | Usually unstable – treatment determined by the size of the dorsal fragment | Small fragment: pinning in extension ± central slip reinsertion |
Large fragment: fixation with miniscrews ± joint pinning | |||
C3 | Pilon fracture | Unstable – treatment depends on the number and size of the fragments | Large enough: ORIF with small screws ± autologous graft packing |
Small and numerous: dynamic external fixation – remodeling |
This strategy must be tailored to specific requirements; when the patient or team demands an early return to competition, to be safe, operative fixation has to be discussed in more detail, weighing the risks and benefits of each when both conservative and operative management are valid options.
Nonoperative Management
It is indicated in types A (avulsion fractures) and B (undislocated intra-articular fractures) that are initially undisplaced and considered as stable fractures. Avulsed small fragments fractures can be treated functionally in a digital splint for a short 5- to 10-day period until swelling has resolved, followed by active motion with buddy taping.
Initially stable type B fractures are appropriately treated in a digital splint in extension (dorsal fragment) or in slight flexion (volar fragment) for 3–4 weeks, followed by active motion as above.
Frequent radiographic and clinical checks are recommended so that any sign of secondary dislocation can be recognized and operated.
Surgical Management
When stability and articular congruency is an issue – and this is most frequent in PIP fracture–dislocations – operative treatment must be considered.
PIP fracture–dislocations are some of the most challenging fractures encountered in hand surgery such that they must be very carefully evaluated before embarking upon surgery that can be even more deleterious than the injury itself. One should be particularly cautious with soft tissue handling as any additional injury may increase instability and will increase swelling, secondary scarring, and eventually joint stiffness. On the contrary, the expected difficulty in itself is not a reason to dismiss operative treatment. One must consider short- as well as long-term outcome with respect to each particular setting – type of ball sport, position in play, hand dominance, etc.
The goals of operative management are threefold: maximize articular congruency/bone stability, minimize soft tissue injury, and allow early mobilization.
There is no consensus or evidence as to the best way to achieve these goals. Many different operative methods have been designed and developed over time: extension-block pinning with K-wires, miniscrews, and a wide variety of static/dynamic custom-made or industrial external fixators [87]. Considering the wide variety of fracture patterns encountered, one can suspect that a single method cannot be appropriate in all circumstances and that each fracture has to be treated specifically. The simplest operative method able to achieve the aforementioned goals should be prioritized. This is not an easy choice, and it obviously depends on the surgeon’s experience and on local preferences or habits.
Choice of surgical technique is based upon main features of the injury including (a) the presence, direction, and importance of dislocation; (b) the displacement and intrinsic stability of the fracture; and (c) the number and size of bone fragments (see Table 7.2).
Basically, any unstable or displaced fracture requires operative stabilization, possibly stable enough to allow early mobilization. This can be achieved by K-wires, or preferably screws whenever possible, as long as the fragments are large enough to accommodate them. Comminuted fracture–dislocations of the C1 and C3 types are most often unstable by nature and require particular attention and commitment. The degree of comminution is paramount for choice of the technique: Limited comminution in a C1 fracture can be quite adequately treated by an extension block with a single well-placed K-wire with an excellent outcome, due to the remodeling capacity of the para-articular bone fragments. More extensively comminuted fractures (C1 with more than 50 % of articular surface involved or C3 with many small impacted fragments) cannot be stabilized by screws and are best treated by primary volar plate arthroplasty, one of the numerous dynamic external fixation methods or (usually secondarily) by a hemihamate reconstruction of the middle phalanx volar lip.
Postoperative Care
Early active and passive exercises should be started as soon as possible, usually within a few days following surgery and be progressively increased according to swelling and pain. Competition athletes are usually keen to mobilize and should sometimes be held back rather than driven to move on too early or strongly. Anyway, careful follow-up with frequent clinical and radiological controls is advisable. Strenuous exercises should not be started before radiological signs of bone healing can be attested.
Postoperative mobilization must be adjusted according to the stability of the surgical construct. Close supervision by hand therapists, who rely on accurate instructions from the surgeon, is mandatory. Teamwork is the key to a successful rehabilitation.
Outcomes and Return to Sport
Outcome is closely related to the severity of the initial injury and to the quality of the surgical result in terms of articular congruency and stability, which determines the ability to mobilize early or not. A stable osteosynthesis and a well-reduced joint are prerequisites for a smooth postoperative therapy and consequently good outcome. Otherwise, there is little chance for satisfactory results.
Time of return to sports is almost always a matter of discussion with the athletes. However, bone and soft tissue healing follows biological rules rather than human wishes, and the surgeon will be well advised to refrain from allowing sportsmen to return to the field earlier than the average [88]. If not, it may well be at a much higher cost than the 2 or 3 weeks which have been spared.
Complications
Early on, loss of reduction is the risk most commonly encountered. If it occurs, reoperation may be extremely difficult but inevitable; it must be attempted nonetheless. It is usually less efficient than initial treatment but probably better than doing nothing. The challenge is then to reoperate on weakened tissues, especially bone, as loss of reduction occurs most often between the second and fourth week following the first operative procedure. The second operation will most probably end up with more hardware and more soft tissue injury, leading to more difficulties during mobilization and eventually more joint stiffness.
In later stages, stiffness [89] and joint arthritis [90] are the most usual complications. They depend on the degree of initial injury, both traumatic and operative. Treatment is first by physical therapy and ultimately by palliative operations like joint fusion or implant arthroplasty. This may well signify the end of competition for the ball-sports athlete.
Preferred Methods of Treatment for Athletes
Table 7.2 summarizes my preferred options for management of PIP fracture–dislocations. I tend to favor minimally invasive, when possible, percutaneous methods of fixation, with as little hardware material as possible (c.f. Vitale et al. [91] as a good technical example of this strategy). Indications for surgery should be generous; however, the procedure itself should be as atraumatic as possible, always bearing in mind that joint congruence and stability are the ultimate goal, whatever the technical choice.
Classification

Fig. 7.50
Rugby player with a stable volar and dorsal avulsion sports fracture of the middle finger of unknown mechanism. Treatment was by 10-day immobilization in a digital thermoformed splint, followed by active motion and strapping to the adjacent finger. Return to the field at 5 weeks

Fig. 7.51
(Left) Lateral avulsed bony attachment with clinical instability. (Right) Open reduction and screw fixation. Result at 1 month

Fig. 7.52
Undisplaced intra-articular fracture sustained when playing volleyball, treated conservatively in a digital splint for 4 weeks and then mobilized. Left on day 0, right at 4 weeks

Fig. 7.53
Almost the same pattern as in Fig. 7.52 but displaced. Treatment was by open reduction and a latero-volarly placed lag screw
Fig. 7.54
Classification of fracture–dislocations of the PIP joint (see text for explanations)

Fig. 7.55
Type C1 dislocation-fracture with approximately 40 % of the articular surface involved and little comminution. Treatment by a single dorsal K-wire for 4 weeks, followed by active and passive motion exercises. Return to handball at 9 weeks

Fig. 7.56
Type C1 monofragmental fracture–dislocation with 50 % of the articular surface involved, treated by two lag screws through a dorsal approach after percutaneous reduction with a small forceps. Result at 3 months. Full function. Active football player with no complaints at 6-year follow-up

Fig. 7.57
Rugby player with a pilon fracture treated with screws. Left: preoperative views. Right: result at 3 months

Fig. 7.58
Same player as in Fig. 7.57. Functional result at 3 years (ring finger). Resumed sport with occasional pain
Key Points
Pearls
Do not underestimate even small dislocations or cartilage damage.
The goals of operative management are threefold: maximize articular congruency/bone stability, minimize soft tissue injury, and early mobilization.
Choose the simplest operative method that achieves these goals.
Do whatever possible with as least hardware as possible to fully reduce and stabilize these fractures.
Indication
Nonoperative management is indicated in types A (avulsion fractures) and B (undisplaced intra-articular fractures) that are initially undisplaced and considered as stable fractures.
Surgery is indicated for any articular displaced and/or unstable fracture (primary or secondary).
Preoperatively
Stability – or potential instability – is best evaluated by careful assessment of the radiographs.
Clinical stability testing should be avoided in order not to aggravate the lesion, except for lateral avulsed fragments that might require fixation to reestablish stability and allow early ROM.
CT scans might be useful to evaluate the degree of comminution in pilon fractures.
Technical Points
Adapt the hardware to the size of the fragments, from K-wires and screws for large fragments to dynamic fixators, primary volar plate arthroplasty, and hemihamate reconstruction for highly comminuted fractures.
Be as minimally invasive and atraumatic as possible.
Use a dorsal approach for dorsally displaced fragments and a volar approach for volar fragments.
Use cancellous bone grafts generously in comminuted fractures, only after reduction and fixation have been achieved.
Pitfalls
Each fracture has to be considered individually – there is no single way to treat all.
Postoperatively
Initiate active and active-assisted range of motion according to the stability achieved by fixation.
Close supervision by hand therapists and teamwork with the surgeon are key to a successful rehabilitation.
Splint the PIP joint in full extension or slight flexion between exercise sessions.
Do not allow strenuous exercises before bone healing has occurred.
Suggested Readings
Kiefhaber TR, Stern PJ (1998) Fracture dislocations of the proximal interphalangeal joint. J Hand Surg 23A(3):368–380
Based on a thorough experience and a careful description of basic mechanisms leading to joint instability, a clinically oriented review of the basic patterns and therapeutic requirements of PIP fracture dislocations.
O’Rourke SK, Gaur S, Barton NJ (1989) Long-term outcome of articular fractures of the phalanges: an eleven-year follow-up. J Hand Surg 14B:183–193
More than 40 intra-articular fractures of the phalanges followed prospectively for a long period: a useful series to demonstrate the remodeling ability of the PIP joint and what can be expected from both conservative and operative management of these fractures.
Weiss AP, Hastings H (1993) Distal unicondylar fractures of the proximal phalanx. J Hand Surg 18A(4):594–599
The only case-series describing in some details the pattern, treatment and outcome of condylar fractures with the useful addition of coronal fractures to the previous classification by London.
7.2.4 DIP Finger Joint Fractures
Abstract
Articular fractures of the distal interphalangeal (DIP) joint are common finger injuries in ball sports that are often missed and underestimated leading to significant functional impairment of the digit. The common mechanism of injury is axial loading causing either condylar fractures of the head of the middle phalanx or articular fractures of the distal phalanx. Plain radiographs are usually sufficient to evaluate fracture patterns. The aim of treatment of DIP joint fractures is to maintain a good function of the hand by restoring a stable and painless joint with a strong pinch. Most DIP joint fractures can be managed nonoperatively; knowing when surgery can improve the functional outcome is the key in selecting when to proceed with a specific surgical intervention.
7.2.4.1 Introduction and Natural History
Articular fractures of the distal interphalangeal (DIP) joint are common finger injuries in ball sports. They are frequently missed and underestimated, often leading to significant impairment of the function of the digit. Athletes frequently have a story of finger dislocation reduced by a trainer and consult in a semi-acute state if they continue to suffer from pain and deformity as the fracture starts to displace [92]. A clear history should investigate the age of the patient, the sport ball activity, the hand dominance, and the precise mechanism of injury [93].
Axial loading is the common mechanism of injury [94]. It may yield unicondylar or bicondylar fractures of the head of the middle phalanx or articular fractures of the distal phalanx [93], commonly occurring while attempting to catch a ball [95]. Horiuchi presumed that an axial stress injury applied on a slightly flexed DIP joint causes dorsal dislocation of the distal phalanx with fracture of its volar base [96]. And when it is applied on a slightly hyperextended DIP joint, the result will be a volar dislocation of the distal phalanx with fracture of the dorsal base [96] (Fig. 7.59). These patterns of fracture–dislocation are generally sustained while playing a rugby match.
Fig. 7.59
Axial stress injuries of DIP joint [96]: (a) Dorsal fracture–dislocation. (b) Volar fracture–dislocation
7.2.4.2 Physical Findings
Patients should be questioned about past records of finger injuries, initial deformity, and reduction maneuvers that may have been attempted and any potentially associated injuries. Pain, swelling, weakness, deformity, restricted motion, and instability are common signs of DIP joint injury. Numbness and subjectively altered sensation indicate nerve involvement secondary to swelling [97]. Finally, a thorough and comparative orthopedic examination should be undertaken.
7.2.4.3 Imaging
Plain radiographs should be performed in at least two planes centered at the level of the sustained injury, consisting of posteroanterior and lateral views with additional oblique views which are helpful in evaluating comminution and fractures planes or when diagnostic doubt exists [93]. Radiographs may reveal uni- or bicondylar fractures of the head of the middle phalanx. The majority of fracture dislocations of the DIP joint are palmar dislocations with fractures of the dorsal articular surface. They generally represent severe bony mallet injuries. Clinical and laboratory examination have demonstrated that the DIP joint will remain concentric when less than 43 % of the joint surface is fractured. Subluxation is consistently noticed when more than 52 % of the articular surface is involved [98, 99] (Fig. 7.60). Dorsal fracture–dislocations occur infrequently (Horiuchi: 8 cases in long fingers [96], Hamer: 2 cases [100], Xiong: 1 case [97]). Although most fractures of the volar articular base of the distal phalanx result from avulsion of the flexor digitorum profundus, a small number of cases involve volar articular impaction with intact flexor tendons [98]. Occasionally, computed tomography scans may be indicated for further assessment of complex intra-articular injuries [93, 101].
Fig. 7.60
Wehbé and Schneider’s method of calculating the fracture size and the amount of joint subluxation [101]. (a) Fracture size = B/A + B. (b) Joint subluxation = C/A + B
7.2.4.4 Classification
London initially classified phalangeal condylar fractures into three types (Figs. 7.61 and 7.62):
Fig. 7.61
London’s classification of condylar fractures [96]: (a) Type I unicondylar undisplaced stable. (b) Type II unicondylar displaced unstable. (c) Type III bicondylar comminuted unstable
Fig. 7.62
Plain radiographs of condylar fractures: (a) London’s type I. (b) London’s type II. (c) London’s type III
The severity of these uncommon intra-articular fractures is frequently underestimated. However, assessment of condylar fractures patterns of the head of the middle phalanx helps to predict the progress and influences their management. Condylar fractures type 1 may be treated conservatively with frequent radiographs to check for displacement, while surgery is usually indicated for fractures with displacement (type II–III). Type II is believed to be significantly more unstable as the condylar fragment frequently displaces with conservative treatment owing to rotatory component [95].
7.2.4.5 Nonoperative Management
The aim of treatment of DIP joint fractures is to maintain a good function of the hand by restoring a stable and painless joint with a strong pinch [93]. Union of the fracture in its anatomical position is often not an obsessional condition to achieve this goal. For this reason, it is important that both the surgeon and the athletes have a clear idea of the treatment objectives from outset. Sometimes, injuries can be managed nonoperatively; knowing when surgery is likely to improve, the functional outcome is the key in selecting when to proceed with a specific surgical intervention [93].
Condylar Fractures
Conservative management is only appropriate for undisplaced or minimally displaced fractures (less than 1 mm) that are inherently stable (London’s type I) [93]. Splinting of the DIP joint in extension is then indicated using commercially available splint (Stack) or custom-fabricated splint fitted to the patient’s digit, to be worn continuously for 4–6 weeks, with sequential radiograph control for potential displacement [102] (Fig. 7.63). However, internal fixation using miniscrews can considerably reduce the immobilization period and allow early range of motion and rehabilitation for athletes.
Fig. 7.63
Plain radiographs of condylar fractures type I of London: (a) Initial radiographs. (b) Radiographs at 65-day follow-up after nonoperative management with extension splintage
Fracture–Dislocations
Dorsal fracture–dislocations of the DIP joint can be managed with extension-block splinting which can be used for all sizes of volar fractures according to Hamer. The DIP joint is flexed to reduce the fracture–dislocation and splinted in flexion. The splint is then extended 10° per week over 3–6 weeks period and allows early range of motion (ROM) [100]. It is quite difficult to maintain adequate taping of the splint to the injured joint, especially in the first days as the finger is quite swollen. Failure to maintain the reduction would be an indication for surgical treatment [100]. Finally, there is no possible indication of conservative management for the volar fracture–dislocation of the DIP joint.
7.2.4.6 Surgical Management
Fractures of the DIP joint significantly affect athlete’s career when they occur either in the playing season or in the off-season as they affect athlete’s training. Stable fixation is recommended for those patients [92] to allow early return to competition and rehabilitation.
Condylar Fractures
Inherently unstable and displaced condylar fractures of the middle phalanx (London type II, III) should be managed surgically. Several techniques are described to restore articular congruity and achieve stable fixation to allow early motion [103]:
Fracture–Dislocations
There is no current consensus as to the indication for surgical management of volar DIP joint fracture–dislocations [98] to justify the increasing number of described techniques:
CRPP can be done using the Ishiguro extension-block fixation [104] or by the umbrella handle technique [105].
OR via a transverse curvilinear or Y-shaped skin incision with internal fixation using:
Dorsal dislocation of the DIP joint with fracture of the volar base can be managed with extension-block pinning allowing early active motion [97] or a temporary fixation of the joint in the reduced position with intra-articular K-wire pinning. The volar fragment is reduced when necessary through a midlateral skin incision. A fixation by a K-wire or wire loop can be used to maintain the fracture reduction, with bone grafting in some cases [96].
7.2.4.7 Postoperative Care
Articular fractures of the DIP joint may be temporarily immobilized or pinned for approximately 4 weeks to allow fracture healing. ROM exercises for MCP, for PIP joints, and for the adjacent fingers should be initiated on the second postoperative day. By 4 weeks, the fracture has usually healed. The splinting or pinning is then removed, and active ROM is started [102]. Stable fixation of the articular fractures leaving possible active flexion and extension of the DIP joint allows immediate active mobilization during the first 4 weeks that may enhance the ultimate ROM of the injured joint. Between 4 and 6 weeks, passive mobilization is permitted [97].
7.2.4.8 Outcomes and Return to Sport
Early mobilization is essential for the eventual recovery of an injured finger [97]. From clinical experience, patients usually regain excellent functional ROM to the DIP joint. A small percentage of patients have limited motion, and they rarely express complaints of functional limitation [102]. It is believed that injuries to the DIP joint are more tolerant of fracture displacement and limited motion [98]. Athletes requiring ball-handling skills can return to sports within 3 months, after complete consolidation of the articular fracture of the DIP joint [98] (Figs. 7.64 and 7.65).
Fig. 7.64
Unicondylar fracture London’s type II: (a) Initial radiographs. (b) Closed reduction with K-wire pinning. (c) Radiological outcome after 4-year follow-up. (d) Clinical outcome
Fig. 7.65
Volar fracture–dislocation of the DIP joint: (a) Initial radiographs. (b) Open reduction articular transfixation and reinsertion with Jenning’s barbwire. (c) Radiological outcome after 13-month follow-up. (d) Clinical outcome
7.2.4.9 Complications
Few complications were reported to be associated with articular fractures of the DIP joint. Common complications include pain and swelling of the DIP joint that generally elapses within 6 months to 1 year. Stiffness or limited motion of the DIP joint rarely impairs useful hand function. Degenerative arthritic joint changes and minor osteophytes may occur at follow-up evaluation regardless of the treatment method [99]. Disability and relevant joint deformity are more related to failure of the treatment procedure. Pin-track infection is fortunately rare and can be avoided by special care to pin site.
7.2.4.10 Preferred Method of Treatment for the Athletes
Generally, conservative management is indicated for stable and minimally displaced articular DIP joint, immobilizing temporarily the joint. However, CRPP is preferred in athletes to allow early motion and seems, in our opinion, the most suitable method for stable and undisplaced condylar fractures of the head of the middle phalanx. For unstable and displaced condylar fractures, the least invasive surgical technique is selected to achieve stable fixation (pinning or miniscrews). Closed reduction and external distraction with percutaneous pinning of large fragments is indicated in comminuted and displaced condylar fractures [92]. Percutaneous extension-block pinning is the treatment of choice of dorsal dislocation of the DIP joint with open reduction of a compression fracture of the volar base of the distal phalanx [97]. We believe that the Ishiguro pinning is a simple and efficient technique to manage volar fracture–dislocation of the DIP joint for athletes.
Key Points
Articular fractures of the distal interphalangeal (DIP) joint are common finger injuries in ball sports.
Axial loading is the common involved mechanism of injury
Axial stress injury applied on a slightly flexed DIP joint causes dorsal dislocation of the distal phalanx with fracture of its volar base. When it is applied on a slightly hyperextended DIP joint, the result will be a volar dislocation of the distal phalanx with fracture of the dorsal base.
Plain radiographs centered at the level of the sustained injury are sufficient to evaluate comminution and fractures patterns:
Uni- or bicondylar fractures of the head of the middle phalanx (London’s classification)
Palmar dislocations with fractures of the dorsal articular surface (severe bony mallet fracture)
Dorsal dislocation with fractures of the volar articular base of the distal phalanx infrequent
Stable fixation (pinning, miniscrew) is indicated in condylar fractures allowing early range of motion.
Percutaneous extension-block pinning is indicated for dorsal dislocation of the DIP joint.
Ishiguro pinning can be indicated for volar fracture–dislocation of the DIP joint.
Suggested Readings
Horiuchi Y, ItohY, Sasaki T, Tasaki T, IIjima K, Uchinishi (1989) Dorsal dislocation of the DIP joint with fracture of the volar base of the distal phalanx. J Hand Surg 14B:177–182
The authors report nine cases of dorsal dislocations of the DIP joint with volar base fractures usually caused by an axial loading of the distal phalanx occurring during ball games. All these injuries were treated surgically, and the dislocation was easily reduced. The reduction is maintained by temporary DIP joint-blocking K-wire. The management of bony fragment varied according to individual injury. Active exercises were started 3–5 weeks after. The clinical and radiological outcomes at the last follow-up (6.4 years) were good.
O’Rourke SK, Gaur S, Barton NJ (1989) Long-term outcome of articular fractures of the phalanges: an eleven year follow up. J Hand Surg 14B:183–193
The authors studied clinical and radiological outcomes after 11 years on 59 articular fractures of phalanges. These fractures were classified into condylar fractures and basal fractures. The majority of these injuries were managed conservatively. Long-term outcomes depend on the volume of the fragment, comminution, displacement, and articular congruity. Pain, stiffness, and cold discomfort improved with time. Unlike bigger joints, the articular fractures of interphalangeal joints have good outcomes even with conservative management.
Xiong G, Zheng W, Wang S (2008) Extension block pinning of the treatment of a dorsal fracture dislocation of the distal interphalangeal joint: case report. J Hand Surg 33A:869–872
The authors reported a relatively rare case of dorsal dislocation of the distal interphalangeal joint associated with compression fracture of the volar base of the distal phalanx. They used extension-block pinning with K-wire in order to maintain the reduction during active flexion and extension exercises after surgery. At 49-month follow-up, the clinical results and radiographic findings were satisfactory.
7.2.5 Thumb Phalangeal Fractures
Abstract
Despite the functional importance of the thumb and the relatively high frequency of sports-related thumb phalangeal fractures, there is little evidence as to the best treatment, and published series do not provide information about specific treatment in athletes. Correctly exposed X-rays are mandatory for the diagnosis, and in some cases of intra-articular fractures, CT scans may be helpful. Axial trauma by a ball hitting the thumb may result in intra-articular fractures of the phalangeal base, whereas lateral deviation, hyperflexion, or hyperextension injuries are associated with avulsion fractures of collateral ligaments, the extensor tendon, or volar plate. Unicondylar fractures of the proximal phalanx are the most frequent fracture type of the thumb phalanges and mainly include ulnar collateral ligament avulsion fractures. Most thumb phalangeal fractures can be treated conservatively with short casts or splints as the fragments are often small and minimally displaced. Diaphyseal fractures are rare and only need internal fixation if there is a significant gap between the fragments of the distal phalanx or relevant malalignment in the proximal phalanx. Surgical treatment is indicated if the fracture is displaced and unstable, in the case of impacted articular fragments especially at the base of the proximal phalanx, with rotated condylar fragments of the head of the proximal phalanx or if there is additional ligamentous instability, namely, at the ulnar side of the metacarpophalangeal joint. The thumb must be protected even after surgical fixation, as the impact of a ball would exceed the primary stability of the fixation. Taping of an injured joint may be helpful when sport activities are resumed but is not possible to protect the thumb sufficiently in the early phase, as it cannot be taped to any adjacent finger.
Even though the thumb plays a fundamental role in different types of gripping and daily activities, the literature on phalangeal fractures of the thumb is very sparse except for avulsion fractures of the collateral ligaments of the thumb metacarpophalangeal joint (MPJ). Thirty percent of all phalangeal fractures occur in sports (including ball sports) injuries, and the thumb phalanges are involved in nearly 19 % of all phalangeal fractures with unicondylar fractures of the proximal phalangeal base being the most frequent type, accounting for 52 % of all thumb phalangeal fractures [107]. Rugby seems to be associated with thumb phalangeal fractures more often than basketball, volleyball, or American football [108]. Published series combine thumb and finger phalangeal fracture treatment and only include few if any cases of thumb phalangeal fractures which are not discussed separately. Detailed treatment recommendations for thumb phalangeal fractures in athletes or typical sport injuries are not described in the current literature.
The type of fracture of the thumb phalanges in ball sports depends on the direction of the impact of the ball: An axial trauma of the ball to the thumb may result in an often-comminuted intra-articular fracture of the phalangeal base. Lateral deviation of the thumb may cause a rupture or avulsion fracture of the collateral ligament, eventually with additional unicondylar compression fracture; forced flexion of the extended interphalangeal joint (IPJ) may result in an extensor tendon avulsion fracture, and rarely, rotational trauma may result in a spiral or oblique fracture of the phalangeal shaft. Clinical signs are pain, swelling and/or hematoma, and loss of function. As these signs are unspecific, standard anteroposterior (or posteroanterior) and lateral radiographs are mandatory for the diagnosis or exclusion of a fracture. Poorly taken radiographs must not be accepted, and as the position of the thumb is different from the other fingers, correct positioning of the thumb may be problematic and separate thumb views are necessary. Standard radiographs of the whole hand do not show these fractures adequately. Lateral views of the thumb are usually obtained without difficulty, but true AP or PA views may be more difficult. Failure to get proper radiographs with the joint space of the MPJ and IPJ joint projected free of bone overlapping may miss collateral ligament avulsion fractures [109]. If necessary, CT scans are performed to show more details of the fracture pattern (number of fragments, centrally impressed fragments, articular step-off, and displacement) in intra-articular fractures.
Tuft fractures are the result of crushing injuries of the distal phalanx of the thumb. They are thus most often not related to a direct impact of a ball, but rather due to trampling by another player’s shoe especially cleats. The often present subungual hematoma should be evacuated for pain relief, and eventually the nail bed injury has to be repaired using a running suture or fine resorbable sutures. The fracture itself is stable, and an intact or refixed nail plate provides additional stability, so often these fractures do not need any specific treatment and sports activities can be resumed depending on residual pain. With nail bed injuries and nail refixation, a splint should be applied for 3–4 weeks.
Transverse fractures of the distal phalanx are rare but are unstable especially if located proximal to the nail plate (Fig. 7.66). This fracture tends to show a volar apex angulation due to the pull of the flexor pollicis longus tendon. With minimal or no displacement, the thumb should be protected with a Stack-type splint during 4–6 weeks. If there is a relevant gap between the fragments, reduction under compression and additional K-wire fixation (eventually driven across the IPJ into the head of the proximal phalanx if the fracture is very proximal) is reasonable [110]. Interfragmentary compression using headless screw fixation has been described [111]. Sports activities can eventually be resumed with the Stack splint firmly fixed to the thumb using a tape bandage.
Fig. 7.66
Flexor and extensor tendon insertion on the distal thumb phalanx. Avulsion fractures may displace according to the tendon pull. Fractures of the volar edge of the distal phalanx correspond to avulsion fractures of volar plate, not the flexor pollicis longus tendon. Fractures distal to the vertical line are stabilized by an intact overlying nail plate. 1 Nail plate, 2 DIP, 3 extensor tendon, 4 volar plate, 5 flexor pollicis longus tendon (G. Chick © 2012, all rights reserved)
Avulsion fractures of the collateral ligaments of the IPJ may be treated conservatively with a Stack-type splint (about 2–3 weeks continuously, afterward taping to prevent lateral deviation during sports and daily activities) as the fragments are usually small and minimally displaced. The exact amount of displacement of articular fragments that can be accepted in hand and finger fractures is not known, but open reduction and internal fixation has been recommended if fragments are displaced more than 1 mm at the joint surface or involve more than 25 % of the joint surface [112]. In the case of a displaced and rotated avulsion fragment with clinical instability of the IPJ, open reduction and K-wire or preferably screw fixation if the fragment is sufficiently large is performed. Range-of-motion exercises can be started immediately, but the internal fixation should be protected with a Stack-type splint during 4 weeks, afterward with taping for sport activities.
Dorsal avulsion fractures include the extensor tendon insertion at the distal phalanx; a typical injury mechanism is a forced flexion by a ball while the thumb IPJ is actively extended. With very small fragments, treatment corresponds to closed pure extensor tendon ruptures, and a Stack-type splint is applied for 8 weeks holding the IPJ in slight hyperextension [113]. The splint must be worn 24 h and may only be removed for skin care with the IPJ passively held in extension. Later, the IPJ may be protected against hyperflexion by a ball with taping, and the splint is worn at night until 12 weeks after the injury. With larger fragments, the Stack-type splint is worn during 4–5 weeks until radiographs show adequate bone healing. The indication for internal fixation (preferably by lag screw fixation) is a large avulsion fragment with volar subluxation of the distal phalanx with fragments involving more than one-third of the joint surface in the lateral view. If the fragments do not allow stable fixation due to comminution, volar subluxation can also be treated with closed reduction and K-wire transfixation of the IPJ [114].
Volar fragments at the IPJ (which should not be confused with the volar sesamoid bone which is found in 22–86 % of thumbs examined [115]) correspond to volar plate avulsion fractures in dorsal dislocations of the IPJ. They are rare and do not need any specific treatment in most cases provided that the fragments are small and there is no dorsal subluxation. Repeated hyperextension should be prevented during 6–8 weeks with a splint or taping if necessary. A volar avulsion fragment may be part of impaction fractures of the base of the distal phalanx so X-rays have to be carefully checked. A literature search did not show any reports on flexor pollicis longus avulsion fractures from the distal phalanx of the thumb.
Impaction fractures of the base of the distal phalanx as a result of an axial trauma are very rare and can usually be treated conservatively with a Stack-type splint during 4 weeks (Fig. 7.67), and good mobility can be expected even if the X-rays show some malalignment [114]. Open reduction and internal fixation (ORIF) using K-wires or lag screws with possible bone grafting may rarely become necessary if there is relevant lateral deviation or impaction. Postoperatively, a protective splint is used until the X-rays show adequate bone healing.
Fractures of the head of the proximal phalanx are also rare injuries, and treatment depends on fracture type and displacement. Undisplaced fractures can be treated with a full-length thumb cast (but wrist joint not included) with regular radiological controls. Condylar fractures occur in combined axial load and lateral angulation injuries and tend to be very unstable. These unicondylar fractures can be stabilized with K-wires or better with one or more lag screws to allow early functional therapy. In bicondylar inverted Y-shaped fractures with one long condylar fragment, lag screw fixation may be possible, otherwise bicondylar fractures are best treated with stable plate fixation, and a lateral plate position is preferable to reduce extensor tendon adhesions. Reduction is often difficult, but anatomical reconstruction of the articular surface as well as correct longitudinal alignment should be attempted to avoid later degenerative changes. In bicondylar fracture fixation, the use of a reduction forceps with pointed tips often leads to rotation of the articular fragments so reduction and temporary fixation using fine K-wires may be advisable. Correct positioning of the implants is crucial to avoid collateral ligament injury or transfixation, and plates have to be perfectly adapted to the bone surface to avoid redisplacement of fragments when the screws are tightened.
Diaphyseal fractures of the proximal phalanx of the thumb are rarely reported and accounted for only 14 % of proximal phalangeal fractures of the thumb [107]. If they are not or only minimally displaced, conservative treatment with a thumb cast for 4 weeks is possible. Afterward the thumb has to be protected with a removable splint if ball-sport activities are resumed. Due to the very mobile thumb carpometacarpal joint and the fact that there is no overlapping over a neighboring finger, some malalignment is better tolerated than in fractures of the proximal phalanx of the long fingers. However, fractures showing more than 20–30° of angulation in the lateral plane (resulting in an extensor lag of the IPJ) or relevant rotational deformity should be treated with ORIF using lag screws or plates [110]. Depending on the fracture pattern, the surgical approach (and plate position) is chosen laterally or dorsally (Fig. 7.68). Early active mobilization is mandatory to prevent extensor tendon adhesions.
Fig. 7.67
Partial joint impaction fracture of the base of the distal phalanx following axial trauma by a volleyball at 3 weeks of conservative treatment in a thumb splint. (a) Lateral view, (b) PA view
Intra-articular fractures of the base of the proximal phalanx of the thumb occur in axial (resulting in comminuted fractures of the base) and lateral deviation traumas (collateral ligament avulsion fractures). ORIF is often necessary in comminuted fractures to reduce eventually impacted fragments, and bone grafting is advocated to buttress articular fragments and promote bone healing. The surgical approach is usually dorsal between the two thumb extensor tendons, and the MPJ capsule is opened to check correct reduction of the joint surface. The first metacarpal head may be used as a template to reduce the depressed articular fragments, and the void distal to the fragments is filled with cancellous bone grafts from the distal radius. The fragments may be stabilized with K-wires or screws, and plate fixation is usually necessary to further buttress the fragments and to fix the articular fragments to the shaft of the proximal phalanx.
Avulsion fractures of the ulnar collateral ligament are frequent and may result in thumb MPJ instability as in ligamentous skier’s thumb injuries. Fragments are of different size and are often displaced and rotated, but it is not possible to determine from radiographs whether a complete rupture or avulsion of the collateral ligament has occurred in addition. Only if the fragment (which may be very small) is displaced proximal to the adductor aponeurosis, a bony Stener lesion can be assumed from the X-ray and open repair with reinsertion and fixation of the fragment and the ulnar collateral ligament is mandatory (Fig. 7.69). In all other cases, stability of the ulnar collateral ligament is tested in 30° of MPJ flexion as there may exist a combination of a minimally displaced fragment and a complete ligament avulsion. With the force exerted during manual testing, no Stener lesion is provoked [116], and if ulnar collateral ligament instability is found open repair is indicated. With less than 30° of radial deviation (or less than 15° difference to the opposite side), nonoperative treatment with a short thumb spica or splint (immobilizing only the MPJ) is initiated even if the fragment is rotated and displaced, as long as it does not exceed 25 % to one-third of the joint surface [112, 117]. Under these circumstances, results after 6 weeks of immobilization and subsequent mobilization have been reported as excellent with return to previous work and normal sport activities, no instabilities, no significant differences in strength, and subjective satisfaction in all 28 patients [117]. Fibrous union is frequently seen with conservative treatment but was not associated to instability, degenerative changes or later surgical interventions. An indication for ORIF of ulnar avulsion fractures therefore exists if the fragment is larger than 25 % to one-third of the articular surface, is displaced proximal to the adductor aponeurosis, or if there is ulnar collateral ligament instability. Taping the MPJ is advisable when ball-sport activities are resumed.

Fig. 7.68
(a) Unstable dorsally angulated fracture of the proximal phalanx of the thumb. (b) Lateral view. (c) PA view. Six weeks following ORIF with radial position of minicondylar blade plate to reduce extensor tendon adhesions. Final extension/flexion of IPJ 0/0/50 despite some residual deformity

Fig. 7.69
(a) Displaced avulsion fracture (with 90° rotational displacement) of the ulnar collateral ligament with ulnar collateral ligament instability of the MPJ. (b) Lateral view, (c) PA view. Eight weeks following open screw fixation
As the impact of the ball on the thumb in ball sports is hardly controllable and the thumb cannot be taped to an adjacent finger, it has to be protected even after stable lag screw or plate fixation. Early active mobilization under supervision of a hand therapist is encouraged following internal fixation, but ball-sport activities should only be resumed if the radiographs taken at 4 weeks show adequate bone healing and a removable splint is recommended during another 3–4 weeks. At that time, radiographs should confirm stable healing of the fracture. Taping may be sufficient for light activities at noncompetition level and is helpful after splint removal.
Key Points
Standard anteroposterior and lateral X-rays of the thumb only are mandatory to depict fractures of the phalanges. Extra-articular fractures can often be treated with splints if displacement is minimal. In intra-articular fractures, open reduction and internal fixation is recommended if the fragments include more than 25 % of the joint surface and step-off is more than 1 mm. In avulsion fractures of tendon or ligament insertions, internal fixation is recommended if there is volar subluxation at the IPJ in extensor tendon avulsions and ulnar collateral instability of the MPJ in fractures of the ulnar base of the proximal phalanx or if larger fragments are displaced.
Suggested Readings
Aitken S, Court-Brown CM (2008) The epidemiology of sports-related fractures of the hand. Injury 39(12):1377–1383
In this retrospective analysis of 1,430 hand fractures, more than 22 % were sports related. Football resulted in the highest number of phalangeal fractures, but in the thumb, rugby accounted for a higher percentage of phalangeal fractures than in the other digits.
Day Charles S, Stern Peter J (2011) Fractures of the metacarpals and phalanges. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH (eds) Green’s operative hand surgery, 6th edn. Elsevier/Churchill Livingstone, Philadelphia
Basic principles of fracture treatment in the hand are discussed in this chapter and details of surgical fixations are shown. One section deals with indications and techniques of thumb phalangeal fractures.
Sorene ED, Goodwin DR (2003) Non-operative treatment of displaced avulsion fractures of the ulnar base of the proximal phalanx of the thumb. Scand J Plast Reconstr Surg Hand Surg 37:225–227
Twenty-eight thumbs with ulnar collateral ligament avulsion fractures that were stable on clinical testing were treated conservatively with a spica cast. At 2.5 years 26 were pain free and no thumb was unstable.
7.3 Sesamoid Fractures
Renato Fricker8
Abstract
Sesamoid bones are found at the radial and the ulnar sides of the thumb metacarpophalangeal joint (MPJ) in almost all persons and are part of the complex ligamentous stabilizing system on the volar side of the thumb MPJ. Fractures are rare and occur in hyperextension injuries of the MPJ, e.g., when a ball hits the extended thumb. Pain, swelling or bruising, and local tenderness on the volar side of the MPJ are typical, and if standard posteroanterior and lateral radiographs do not show a fracture, additional radial and ulnar oblique views should be obtained. Stability of the volar plate and the collateral ligaments has to be tested, as additional lesions may be present. If the volar plate is intact in type 1 fractures, treatment is conservative with a splint or cast in 30° of MPJ flexion to approximate the fragments. In type 2 injuries with volar plate instability, a suture repair of the palmar plate and the sesamoid bone is recommended, and the MPJ is immobilized with a splint in slight flexion. Taping is used to prevent hyperextension during the first weeks, and recovery of a pain-free fully mobile and stable MPJ can be expected.
The sesamoid bones got their name from their appearance resembling the Sesamum indicum grains. Sesamoid bones are found both at the radial and the ulnar sides of the thumb metacarpophalangeal joint (MPJ) proximal to the A1 pulley in almost all persons according to different dissections and X-ray studies [118]. Ossification starts at puberty and may be incomplete in rare cases as confirmed by bipartite sesamoids in 0.6–6 % of cadaveric hands [119]. Their precise functions remain debatable, but as the flexor pollicis brevis (radial) and the adductor pollicis (ulnar) tendons have their insertion on the sesamoids, they are thought to modify pressure, diminish friction to protect the tendons from excessive wear, and alter the direction of the muscle pull [120]. They are part of the complex ligamentous stabilizing system on the volar side of the thumb MPJ: accessory collateral ligament insertion on their lateral margins, distal and proximal palmar ligaments (connecting them to the base of the proximal phalanx and the metacarpal head, respectively), and transverse palmar ligament (intersesamoid ligament) which prevents the two sesamoids from separating when they glide on the radial and ulnar condyles of the first metacarpal head (Fig. 7.70).
Fig. 7.70
Anatomy of the sesamoid bones with inserting ligaments. The insertions of the flexor pollicis brevis and the adductor pollicis tendon on the lateral sides of the radial and ulnar sesamoid bones, respectively, are not shown. 1 Ulnar collateral ligament, 2 accessory ulnar collateral ligament, 3 proximal palmar ligament, 4 distal palmar ligament, 5 palmar transverse ligament (intersesamoid ligament), 6 ulnar sesamoid, 7 radial sesamoid (G. Chick © 2012, all rights reserved)
Fractures of the thumb MPJ sesamoids are rare and are related to hyperextension injuries of the MPJ. In athletes, they occur both following a fall on the hand and thumb and following direct impact, e.g., of a ball to the extended thumb. A direct trauma with an impact to the sesamoids has been reported being responsible more often for fractures of the radial or both sesamoids [121], but a detailed analysis of the injury mechanism (if described at all) cannot exclude a thumb hyperextension mechanism in all these cases. Fractures occur more frequently at the ulnar sesamoid [119, 122].
Typical clinical signs of a sesamoid fracture are pain on the volar aspect of the thumb MPJ and swelling and hematoma at the same site with reduced active mobility. Bruising may extend along the flexor pollicis longus tendon sheath [123]. The stability of the ulnar and radial collateral ligaments of the MPJ must be evaluated, as combined injuries may occur (Fig. 7.71). As the sesamoids are part of the volar plate complex, its stability has to be tested carefully. Standard posteroanterior and lateral radiographs may not show the fractured sesamoid adequately, so additional radial and ulnar oblique views should be obtained to confirm or exclude a fracture [119]. The fractures may be undisplaced or minimally displaced, or the fragments may be separated several millimeters due to muscle pull especially if the volar plate is also ruptured. Arthrography has been effective in confirming this combined injury [124]. As two sesamoid bones are present in close to 100 % of MPJ, they should not be mistaken as avulsion fractures from the proximal phalangeal base or the metacarpal head, but fractures of a sesamoid may be mistaken as a bipartite sesamoid, which only can be assumed if the edges of bone fragments are smooth with a cortical bone surface. CT scans will distinguish between a fractured or bipartite sesamoid if necessary.


Fig. 7.71
Multifragmentary fracture of the ulnar sesamoid bone of the thumb MPJ following hyperextension injury. (a) PA view, (b) lateral view, (c) oblique view
Potential volar plate or collateral ligament instability is tested clinically, but if not conclusive stress views, arthrography, ultrasound, or MRI can be performed. Patel established a simple classification of sesamoid fractures of the thumb MPJ (Fig. 7.72) where stability testing of volar plate allows the fracture to be classified into type one with the palmar plate intact or type 2 when the palmar plate is ruptured [122]. Whereas in type 1 injuries the thumb MPJ remains in its standard resting position in slight flexion and the ability to flex the MPJ is preserved, the additional volar plate insufficiency in type 2 injuries allows a hyperextension position and active flexion of the MPJ is lost. Treatment of sesamoid fractures depends on the presence of additional soft tissue instability and not on the fracture itself.
Fig. 7.72
Patel classification of thumb MPJ sesamoid bone fractures. Type 1 fractures are stable due to the intact volar plate, whereas, in type 2 fractures, the additional volar plate rupture causes volar instability of the MPJ. 1 Proximal palmar ligaments, 2 distal palmar ligaments, 3 volar plate with intersesamoid ligament, 4 ruptured volar plate (G. Chick © 2012, all rights reserved)
The aim of treatment in the acute situation is to relieve pain, and a thumb splint is applied in slight flexion of the MPJ. If necessary, stability testing (collateral ligaments and palmar plate) is repeated after a few days. The final goal of treatment is complete recovery of function, which, in the thumb MPJ, is more dependent on stability than mobility. Type 1 sesamoid fractures are therefore treated conservatively with a splint or cast in 30° of flexion of the thumb MPJ to relieve the pull of the inserting muscles and to approximate the fracture fragments [125]. The wrist and thumb interphalangeal joints are not immobilized, and after 2–3 weeks, mobilization of the MPJ is encouraged, but a removable splint is applied to protect the MPJ from hyperextension during another 3–4 weeks. Athletes may prefer taping only in order to return to sport activities earlier, and good functional results can be achieved with both techniques [119].
If the palmar plate is ruptured with hyperextension instability of the MPJ in a type 2 injury, surgical treatment is preferred, but details of the procedure are not reported in the current literature. A volar Bruner incision is made with the apex radially in the proximal MPJ crease, and the A1 annular pulley is opened for better visualization of the volar plate. The main goal is the restoration of palmar MPJ stability, so a combined repair of the palmar plate and the sesamoid bone is necessary using nonabsorbable sutures. The size of the sesamoid fragments precludes internal fixation with screws. Postoperative treatment includes a removable splint in slight MPJ flexion, early active mobilization depending on the intraoperative stability, and the prevention of hyperextension during the first 8 weeks (splint or taping).
In the case of relevant ulnar collateral ligament instability with a suspected Stener lesion in addition to the sesamoid fracture, open repair of the ulnar collateral ligament and the sesamoid bone can be performed through the same ulnar-sided approach as done in one of our cases.
The MPJ may be painful for several weeks or months, but final results after conservative and operative treatment are reported as good with painless full range of motion of the thumb MPJ and without signs of instability [119, 122, 125, 126]. If, however, the metacarpo-sesamoid joint is painful with posttraumatic osteoarthritis, excision of the sesamoid results in pain relief and preservation of stability and mobility [127].
Key Points
Fractures of the sesamoid bones of the thumb MPJ occur in hyperextension injuries. Fractures are classified according to Patel, and simple fractures of the sesamoids are stable (type 1) and are treated with a splint or cast in slight MPJ flexion to approximate the fragments and to prevent repeated hyperextension. Type 2 fractures with additional rupture of the volar plate result in volar instability, and surgical repair is indicated.
Suggested Readings
Dong PR, Seeger LL, Shapiro MS, Levere SM (1995) Fractures of the sesamoid bones of the thumb. Am J Sports Med 23(3):336–339
Eight cases of thumb MPJ sesamoid bone fractures were treated conservatively with a splint in 30–40° of flexion in six patients and with taping alone in two athletes. Seven patients had clinical follow-up at 6–8 weeks and showed full range of motion and pain free function.
Ishizuki M, Nakagawa T, Ito S (1994) Hyperextension injuries of the MP joint of the thumb. J Hand Surg 19B(3):361–367
Twenty-six cases of thumb MPJ hyperextension injuries are reported. In addition to sesamoid bone fractures (all treated conservatively), dorsal dislocation (with volar plate rupture which can easily be reduced closed) and locking of the thumb MPJ (which most often necessitated open reduction) are described.
Patel MR, Pearlman HS, Bassini L, Ravich S (1990) Fractures of the sesamoid bones of the thumb. J Hand Surg 15A(5):776–781
Twenty-five cases of sesamoid fractures of the thumb MPJ are reported from the literature, and three own cases are added. Immobilisation in slight flexion in type 1 injuries with palmar plate intact is suggested whereas surgery is recommended in type 2 injuries with palmar plate rupture.
7.4 Fractures in the Digits
7.4.1 Fracture in the Digits: Is There a Place for Nonsurgical Treatment in Athletes?
Abstract
The hand should be moved as soon as possible after a fracture to avoid stiffness and to return the ball player to sport at the earliest opportunity. Furthermore, the fracture must heal in a proper position. In many cases, this goal is best achieved with surgery. However, surgical treatment of finger fractures carries a risk of complications such as infection and stiffness, which could make the athlete worse. Many fractures can be treated without surgery, and indeed, some (such as mallet fractures) may recover better without surgery than with surgery. Nonoperative treatments include benign neglect, specific splints, and neighbor strapping. During nonoperative management, the treating doctor must be vigilant for a change in position which would then require surgical correction and stabilization.
7.4.1.1 Background
A ball player may fracture their hand during sport or away from sport; the athlete will need the quickest recovery so that he can return to training and competition as soon as possible. If the fracture is treated poorly, then the hand may be compromised such that the original performance is never resumed. Meticulous assessment and matching treatment to the athlete’s needs is essential. While many fractures do require surgery, some do not. Any surgical operation has the capacity to make an athlete worse rather than better if it is performed poorly or if there is an unexpected and unavoidable complication. Therefore, it is essential to understand the role of nonsurgical management in the ball player.
7.4.1.2 Principles of Hand Fracture Treatment
The sooner a hand is moved after injury, the less likely it is to become stiff and the sooner function will recover. This is the fundamental principle of managing hand fractures. Furthermore, for the ball player, the soonest return to play will maintain practice and skills. If the hand can be moved very soon after the injury without surgery, and if the bones then heal in a proper functional position, then surgery is not usually required. If the opposite is true, then surgery may well be required.
Aims of Managing a Hand Fracture
Prevent hand stiffness
Maintain a proper position
Enabling the earliest possible return to normal function
Avoid treatment that could compromise function
7.4.1.3 The Disadvantages of Surgery
The aim of surgery is simple and is the same as nonoperative treatment: to hold a fracture in its original position, firmly enough to allow the hand to move without fear of the bone displacing again into an unsatisfactory position. In the ball player, training and sport can therefore be resumed at an early stage; this is most desirable. Surgery can contribute to this aim.
However, any operation carries a small risk of an unexpected and unavoidable natural problem. Infection can affect any surgical wound. When metal is present, then infection can be more likely to occur and hardware to eradicate. Just occasionally, the entire hand can become stiff, shiny, and painful – a condition known as dystrophy. These complications can make the athlete worse.
Surgery does not make a bone heal quicker. Indeed, exposing the fracture can diminish the healing rate. This is because stripping away the bone lining (periosteum) will reduce the blood supply to the bone. Surgery will also remove the normal physiological substances around the fracture that enhance wound healing.
Poor surgical technique is particularly hazardous for the patient. If the surgical implants hold the bone apart rather than properly apposed, then bone healing will be retarded and may not even occur. Clumsy surgery may reduce the rate of recovery, due to surgical scarring around tendons, damage to vulnerable nerves, or inhibition of healing. The surgical wound may fail to heal if the skin incision is not planned carefully enough to respect the blood supply to the wound. While infection may be unavoidable, it is more likely if proper sterile operating room procedures are overlooked.
If a patient has an operation to mend a fracture, that will require either the penetration of the skin with metal wires (K-wires or external fixator pins) or opening the skin and displacing the tendons to mend the bone. Surgery will always risk adherence of the metal to the tendons and the tendons to the bone due to scar tissue. It is essential that the fracture is fixed firmly enough to allow immediate movement. Early movement will prevent the inevitable scar tissue from restricting motion. If the metal fixation is too weak such that despite surgery the fracture fragments remain unstable and vulnerable to displacement when moved, then the hand will need to be immobilized on a splint until the fracture starts to heal. This will predispose to considerable stiffness as the swelling and scarring from surgery cannot be assuaged by early movement; rather, there will be excessive scarring around the fracture and displaced tendons. The outcome will probably be worse than if no surgery had been performed. A common reason for instability despite surgery is that there are too many fragments to capture with the fixation device – a comminuted fracture.
Complications of Surgery
Natural complications:
Dystrophy
Infection
Stiffness
Surgical complications:
Reduced healing
Stripping of periosteum
Inadequate fixation
Distraction
Finger stiffness
Wound failure
Infection
Deformity
Nerve damage
7.4.1.4 Stable Fractures: Nonsurgical Treatment
The benefits of surgery depend on the type of fracture and the needs of the ball player. The hand surgeon will assess each case according to these conditions. If a fracture is stable (which means that the bone fragments are continuous and interlocked so they are unlikely to change position regardless of movement by the patient), surgery is usually not required. The risks of surgery outweigh the gains.
Indications and Contraindications for Nonsurgical Treatment
Indications for nonsurgical treatment:
Stable fracture that will not displace despite early movement
Current infection
High risk of complications
Fracture pattern not amenable to surgical fixation
Patient unfit for surgical intervention
Patient prefers to trade longer recovery for lesser risk
Contraindications to nonsurgical treatment:
Deformed finger that cannot be reduced and held with splint
Displaced joint (articular) fractures
Open fracture (i.e., associated skin wound)
Associated tendon injury
Unstable fracture that cannot be controlled by splint
Impracticality of repeated clinical examination and radiographs
Relative indications for nonsurgical treatment:
Reasonable expectation that nonoperative treatment will allow an equivalent return to sport and equivalent function to surgery
Nondominant hand
Position of Safe Immobilization
Fractures of the metacarpals and phalanges can be treated in a splint made of plaster or plastic, which holds the hand in the position of safety. In this position, the metacarpophalangeal joints (MCPJs) are held at 70–90° of flexion and the proximal interphalangeal joints (PIPJs) are held straight. In this position, the collateral ligaments of the MCP joint and the palmar plate of the PIP joints are held at their maximum length. The collateral ligaments and palmar plate are the strong structures to the side and front of the joint, respectively, which prevent sideways or backward movement. If the hand is immobilized in the opposite posture, with the MCPJs straight and the PIPJs flexed, then the ligaments start to contract. This can lead to permanent stiffness such that the MCPJs cannot be flexed fully and the PIP joints cannot be extended fully. As a first aid measure, almost all hand fractures can be put in this position of safe immobilization, until a decision is made about the most suitable management of the fracture, tailored to the ball player’s needs. While in this large stiff splint, the hand should be elevated to avoid swelling which will exacerbate the risk of hand stiffness. The splint should be discarded in favor of a more specific treatment plan that allows early mobilization as soon as practical (Fig. 7.73).


Fig. 7.73
Position of safe immobilization – different materials
Benign Neglect
An example is the fifth metacarpal neck. The head of the fifth metacarpal is formed by a 270° sphere; this allows the finger to hyperextend at the knuckle by 40–60° in most individuals. When the neck breaks, the head tends to flex forward. However, the fracture heals within 4–5 weeks, and some residual forward angulation is well tolerated by the surplus arc of joint cartilage so that a full functional range of movement recovers. Pain usually settles within 2 weeks or so; there is little advantage in surgical stabilization for many ball players. However, if the head is angulated too far forward, it will be noticed when holding a racquet or when using the palm as a bat. Returning the fracture to a proper position until healed will improve the outcome. The safest way is to pass a surgical wire from the base of the metacarpal so the tip holds the neck (the bouquet technique). The wire does not interfere with the tendons but is not strong enough to allow immediate resumption of ball sports after about 5 weeks when the wire is removed under a simple local anesthetic.
Fractures of the middle or ring metacarpals if relatively undisplaced are splinted by the adjacent metacarpals. The hand can be moved immediately with little fear of displacement of the fragments. For the nondominant hand in racquet sports, there may be little to gain from surgical intervention. In the dominant hand, however, surgical stabilization is likely to restore comfortable grip to the hand 2 or 3 weeks earlier.
Simple Splints
An example is a fracture of the distal phalanx. These commonly occur by stubbing of the tip of the finger. The shaft and distal tuft break. The fracture is usually stable as it is splinted by the patient’s own fingernail. A protective thimble is all that is required to protect from inadvertent knocking. For almost all ball sports, immediate return to play is possible.
Neighbor Strapping
Undisplaced stable fractures of the proximal phalanx and middle phalanx should not be operated upon. There is a high chance of stiffness if these fractures are held with a plate because the bone and tendon and plate tend to adhere to each other. The digit can be strapped to the adjacent digit with a tape – this gives some stability and protection, as well as encouraging movement by passive encouragement from its neighbor (Fig. 7.74). However, even a minor rotational deformity in a proximal phalanx will impede grip around a racquet; as the finger makes a fist, the finger deviates and catches on the adjacent finger. Surgery to the proximal phalanx in particular carries a risk of stiffness due to scarring between the tendon, the metal device, and the bone. However, the need for a perfectly straight finger so that ball playing may outweigh this risk. The fixation must be technically excellent and must be strong enough to allow immediate movement.
Fig. 7.74
Neighbor strap – flexion and extension. Note the blood in the palm from local anesthetic injection for fracture manipulation
Collateral ligament injuries tend to heal well. Neighbor strapping will support the fracture while it heals, yet allowing full flexion-extension and avoid a difficult operation (Fig. 7.75).


Fig. 7.75
Collateral avulsion little finger proximal phalanx
Mallet Splint
A mallet fracture occurs when the extensor tendon (which elevates the tip of the finger) pulls off the piece of bone to which it attaches. The finger tip droops down. If the tip is held up with a fashioned splint for 6 weeks, then in 90 % of cases, the bone will heal and excellent function is restored. The splint will not interfere with most ball sports. Surgery is fraught with complications, and there is no good evidence that there is an earlier return to sport or a better long-term outcome. Indeed, stiffness and wound problems are more likely with surgery. The exception is when the fracture is displaced so that the joint is no longer congruous. Surgery is then needed to restore the joint contour (Fig. 7.76).
Fig. 7.76
Mallet fracture and mallet splint
Specific Splints
Certain injuries need particular splints if they are to be managed nonoperatively. The ulnar collateral ligament of the thumb can be avulsed if the ball player lands on the side of the thumb tip – the injury is sometimes called a skier’s thumb. If there is a substantial displaced fragment, then early reattachment with a screw will allow an earlier return to function. However, a stable undisplaced fracture can be managed in a splint. The ligament is the same length (isometric) whether the thumb is flexed or extended so the splint allows movement to avoid stiffness but protects against sideways pinch that would cause pain and perhaps displace the fragment (Figs. 7.77 and 7.78).
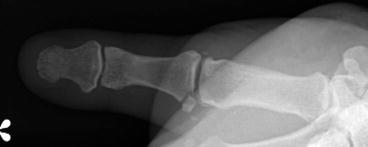

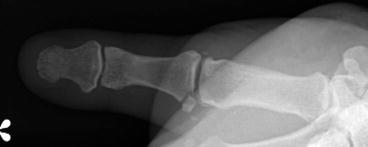
Fig. 7.77
Thumb ulnar collateral ligament avulsion

Fig. 7.78
Protective splint for ulnar collateral avulsion
7.4.1.5 Contraindications to Nonsurgical Management
Failure of Nonoperative Management
If a fracture is treated nonoperatively, the treating doctor must be aware of the possibility that the fracture could change position before it has healed. A fracture which is initially thought to be stable and undisplaced may in fact be rather more unstable than was initially thought. It may change position simply by the joint and tendon forces applied during early movement; the fracture may displace if it is inadvertently knocked during return to play. Therefore, whenever a fracture is treated nonsurgically, the treating doctor must be vigilant with meticulous clinical examination and repeated radiographs during the first 3 weeks.
Earlier Return to Play in Stable Fractures
Surgery can, for certain fractures, bring forward return to training and competition by a few weeks. If an athlete’s ball sport requires him or her to return to impact or repeated/forceful gripping, then even with a stable fracture there may be such inhibition by pain, or vulnerability to sudden displacement from unexpected forces, that surgical fixation may be considered. Strong accurate surgical fixation will allow the hand to be moved immediately and training resumed within a few days for all but the most strenuous of activities. Surgery must only be undertaken if the patient is aware of the small risk of a problem and that the gains would only be for a few weeks at most. The surgeon must be certain that the fracture can be fixed with sufficient strength. The wound must of course be kept protected which may not be possible for sports such as rugby in which contamination is possible. If so, avoidance of contact for a period of 10–12 days until the wound is physiologically sealed is wise.
Open Fractures
If the skin is breached when a bone is fractured, then the outcome is severely compromised. The fracture is far more likely to become infected, and the finger is far more likely to get stiff. The fracture must be cleaned with copious amounts of sterile fluid. Some fractures do not need surgery if they have a minor soft tissue wound and if the fracture is stable; however, if the fracture is unstable, it will require osteosynthesis; tendon injuries need immediate strong repair to allow early mobilization. The wound must be covered primarily, using a skin flap if needed.
7.4.1.6 Conclusion
The reliability and safety of surgical osteosynthesis continues to improve. Meticulous rigid fixation of an unstable hand fracture will usually give the athlete the earliest return to function. The earliest return is desirable for the athlete’s performance as well as for his team and sponsors. However, surgery to the hand carries some risk of infection, stiffness, and nonunion; many fracture configurations can be managed perfectly well with careful rehabilitation and splinting.
Key Points
Nonsurgical treatment has a proper role in athletes.
Careful and logical splinting for some injuries is equal or preferable to surgery.
Surgery can bring forward return to play in ball sports.
Open fractures and unstable fractures usually require surgery.
7.4.2 Management of Suspected Finger Fractures
Abstract
Finger fractures are common in ball sports and mainly affect the phalanges, especially those of the fourth and fifth fingers. The context, the mechanism of onset, and the presence of pain and eventual deformities are important clues to suspect a fracture. However, in the absence of displacement, the diagnosis can only be made by X-ray. A number of precautions are required during the more or less urgent transportation of an athlete injured on the playing field. The player can rarely resume the game. At the emergency department, conventional radiography, which is routinely performed after a trauma, can reveal or confirm the fracture. Through immobilization in anatomical position, the administration of analgesics, and measures for edema reduction, the specific expert management can be postponed.
7.4.2.1 Introduction
In sports, fractures are much more common than dislocations (71 % vs. 4 %) and mainly affect the phalanges (54.1 %), especially those of the fourth and fifth fingers [128]. Young athletes are particularly at risk, with 22.4 % of all finger injuries due to sports. The 10- to 19-year-old age group is the most affected in ball sports, with the highest incidence of finger fractures occurring in football and basketball. Athletes often initially neglect their injuries, hoping for spontaneous recovery. With this delay, treatment becomes increasingly complex with mixed results. Therefore, the importance of early management must be emphasized and guided by an informed environment to avoid underestimating the lesion, as well as to avoid long-term functional repercussions (especially in case of phalangeal fractures).
7.4.2.2 On the Playing Field
The context, the mechanism of onset, and the presence of pain and deformities are important clues for the diagnosis. However, in the absence of displacement, a fracture may be initially misdiagnosed. The diagnosis can only be later confirmed by X-ray. The player can rarely continue playing. The priority is to set the finger in the best possible conditions during transportation to the emergency department. Basic immobilization, analgesics, and the application of cold can reduce the pain. The patient should fast, by principle. A number of emergency situations requiring a speedy evacuation from the field must be identified.
Emergency Situations
Open Fractures
In case of open fracture, a number of factors must be identified and reported to the emergency team:
The degree of fracture openness
The degree of soiling
The eventual presence of foreign bodies (glass, metal, gravel, etc.)
The precise time of occurrence
The wound must first be disinfected. Then, a nonadherent dressing should be placed over the injury, together with sterile gauze. Circular bandages should be avoided around a finger, and the neighboring finger should be included in the dressing separated from the injured finger by a dry gauze. The whole should be immobilized with a semirigid transportation splint. An IV line should be established, after which the fasting patient should be transported to the care center.
The diagnosis should then be confirmed by X-ray. Tetanus immunization should be verified. A basic but accurate assessment should identify specific surrounding soft tissue lesions, such as nerves, arteries, tendons, and ligaments, which is critical for choice of a therapeutic approach. A prophylactic antibiotic therapy should be started, depending on the degree of soiling.
The treatment should be started urgently to minimize the risk of infection. Debridement and cleaning of the fractured site and associated lesions are essential before repair. There is no room for conservative treatment in these fractures.
Compartment Syndrome
At the level of the hand, an acute compartment syndrome usually occurs following a crush injury. Muscle ischemia can then develop because of the abnormal increase in pressure within the inextensible compartments of the intrinsic muscles. Surgery should be performed urgently because the lesions become irreversible within a few hours.
Pain is disproportionate to the type of injury. The muscles are stretched (Fig. 7.79), and nerve disorders such as paresthesia, followed by sensory and motor deficits, can develop. Pulse is present, unlike in case of ischemia. There is also pain during passive extension of the muscles.


Fig. 7.79
Crush injury of the hand with compartment syndrome. (a) Volar view; (b) dorsal view; (c) side view. Note the hand thickening
Emergency treatment consists of surgical decompression, which requires large incisions to decompress all compartments. In the absence of immediate treatment, muscle necrosis, sensory–motor nerve palsy, and Volkmann’s contracture can develop.
Devascularization
Devascularization usually affects the ring finger. The diagnosis is based on symptoms such as a cold, lifeless finger with a pulp that does not reshape after pressure. Treatment is urgent. After bone stabilization, the restoration of arterial continuity will determine the future of the finger.
Puncture by Human Teeth
A punch, accidental or not, to a tooth, with the metacarpophalangeal (MCP) joint flexed, may be responsible for a metacarpal head fracture. The skin breach is usually small. The risk of septic arthritis is very high. Debridement should be performed urgently, together with antibiotic treatment against anaerobes. The treatment follows same principles of open fracture treatment if no infection has been detected.
Closed Fractures
Context
In most cases, a fracture occurs during a particular game phase, and the experienced eye of the club physician or physiotherapist is crucial in anticipating a possible lesion. For instance, in rugby, fingers are frequently injured during the scrum, lineout. or tackles. Basketball, volleyball, and handball injuries occur mostly when blocking. However, a fall or direct contact with an opponent may also cause fractures. Also, the entourage of the athlete may be alerted by the speed of the ball hitting the finger. However, high-velocity injuries are less frequent on the field than in road accidents [129].
Mechanism of Deformity
Finger fractures may follow axial trauma (direct contact with the ball, fall on the finger) or rotating trauma when grasping (Fig. 7.80). Phalanges and metacarpals are similar in their susceptibility to fracture due to their exposed position.
Fig. 7.80
Example of finger trauma in ball sports. (a) Axial trauma due to direct contact with the ball, responsible for a P3 fracture. (b) Traumatic torsion (G. Chick © 2012, all rights reserved)
Metacarpal Fracture
They follow direct or indirect trauma usually by an axial force transmitted from the MCP joint in the axis of the diaphysis. The action of the flexor tendons and interosseous muscles causes a volar flexion of the distal bone fragment, with dorsal opening of the fracture site (Fig. 7.81). This deformity is even greater in case of fractures involving the metacarpal neck [129]. The interosseous muscles also induce an axial rotation of the distal fragment. The second and third metacarpals tend to pronation (ulnar rotation), while the fourth and fifth metacarpals tend to supination (radial rotation).
Fig. 7.81
Mechanism of deformity of the finger after fracture of the metacarpal. 1 Flexor tendon, 2 extensor tendon, 3 lumbrical muscle, 4 interosseous lumbrical muscle (Inspired by Merle and Voche [130]) (G. Chick © 2012, all rights reserved)
Axial trauma on the metacarpals of the fingers may also cause fracture–dislocations of their bases. The volar bone fragment remains attached to the carpal bones. Sometimes, the crush causes multiple fractures, with lesions of the soft tissues (Fig. 7.79).
Particularities of First Metacarpal Fractures
Extra-articular fractures (metaphyso-diaphyseal) cause posterior angulation with flexion adduction of the distal fragment.
Articular Bennett-type fractures are fracture dislocations where a proximal anterior fragment separates and remains attached to the trapezium and the second metacarpal. The first metacarpal is pulled dorsally and proximally by the action of the extrinsic muscles especially the APL. The mechanism of injury is usually indirect by axial trauma to the partially flexed thumb column – the classic boxer’s fracture.
Phalangeal Fractures (Extra-articular)
The type of fracture depends on the position of the finger, the direction, and the magnitude of the force applied:
In case of direct trauma, the crush is responsible for associated soft tissue injuries (skin, extensor tendon, nail bed, etc.)
In case of indirect trauma, spiral fractures are the result of a torsion, unlike transverse fractures, which occur after a cantilever (three-point bending force) action. Spiral lesions are unstable and occur on a semiflexed finger.
Diaphyseal P1 Fracture
The proximal fragment is flexed by the action of the interosseous muscles. The distal fragment is extended by the lateral slips of the extensor apparatus, with volar opening of the fracture site (Fig. 7.82). This displacement may be accompanied by bone shortening which causes a swan-neck deformity of the finger due to laxity of the extensor mechanism.
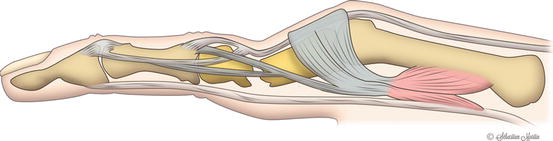
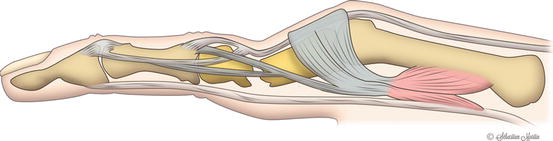
Fig. 7.82
Displacement in volar angulation of P1 fractures by the action of the intrinsic muscles and lateral bands of the extensor mechanism (Inspired by Merle and Voche [130]) (G. Chick © 2012, all rights reserved)
Diaphyseal P2 Fracture
When the fracture line is proximal to the insertion of the superficial flexor tendon, the proximal fragment is extended by the median slip of the extensor, and the distal fragment is flexed by the action of the superficial flexor. The deformity results in an angulation with dorsal opening (Fig. 7.83). When the fracture line is distal to the insertion of the flexor tendon, the proximal fragment switches to flexion and the distal fragment to extension, resulting in a deformity with volar opening (Fig. 7.84).
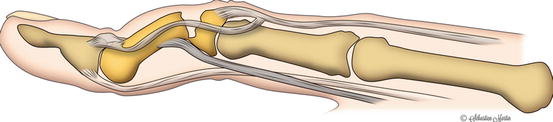
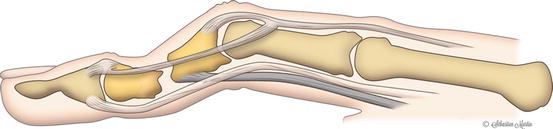
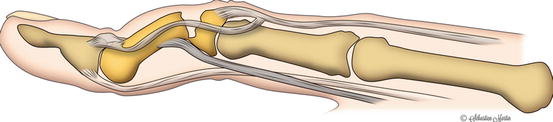
Fig. 7.83
Dorsal angulation deformity of P2 fractures when the fracture line is proximal to the flexor digitorum superficialis insertion (Inspired by Merle and Voche [130]) (G. Chick © 2012, all rights reserved)
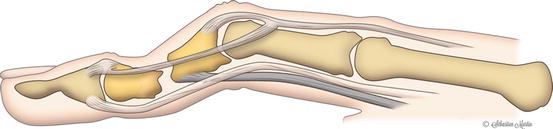
Fig. 7.84
Volar angulation deformity of P2 fractures when the fracture line is distal to the flexor digitorum superficialis insertion (Inspired by Merle and Voche [130]) (G. Chick © 2012, all rights reserved)
Diaphyseal P3 Fracture
In most cases, diaphyseal P3 fractures are due to a crush injury (Fig. 7.85).
Fig. 7.85
Subungual hematoma: X-rays should be systematically performed. (a) Clinical aspect; (b) X-ray lateral view; (c) X-ray PA view
Phalangeal Fractures (Articular)
Condylar Fractures
These types of fracture usually occur during sports. Tension with rotation through the collateral ligament results in an oblique fracture, and compression with subluxation causes coronal fractures (Fig. 7.86).
Fig. 7.86
Direction of forces transmitted determines the condylar fracture configuration (Inspired by Merell et al. [131]) (G. Chick © 2012, all rights reserved)
Fracture Dislocations of the Proximal Interphalangeal Joint
Concomitant lesions of soft tissues and ligaments are often found here. These injuries can result from axial compression, flexion or rotational forces, or a combination of both.
Fracture Dislocations of the Distal Interphalangeal Joint (Mallet and Jersey Finger)
The mallet finger is usually due to an axial trauma (reception of the ball to the tip of the finger – Fig. 7.80a). The rugby finger is usually due to a hindered movement of extension, such as during a tackle (Fig. 7.87).
Fig. 7.87
Jersey finger, left fifth finger. (a) Clinical aspect; (b) radiological aspect
Clinical Examination
In case of fracture without displacement, there is no obvious deformity of the hand or fingers. The diagnosis can be suspected by pain on palpation at the fracture site, localized edema, or a hematoma. The athlete may report an inability to move the injured part. The diagnosis is usually made secondarily, after systematic radiography, which reveals a bone or osteoarticular lesion.
Depending on the etiology, the deformity can be global (swollen hand) or localized to only one finger (large PIP). A severely traumatized hand quickly becomes wholly swollen. This edema accumulates in the free spaces of the back of the hand, creating a deformity with a wrist in flexion, MCP in extension, PIP in flexion, and thumb in adduction. This hand swelling may remain permanent in the absence of fast and appropriate care: The collateral ligaments of the MCP will retract, setting the joints in extension, and the volar structures of PIP will retract, fixing the joints in flexion [130].
A fracture can cause an angulation or rotational deformity of a finger. The tenodesis effect can help identify this deformity without active participation of the patient. This is particularly useful in the absence of compliance or coma. The long digital rays, seemingly parallel in extension, converge in flexion toward the tubercle of the scaphoid. In case of rotational disorder, the affected finger can drift above or below the adjacent finger (Fig. 7.88).
Fig. 7.88
Tenodesis effect showing a rotation disorder of the index finger in the context of a P1 fracture. (a): Wrist in flexion; (b) wrist in extension
Particularities of Metacarpal Fractures
Flexion of the MCP joints reveals the arc of the metacarpals.
In case of a metacarpal neck fracture, the head is displaced, and with substantial angulation, it will be palpable in the palm of the hand on the other side of the distal volar fold (Fig. 7.89).




Fig. 7.89
Fracture of the head of the M5 after axial trauma (fall on a tight fist). (a) Clinical aspect (note the early appearance of edema); (b) radiological aspect, PA view; (c) oblique view
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








