Fig. 8.1
Diagram showing that the collateral ligaments of MCP joint are taut in flexion and relaxed in extension (G. Chick © 2012, all rights reserved)
Posttraumatic Proximal Interphalangeal Joint (PIP) Stiffness
PIP Joint Flexion Contracture (Fig. 8.2)
Fig. 8.2
Preoperative PIP joint flexion contracture (a) and radiographic study (b)
It is one of the most common complications of trauma including tendon injuries, fractures, and soft tissue injuries such as post-joint dislocation ligamentous lesions. Chronic edema and immobilization always put the joint in a flexed position, with subsequent contracture of the palmar volar plate of the capsular ligament and the adherence of the collateral ligaments. Flexor tendon adhesions and palmar skin scarring also play important roles in contributing to joint stiffness.
PIP Joint Extension Contracture
Limitation of flexion of the PIP joint may be due to the impaired anatomical structures in the finger after dorsal skin laceration or direct trauma to the joint. These structures include [1] scarring of the dorsal skin and joint capsule [2], adherence of the central extensor tendon [3], contracted interosseous muscle or adherent interosseous tendon, and [4] contracted capsular ligament, particularly the collateral ligament. The consequent immobilization may also contribute to the resulting joint stiffness.
While they are not accepted universally, the classification schemes may help the treating physician consider general treatment strategies. For example, Salafia and Chauhan have proposed that contractures may be considered as follows: (a) mild (the PIP joint can be forcibly extended by stretching the skin and may respond to serial casting or splinting), (b) moderate (maximum possible extension remains 50–60° short of full), and (c) severe (the collateral ligaments and palmar plate are contracted so that the PIP contracture is 90° or more). Similarly, Tubiana et al. proposed a classification of Dupuytren’s disease, Grades I–IV (Table 8.1), based on the fixed angle of PIP contracture. Clearly, the more advanced the degree of contracture by either classification scheme, the more difficult the treatment.
Table 8.1
Classification of Dupuytren’s disease
Grade | Total fixed deformity (°) |
|---|---|
I | 0–45 |
II | 45–90 |
III | 90–135 |
IV | Over 135 (hyperextension at DIP joint is added to total deformity) |
Contracture of Distal Interphalangeal (DIP) Joint
Several etiologic factors for distal interphalangeal joint contracture have been reported, but little has been written about isolated DIP flexion contracture. The relationship between the flexor and extensor systems of the digits is both intricate and balanced, such that disruption can affect the entire dynamics of the finger. The development of fixed flexion contractures at DIP joint of the finger, if not detected early and prevented, can lead to abnormal mechanics, with resultant clinical signs and symptoms as severe as a swan neck deformity (Fig. 8.3).


Fig. 8.3
Swan neck deformity after DIP joint contracture in zone I—at 6 months
Volar Plate Avulsion Injuries (MCP, PIP, PID Joints)
Hyperextension of a finger joint, such as a dorsal dislocation, can injure the volar plate (Fig. 8.4a). Injury to the PIP joint is relatively common in athletics, especially ball sports, and collateral ligament damage is often present. The volar plate can be partially or completely torn, with or without an avulsion fracture. The subsequent loss of joint stability may allow the extensor tendon to gradually pull the joint into hyperextension, causing deformity. Maximal tenderness will be located at the volar aspect of the affected joint [4]. Full extension and flexion will be possible if the joint is stable. Radiographs may show an avulsion fragment at the base of the involved phalanx (Fig. 8.4b, c). It also usually involves a collateral ligament tear which often heals with abundant scar tissue leading to a chronic swelling on one side of the joint, which is permanent.
Fig. 8.4
Volar plate tear (a). Radiographic study showing avulsion fragment (b, c)
The severity of joint contractures and the resultant decreased joint ROM will not have the same impact on an employee or on an athlete, especially a ball athlete.
The useful range of motion of long fingers for ball catching depends on the sport, position of the athlete, and the diameter of the ball. Thus, the return to sport of an athlete with a PIP joint stiffness is earlier in a football player than a basketball or handball player who has more hand contact with smaller balls that require broader useful range of motion.
We consider that the last 5° of normal range of extension or flexion of MCP or PIP joints (Table 8.2) are functionally irrelevant and do not determine disability. The useful range of mobility in long fingers of the MCP joint ranges from 20/30° to 85° and of the PIP joint ranges from 40/50° to 95°. The functional ROM of DIP joint is less relevant and ranges from 15/20° to 70/75°.
Table 8.2
Normal range of motion (ROM) for each joint of long fingers
Joint | Movement | Normal ROM (values in °) |
|---|---|---|
MCP | Abduction | 0–25 |
Adduction | 20–0 | |
Flexion | 0–90 | |
Extension | 0–30 | |
PIP | Flexion | 0–120 |
Extension | 120–0 | |
DIP | Flexion | 0–80 |
Extension | 80–0 |
The indication for treatment is mainly functional in the adult ball athlete who must have a hand that strikes and receives effectively. It is also related to the affected finger since the second and third fingers are more functionally important than the fourth or fifth.
8.1.1.4 Management of Long Finger Stiffness
Joint contractures are an unwanted but common consequence of a variety of hand injuries.
Treatment used to improve the joint stiffness should be integrative and problem focused. Pressure therapy, active and passive mobilization through remedial activities, and corrective splinting should be started as soon as problems arise. The greater the joint limitation becomes, the longer the time the splint should be applied. Surgical treatment can be considered only after failure of a long period of conservative treatment.
Important factors to consider during preoperative planning are the duration and extent of the original deformity, the degree of progress with splinting, improvement reaching a plateau, patient tolerance of the treatment program, and the extent of residual deformity. Additionally, radiographic changes within the joint may also influence the choice of surgical technique.
Various surgical techniques have been described with differing results for the treatment of joint contracture. These techniques can be assigned to two categories: open release or distraction histogenesis.
The conventional treatment consists of performing a combination of arthrolysis, tenolysis, and occasionally, as a last resort, arthrodesis or replacement. Frequently, this does not achieve a good result particularly when there is a long delay since the injury [5, 6].
In case of a long-standing and severe MCP joint extension contracture, the joint is usually rigidly fixed by the collateral ligaments and dorsal capsule, requiring operative treatment. Approach is through a dorsal incision; the sagittal band hood fibers are retracted distally or cut if necessary, usually on the ulnar side. The dorsal capsule is transected and the joint is passively flexed. It is usually necessary to transect the ulnar or both collateral ligaments and occasionally necessary to free volar plate adhesions, too, in order to produce satisfactory flexion. Postoperatively, these joints should be maintained in full flexion for the first week; active mobilization is then begun. Night splinting or plaster may be necessary for several weeks.
The surgical approach to flexion contracture of PIP joint is well described in literature with checkrein ligament release. In the interphalangeal joints, adhesions and fibrosis occur proximal to the volar plate which does not flex; rather, it slides proximally and distally with flexion and extension of joint. There is normally no ligamentous structure between the volar plate and the assembly lines (two ridges on the volar lateral surfaces of phalanx); otherwise, extension would never be possible. The checkrein ligaments are two pathologic collagenous bands that form between the lateral proximal volar plate and the assembly lines after injury, usually pyramidal in configuration with thicker base attached distally to the volar plate and the thinner but longer apex attached proximally to the assembly line. Although some degree of fibrosis of the capsule and collateral ligaments occurs, the main structure preventing extension in the contracted interphalangeal joints is one or both checkreins. During checkrein resection procedure, the flexor sheath distal to the A2 pulley is exposed and opened. The nutrient artery from the digital artery to vincular system is identified passing beneath the checkreins, approximately 3 mm proximal to the edge of the volar plate (Fig. 8.5a). The proximal edge of the volar plate is identified, and checkreins are cut free from their broad triangular attachments to the proximal edge of the volar plate (Fig. 8.5b). As the collateral ligaments have approximately the same tension in flexion as in extension is almost never necessary to cut these ligaments; full ROM is usually possible once the checkreins are excised. The volar plate should be preserved in all cases. A moderate amount of gentle, passive extension may often be required to break up other small adhesions after checkrein resection, but full extension will occur. Watson et al. achieved full extension in 96 % of PIP joint contractures by checkrein resection as described. The joint is occasionally fixed in extension with K-wire to maintain the release. Following contracture release, the hand is immobilized in a bulky dressing reinforced with dorsal splint for 2–5 days, and when sutures are removed after 12 days, active motion is encouraged and corrective splinting applied [7].
Fig. 8.5
Diagram showing checkrein pathologic bands with transverse communicating vessels 2 mm proximal to the volar plate (a) and its complete excision (b). (G. Chick © 2012, all rights reserved). Inspired by Watson HK; Weinzweig J. Stiff Joints: Green DP, Hotchkiss R, Pederson W.; Green’s operative hand surgery, 4th edition, Vol. 1 (16), Churchill Livingstone, 1999
Extension contractures of IP joints rarely occur as pure joint contractures. They almost always involve structures other than the joint capsule. When performing a dorsal capsulotomy, a dorsolateral approach adequately exposes the hood. The transverse lamina of Landsmeer is divided and the lateral band elevated while preserving the central slip of extensor mechanism. The dorsal capsule is then incised and the joint passively flexed. In severe articular fibrosis, it is occasionally necessary to incise the entire capsule, divide both collateral ligaments, and free the volar plate adhesions.
Volar plate avulsion injuries are another common cause of loss of interphalangeal flexion. Reattachment of the volar plate is performed by formation of a cancellous groove on the volar proximal lip of middle phalanx, leaving the volar plate attached to the assembly line on one side. The joint is mobilized 3–5days postoperatively.
Stiffness or contracture of the DIP joint is seldom a problem unless there is a fixed flexion or hyperextension deformity. A fixed extension deformity can often be treated by dividing the most dorsal and lateral fibers of extensor tendon. Occasionally, complete transaction of the tendon is indicated. Late untreated mallet deformities are seldom adequately salvaged by tendon reconstruction; arthrodesis is frequently the procedure of choice.
However, single-stage surgical release of a digital joint contracture can be problematic. The amount of correction is often dependent on the status of the blood vessels and nerves. Overcorrection may cause cartilage necrosis and neurovascular overstretch and compromise, sometimes requiring subsequent amputation. Allodynia or algodystrophy may result from excessive nerve traction. In addition, there can be a lack of skin cover. Several studies have reported poorer results with increasing number of structures released at surgery. A recent report by Ghidella and coworkers [6] indicated the results of surgical intervention were dependent not only on the severity of contracture but also patient age, prior surgery, bony abnormalities, and the total preoperative arc of motion. The outcome of surgical release is discouraging [5, 6, 8]. This was noted by Foucher et al. and Koller et al. who attributed their poorest results (18–41 %) to digital tenolysis and capsulotomy performed around the PIP joint. The main risk to the patient is worsening of the situation if open surgery is unsuccessful [5, 8]. Foucher et al. noted that the fingers got worse in 12 % of cases after tenolysis. Ghidella et al. reported that the average improvement by open surgery was 8° in 68 PIP contractures. By grouping the patients into simple and complex cases, the average improvements were 17° and 0°, respectively, and emphasized that the best results were achieved in younger patients with less severe diagnosis and preoperative maximum flexion contracture of 45°.
In our experience, digital tenolysis and capsulectomy often mean more extensive surgery per se, which in turn increases problems associated with rehabilitation, with disappointing results.
In an effort to avoid the problems inherent in single-stage surgical releases, there have been many reports in the literature of various forms of primary treatment with dynamic tractions for acute fracture dislocation around PIP joint to avoid contracture, with promising results.
Joint distraction histogenesis techniques were first reported by Kolontay and Miloslavskii [9] in 1987 in the former Soviet Union; thereafter, lengthening techniques for soft tissues were sporadically reported in literature. Patel and Joshi described distraction for chronic fracture dislocations of PIP joint [10]; Bain et al. introduced dynamic extension technique using a compass hinge external fixator (Fig. 8.6) for treatment of PIP joint contracture with good results in two cases, and Houshian and Schroeder reported a mean of 38° of improvement of motion with a mean range of motion of 42° by dynamic extension correction technique using compass hinge external fixator in 27 patients with PIP joint contractures [11, 12].
Houshian and Schroder reported good short-term results using a monolateral frame (mini-Orthofix external fixator) for distraction correction in ten patients with chronic flexion contractures of the PIP joints with a mean range of motion gain of 54° (Fig. 8.7a–c) [13].
Fig. 8.7
Mini-Orthofix external fixator applied to PIP joint before correction (a) and after correction (b). PIP joint showing joint distraction before removal of the device (c) [12]
Over the years, skeletal fixation devices have relied on traction to create an extension moment at the PIP joint, thus applying distraction forces to the contracted tissues. Those devices relied on the principle of applying incremental stress (lengthening) to the contracted tissues, followed by a period of sustained, static force during which biologic creep was to occur. For many devices, that incremental stress was applied once to four times daily while the device was worn by the patient. Many previous devices were bulky and cumbersome and required fixation via transversely oriented hardware, making application to more than one finger difficult or impossible.
In 2005, Natividade da Silva et al. presented a case of a delayed (20 years) work-related traumatic flexion deformity of the PIP joint of the left index and middle fingers (Figs. 8.2 and 8.8) [14]. This was the result of a complete division of both flexor tendons of both fingers. The range of movements, both active and passive, were limited to 90/100° in the index finger and 95/100° in the middle finger.
Fig. 8.8
Preoperative view devices assemble (a) and result 6 months postoperative (b, c)
Following joint distraction using the lengthening device—AntãoTM, Portugal (Fig. 8.8a)—the patient was able to achieve an active and passive range of movements of 10/100° for the PIP joint of the index finger and 40/100° of the middle (Fig. 8.8b, c). The lengthening of the device was adjusted daily, up to maximum tolerated length, determined by appearance of moderate pain rather than skin perfusion. This clinical case shows the simplicity of our technique for the correction of joint contractures. In the presented case, the limitation of motion was attributed to adhesions of the flexor tendons and contracture of the ligaments and capsule of the affected joints. The progressive distraction of the joint allowed the lengthening of the contracted structures, with simultaneous rupture of the flexor tendon adhesions, without causing any damage to neural or vascular structures. Once the desired length is achieved, the fixator should be held in situ for a week and in long-standing contracture for 2 weeks. This allows the stretched tissues to mature in their new position and tissue inflammation to subside.
Temporary DIP joint flexion contracture following distraction correction of PIP joint is indeed a persistent problem that may be treated by hand therapy following deformity correction. We avoided this, by transfixation of DIP joint, using a Kirschner wire during the PIP joint distraction.
Distraction correction differs from extension correction using the compass hinge used by Bain et al. and Houshian et al. in that contractures are automatically corrected when the joint is subjected to gradual distraction. By distracting the offending structures responsible for contractures such as the capsule, the collateral ligaments and the palmar plate with the so-called checkrein ligaments are all lengthened, especially the volar structures, as the distractor is placed volarly. This distraction restores the length of the contracted structures.
More recently, Slater et al. described a new device, the Digit Widget (Fig. 8.9a, b), which is designed to correct PIP flexion contractures by a minimally invasive surgical technique. The device relies on the application of torque (the product of applied force times the lever arm length) to correct the angular deformity of the involved digit. It employs the principle that a gentle extension torque, applied continuously, stimulates the growth and elongation of contracted soft tissues, thus regaining, maintaining, or increasing extension of the joint. The Digit Widget is fixed to the dorsal aspect of the involved finger so it can be applied to more than one digit simultaneously. The application of continuous torque rather than application of intermittent sudden stress promotes subsequent creep—probably a better method for achieving that goal [15].
However, all these researchers excluded patients with flexion contractures combined with scar tissue around the joints from burn or crushing. To restore function in these patients, surgical release of all contracted tissue seems to be inevitable, and the resultant skin defect should be covered with stable skin to prevent recurrence. In 2009, Hahn et al. evaluate the effect of cross-finger flaps after extensive surgical release of contracted tissue and vigorous postoperative extension exercise for long-standing (10 years or more) severe flexion contractures with palmar scarring of the fingers. In these patients, tethering by the scar tissue and contractures of the palmar plates and collateral ligaments were the main cause of contracture. In all of our patients, surgical release of contracted tissue was inevitable to achieve maximal extension of the joint during the operation. The resultant skin defect was covered by a cross-finger flap, which was slightly larger than the defect from a neighboring finger to prevent contracture with time. By covering with stable and redundant skin, vigorous ROM exercises were possible just after healing of the operative wound. With this technique and postoperative management, a mean of 79.4° of increase of motion was achieved in comparison with preoperative values [16]. The authors believe that early vigorous exercises after covering the defect with stable skin led to excellent clinical results.
Similarly, treatment of athletes’ long finger stiffness may be optimized if minimal difficulties are anticipated. Intermittent regimes of active and passive mobilization together with the properly prescribed corrective splinting programs should be started as soon as problems arise or in postoperative period. Conservative treatment is the gold standard, and it may be all that is necessary for the quickest possible return to sports activities, which is the priority for an athlete.
8.1.1.5 Conclusion
A stiff hand is an unwanted but common consequence of a variety of hand injuries. The biological responses of the injured tissue in severe trauma are difficult to manage. Sometimes, minor trauma to the involved finger can also result in stiff joints if the patients are extremely withdrawn and cannot manage due to some psychological troubles. Therefore, managing the stiff finger joint is not only a matter of competition between the pace of prioritized treatment and the growth of scar tissues but a matter of psychological reassurance to the patients and the close relationship between the surgeon and patient as a whole.
The more the joints become stiff, the longer the tissues should spend at their end ranges in a fixator in order to improve the passive range of joint motion. At the same time, long hand therapy programs with intermittent regimes of active and passive mobilization—regardless of the technique—seem to be the vital measure.
Apart from these, accurate judgment, flexible attitude as well as prompt action are needed to tailor the treatment program for every individual patient. Good communication between surgeon and therapist as well as between surgeon and patients is important to ensure the best efficacy of treatment.
Key Points
Joint stiffness remains an unwanted but common phenomenon complicating severe hand injuries.
The most common posttraumatic joint contractures are the metacarpophalangeal joint extension contracture, proximal interphalangeal joint flexion contracture and extension contracture, and thumb web contracture—the positions that patients find to be more comfortable to rest their hands after injury.
The useful range of mobility in long fingers for ball athletes depends on the sport, position of the athlete, on the affected finger, and is related to the diameter of the ball.
Treatment used to improve the joint stiffness should be individualized, integrative, and problem focused.
Surgical treatment—as in open release or distraction histogenesis—can be considered only after failure of a long period of conservative treatment.
Suggested Readings
Natividade da Silva P, Barbosa R, Ferreira P et al (2005) Correction of long term joint contractures of the hand by distraction. A case report. Br J Plast Surg 58:1148–1151
This is a case report of a delayed (20 years) traumatic flexion deformity of PIP joint of index and middle fingers of left hand after complete division of both flexor tendons of both fingers. This clinical case shows the low cost, low morbidity, and the simplicity of application of joint distraction technique for correction of long fingers joint contractures, using a very simple lengthening device that is easy to assemble and adjust compared to other devices usually employed.
Hahn SB et al (2010) Correction of long standing proximal interphalangeal flexion contractures with cross finger flaps and vigorous postoperative exercises. Yonsei Med J 51(4):574–578
This is one of the only studies evaluating patients with flexion contractures associated with scar tissue around the joints. To restore function in these patients, surgical release of all contracted tissue seems to be inevitable, and the resultant skin defect should be covered with stable skin to prevent recurrence. This study evaluates cross-finger flaps after extensive surgical release of contracted tissue and vigorous postoperative extension exercises for long-standing severe flexion contractures with palmar scarring of the fingers.
Wong JMW (2002) Management of stiff hand: an occupational therapy perspective. Hand Surg 7(2):261–269
Treatment used to improve joint stiffness should be integrative and problem focused. Splintage, pressure therapy, and active mobilization are treatment modalities that occupational therapists use to improve hand function. This article helps surgeons to understand the process of tissue healing and different functions of splints for best results.
8.1.2 Stiffness of the Thumb
Abstract
Depending on the joint and sector of mobility involved, stiffness can affect ball catching, propulsion, and striking. The metacarpophalangeal joint (MCP) of the thumb requires stability to provide pollicidigital grips. Trapeziometacarpal (TMC) joint mobility is necessary for complex movements of the thumb column. Interphalangeal (IP) joint mobility compensates for overlying joint stiffness and increases ball grip. A wide first web opening is a key factor in ball control. Regardless of the stiffness level, treatment should first address the cause. Surgical treatment should only be considered for athletes if they have failed to respond to a sufficiently long period of conservative treatment. To adapt the treatment, a semiotic analysis must be performed to differentiate joint stiffness from stiffness due to periarticular soft tissues. Physical therapy must be provided after surgery to maintain the range of motion achieved through the intervention. The presence of symptomatic arthritis often suggests that the treatment effects may shorten the athlete’s career. For this reason, the best treatment strategy is prevention, including strict observance of immobilization positions and fixation rules.
8.1.2.1 Introduction
Stiffness of the thumb column or closure of the first web space can be handicapping when grabbing, throwing, or hitting a ball. The athlete’s resulting disability depends on the type of ball sports and the position held. Although finger mobility is essential, the stability of the thumb’s metacarpophalangeal (MCP) joint is critical for pollicidigital gripping. The trapeziometacarpal (TMC) joint must remain mobile and congruent to allow complex thumb movements. Retraction of the first web space should be prevented by observing immobilization principles.
8.1.2.2 Posttraumatic TMC Joint Stiffness
TMC joint stiffness can result in a more or less marked limitation of the abduction, adduction, and/or opposition of the thumb column. Flexion and adduction contractures may develop. The resulting functional deficit depends on the mobility sector involved, the demands, the presence of pain, and/or the decrease in grip strength [17].
Relevant Anatomy
The TMC joint is a double-saddle joint (Fig. 8.10) with two degrees of mobility. Its asymmetric nature contributes to its relative incongruence. It is stabilized by a dorsally fragile joint capsule, which is reinforced by a complex ligament structure (Fig. 8.11) that includes the posterior, anterior, and intermetacarpal ligaments [18].
Fig. 8.10
Anatomical specimen of a trapezium with a saddle-shaped surface for articulation with the base of the first metacarpal bone
Fig. 8.11
Ligaments of the TMC joint (According to Bettinger et al. [18]): (1) SAOL superficial anterior oblique ligament, (2) DRL dorsoradial ligament, (3) POL posterior oblique ligament, (4) DAOL deep anterior oblique ligament or “palmar beak ligament”, (5) IML intermetacarpal ligament, (6) DIML deep intermetacarpal ligament, (7) UCL ulnar collateral ligament, (8) DTT dorsotrapezotrapezoidian ligament, (9) VZZ ventrotrapezotrapezoidian ligament, (10) APL abductor pollicis longus. (G. Chick © 2012, all rights reserved)
Physiology
Mobility
The muscles of the first web space ensure the mobility of the TMC joint. They provide pure flexion/extension and abduction/adduction around two perpendicular axes. The geometric configuration of the joint allows for a third movement: automatic circumduction around the longitudinal axis. Complex movements of the hand, such as finger-thumb opposition, combine pure movements and circumduction of the thumb to varying degrees (Fig. 8.12). These movements are made possible by ligament tensioning caused by contractions of the intrinsic muscles inserted into the joint [19–21].
Fig. 8.12
Description of the mobility of the TMC joint. Flexion (F), extension (E), abduction (Abd), and adduction (Add) (According to Kapandji et al. [26]). (G. Chick © 2012, all rights reserved)
Effect of TMC Joint Stiffness on Ball Grip
Depending on the sport, the hand can propel (rugby, basketball, volleyball), hit (volleyball), or grip (handball, rugby, football) a ball. Complex technical movements such as spinning are a combination of basic movements. Stiffness in adduction and extension can limit thumb opposition and commissural opening, causing difficulties in catching and throwing balls. However, stiffness has little effect on hitting (Fig. 8.13). Stiffness in abduction and flexion impedes, distancing the thumb from the volar side of the hand and thus handicaps the hand hitting the ball (Fig. 8.14). TMC stiffness can also result in technical limitations, mainly in extreme positions, while a moderate limitation in the neutral position has little effect on hand function in ball sports.
Fig. 8.13
(a) TMC stiffness in adduction/extension altering the ability to catch the ball and limiting the adhesion of the ball in the hand, (b) gripping a ball in absence of TMC stiffness
Fig. 8.14
TMC stiffness in abduction/flexion right hand. (a) The thumb hinders the hand that strikes the ball. (b) The hand cannot be opened flat
Clinical Examination
Clinical examination should assess the pain, mobility, and strength and should measure the functional impact with questionnaires such as the Quick Dash [22].
Mobility
Assessing TMC joint mobility is difficult and poorly reproducible (Table 8.3) [23]. It is more often global than specific and includes the following [24]:
Flexion/extension (°) | Abduction/adduction (°) | Automatic rotation (°) | |
|---|---|---|---|
Normal articular range of motion | 41 | 51 | 21 |
The Kapandji test for circumduction [25]
Bourrel’s angle for opposition and rotation of the thumb column (Fig. 8.15)

Fig. 8.15
Bourell’s angle: It corresponds to the angle between the axis of the thumbnail and that of the fourth finger, when pulps of these fingers are in contact (measures the opposition and rotation of the thumb column) (a) normal (b) TMC stiffness: The ability to rotate is slightly reduced (clinical case of Fig. 8.14: TMC stiffness in the right hand)
The M1/M2 opening angle
Strength
Strength evaluation should include grip strength (using a Jamar dynamometer), lateral (lateral pinch) and distal key pinch strength measurements of the thumb index. The measurements should always be taken bilaterally.
Complementary Examinations
PA and lateral X-rays of the thumb column are the key examination. Kapandji views allow a TMC joint analysis [26], particularly measuring the height of the trapezial cavity and joint congruency. CT arthrogram may also be useful for accurate measurement of joint spaces.
Causes
TMC stiffness—with or without arthritis—can result from articular or extra-articular causes [27–29].
Articular Causes
These causes include cartilage and/or scarring lesions of the joint, which cause adhesions and destruction of the capsuloligamentous apparatus:
Articular fractures of the trapezium or fractures of the base of the first metacarpal
TMC joint sprains and dislocations
Articular wounds of the TMC joint
Septic arthritis
Intra-articular foreign bodies
Extra-articular Causes
Periarticular soft tissue lesions (tendons, muscles) and/or algodystrophy may cause TMC joint stiffness.
Iatrogenic Causes
TMC joint stiffness may be due to the insufficient or inappropriate treatment, such as transarticular pinning, the persistence of an intra-articular displacement, or the presence of material within the joint. It may also be due to delayed treatment, prolonged or incorrect immobilization, and failed rehabilitation.
Arthritic Origin
Arthritis is the most common cause of long-term TMC joint stiffness. It may be secondary to an articular malunion or chronic instability [30] and may be primary or rheumatic. Posttraumatic decompensation of the underlying arthritis raises responsibility issues.
Treatment
Conservative Treatment
A sufficiently long period of conservative treatment should always be the first-line therapy. Physical therapy and rehabilitation devices usually help recover a normal range of motion. Physical therapy includes gentle passive mobilization followed by active mobilization with isometric contract-relax exercises and electrotherapy. Static splints should be rigid during the night and flexible during the day, when they are worn for a few hours. The web opening should be maintained and the adduction maintained. The splints should be regularly adjusted in all three planes. Dynamic splints are not appropriate for TMC joint stiffness because they only provide correction in one spatial plane. Rehabilitation for several weeks or months is necessary before considering any surgical treatment [31, 32].
Surgical Treatment
Surgical treatment is rarely required for isolated TMC joint stiffness and should only be performed if medical treatment has failed. The type of surgery will depend on the state of the articular cartilage and the cause of the stiffness.
Arthroscopy
The recent contributions of arthroscopy have changed the strategies for joint surgery, although its efficacy and indications for small joints have yet to be determined (please see the corresponding chapter). For isolated TMC joint stiffness, arthroscopy primarily provides an accurate assessment of the progressive arthritic degeneration. Badia [33] proposed an arthroscopic classification of lesions that can be combined with clinical information to suggest surgical treatment that depends on the disease stage. Arthroscopy remains an effective tool for the early degenerative stages when X-ray images are normal despite the pain and functional impairment. Synovectomy combined with joint debridement and ligament tightening by thermal shrinkage seem to yield favorable results. Arthroscopic arthrolysis is a potential future surgical option.
Open Surgery
Indications for open TMC joint arthrolysis are rare, and a Gedda-Moberg volar approach is recommended in such cases. The radial artery is first identified and protected over the first web space. The procedure starts by sectioning the intermetacarpal ligament and assessing the web space opening achieved. The dorsoradial and posterior oblique ligaments are sectioned, and the passive pronation of the first metacarpal is evaluated. To our knowledge, the results obtained have not yet been published. Intra-articular osteotomy may be required to correct a joint malunion in displacement greater than 1 mm with absence of cartilage damage.
In most cases, the presence of arthritis precludes any joint preservation procedure. In these cases, the following options are possible (please see the chapter on thumb arthritis):
TMC arthrodesis is a paradoxical procedure that may be justified for manual laborers and young workers who have painful stiffness in the dominant hand and damaged joint surfaces. The optimal position for the arthrodesis is 40° of forward flexion and 20° of radial abduction. The main risk is nonunion [34].
TMC denervation may be indicated for cases involving pain. The procedure does not require postoperative immobilization, should not reduce general strength, and does not impede further surgery. A selective anesthesia test of the nerve branches directed towards the joint should be performed first [42, 43].
Recommended Treatment for Athletes
In cases where well-monitored medical treatment fails or where there is functional impairment, the following options may be considered.
In the absence of arthritis, arthrolysis (preferably arthroscopic) should enable a faster return to practicing sports. Osteotomies may be performed for malunions without arthritis.
If arthritis is present, the corresponding therapeutic strategy should be used (please see the corresponding chapter).
Prophylaxis
TMC joint stiffness treatments are primarily preventive and are based on the following rules:
Restoring an anatomical articular surface in cases of articular fractures (displacement <1 mm).
A volar approach (Gedda-Moberg) is preferred because it results in less stiffness.
No transarticular pinning (with respect to the TMC joint space).
Ligament repair should be protected by immobilization, preferably with pins in case of instability.
For immobilization, M1/M2 angle should be 30º in the three spatial planes.
The duration of immobilization should be less than 4 weeks for articular fractures and less than 3 weeks for dislocations.
Early rehabilitation should be initiated to avoid stiffness.
Posture splints should be used to avoid retraction of the first web space.
Key Points
The causes of TMC joint stiffness are mainly iatrogenic.
TMC joint stiffness treatment is primarily preventive.
If medical treatment fails for a professional athlete, the surgical indications must be cautious and adapted to the cause of the stiffness and its impact on the hand function pertinent to his sport.
8.1.2.3 Posttraumatic MCP Joint Stiffness
When the hand hits, guides, throws, or unexpectedly finds itself in the path of a ball, the MCP joint of the thumb may suffer a sprain, dislocation, or fracture. Approximately 19 % of MCP sprains are due to ball sports, of which a third are due to volleyball [29, 44, 45]. These lesions may be complicated by MCP joint stiffness.
Normal Mobility and Useful Range of Motion
The MCP joint of the thumb is a condylar joint that plays a critical role in thumb stability, while the TMC joint ensures mobility. The anatomical shape of the MCP provides three sectors of mobility.
The mobility in flexion/extension varies significantly from one individual to another. The normal range is between 10° and 90° of flexion. In lax subjects, hyperextension varies from 0° to 60° but can become pathological and disabling when it exceeds 60°. De la Caffinière and Mansat [46] have proposed evaluating stiffness based on residual MCP mobility sectors:
Extension stiffness from 0º to 30º
Extension stiffness in the useful range (from 30° to 70°)
Extension stiffness in flexion range (from 70° to 90°)
Although this useful range concept is valid for the MCP joints of the fingers, it does not take into account the variations observed in the MCP joint of the thumb:
The low lateral mobility in extension disappears in flexion.
The pronosupination is low.
This concept of useful range is critical and varies depending on the joints and fingers considered. Table 8.4 shows the results obtained by Hume et al. [21, 47], who assessed the amplitudes of normal MCP joint mobility:
Table 8.4
The functional/useful ranges of motion of the MCP and IP joints of the thumb
Range (°) | Average (°) | SD (°) | Median (°) | |
|---|---|---|---|---|
MCP joint | 10–32 | 21 | ± 5 | 22 |
IP joint | 2–43 | 18 | ± 5 | 19 |
Overall functional arc | 21–65 | 18 | ± 5 | 39 |
0–56° for 85 % of the population
0–27° for 15 % of the population
This variability in the useful flexion range influences the surgical indications. Most useful grips (such as the key pinch, distal pinch, and power grips) involve almost full extension of the MCP joint in a range between 0° and 20° of flexion. For large precision grips, the radial inclination increases the web space opening. The reference position of the MCP joint can be determined at 20° of flexion.
Effect of MCP Joint Stiffness on Ball Grip
We can distinguish between stiffness in extension and in flexion [48]:
Stiffness in extension results in reduced active and passive flexion range of motion (Fig. 8.17).

Fig. 8.17
MCP stiffness in extension of the right thumb: (a) volar view, (b) dorsal view
Stiffness in flexion results in reduced active and passive extension range of motion (Fig. 8.18).
Fig. 8.18
MCP stiffness in flexion: (a) abduction, (b) adduction
The consequences of extension stiffness are negligible if the MCP joint stiffness is isolated and is in the functional position (i.e., in nearly complete extension between 0° and 20°, which is almost the reference position). The web space opening is preserved, and the mobility of the thumb column is preserved by the TMC joint. Grabbing and hitting a ball and technical moves in handball, volleyball, and rugby are not affected. Dribbling in basketball remains possible (Fig. 8.19). Stiffness in flexion is less common and has a major impact because the thumb is in the palm and it impedes lateral pinches (key pinch) and power grips of balls of large and small diameters. It is difficult to grab a ball due to the reduced web opening caused by the extension deficit. The ball cannot fit into the web space, and grip strength is reduced (Fig. 8.18). The “adherence” of the hand to the surface of the ball is impaired. Hitting is hampered on the radial side of the hand by the thumb column because it does not remain on the volar side.


Fig. 8.19
MCP stiffness in extension. The grip of the ball in handball remains possible
Differential Diagnosis Between Joint and Tendon Stiffness
The causes of extension stiffness are diverse and may be isolated or combined [29, 48]:
Dorsal cutaneous scarring lesions
Adherence of the extensor apparatus to the periosteum or the joint capsule
Retraction of the dorsal fibers of the collateral ligaments
Arthritis and articular malunions
Symphysis of the volar plate cul-de-sac
Stiffness in flexion may have the following causes:
Retraction of the skin on the volar side
Retraction and adherence of the flexor tendon system in the finger channel
Retraction of the volar plate and filling of its cul-de-sac
Retraction of accessory collateral ligaments
Articular osteochondral lesions
The following can be used to differentiate between articular and extra-articular stiffness [49]:
A history of extensor or flexor tendon lesions
Poor extension of the interphalangeal (IP) joint due to retraction of the flexor pollicis longus (FPL) and/or deficits in the specific testing of the FPL
A bow-stringing effect on the FPL due to lesions on the pulleys
Lack of IP flexion due to adherence of the extensor tendons
MCP and IP joints X-rays
Overall, stiffness that is secondary to wounds is often mixed and requires tenoarthrolysis. Stiffness that is secondary to sprains and fractures is usually articular.
Conservative Treatment
Not all cases of joint stiffness require surgical treatment. Surgery is only indicated after well-conducted and consistent rehabilitation efforts fail [50, 51]. Stiffness in the functional position should be distinguished from stiffness that affects technical moves. Stiffness in extension responds well to conservative treatment, such as dorsal massages to improve vitality and to restore a gliding motion between the extensor mechanism and the joint capsule, the extensor, and the subcutaneous fat. Passive and active global and specific rehabilitation helps activate the extrinsic flexors and extensors. Dynamic flexion splints of the thumb should be used as soon as MCP flexion is possible. They are worn during the day and replaced by postural splints at night. Establishing the rehabilitation gains is a long-term process that can take several months. Stiffness in flexion is less responsive to conservative treatment, especially if it involves the flexor tendon. A global extension splint, possibly dynamic, should be worn for 5–7 h/day or at night as soon as possible. It is contraindicated in cases of ulnar ligament laxity. Global action braces may be used if the stiffness is painful, while more selective splints can be used for painless stiffness. Conservative treatment should last at least 12 weeks before considering surgery.
Surgical Treatment
This section focuses on arthrolysis and tenoarthrolysis, which are open surgical procedures. Percutaneous arthrolysis, which may be used for other joints of the hand, seems to be of limited use because it does not allow access to intra-articular adhesions and risks damaging noble structures. Distraction methods are of little interest, and procedures under anesthesia are contraindicated [23]. The indications for small joint arthroscopy [52] and arthroplasty [53] of the hand remain poorly established (please see the corresponding chapter), which is partly due to the limited literature available on the subject. Arthroscopy is rarely used on the MCP joint of the thumb, except for Stener lesions resulting from severe sprains. Arthroscopy can be used to treat purely articular joint stiffness, although articular joint stiffness is rare in cases of flexion stiffness of the MCP joint [33, 54, 55].
The indications for surgery and the corresponding prognosis depend on several factors, such as the athlete’s level, the type of ball sports they play, the mobility sector involved, the cause of the trauma, vascularization, sensitivity, skin viability, the state of the tendons and the joint, and the time elapsed since the beginning of the stiffness.
Stiffness in Extension
Due to good functional tolerance, the indications for surgery are rare in ball sports. The surgical approach is either dorsomedial and sinuous or dorsoradial and sinuous. The skin flap is retracted while protecting the dorsal venous network and dorsal sensory collaterals. The extensor pollicis longus (EPL) and brevis (EPB) tendons are tenolysed upstream of the MCP joint. Using a blunt spatula, the lateral band is lifted from the plane of the joint ligaments. The extensor is then lifted with an atraumatic retractor. A dorsal capsulotomy is performed, and the joint is released up to the metacarpal volar cul-de-sac (if possible) using an atraumatic blunt elevator. At this point, passive flexion is attempted. If flexion is impossible, the sagittal bands are partially sectioned along and one millimeter from the extensor mechanism. This procedure exposes the dorsal metacarpal insertion of the collateral ligaments, from which the more dorsal metacarpal fibers may be sectioned if necessary. The surgery should target a useful range rather than a flexion of 90°. Arthrolysis is a progressive procedure that is performed on request, following a specific sequence determined during the preoperative evaluation. Satisfactory joint congruency must be ensured in flexion, and a dorsal gap should be avoided [47].
Stiffness in Flexion
In certain cases, the hand’s reduced capacity in ball sports is significant, and conservative treatment is less effective. The surgical strategy often depends on the type of damaged tissue. Stiffness due to an isolated lesion of the capsular ligaments may respond favorably to ergotherapy. Skin lesions, which are usually of extra-articular origin, may respond favorably to plastic surgery or flaps. When the FPL or several lesions are involved, the strategy should include tactical coverage to protect the tendon. The anterior Bruner’s incision should be large. The collateral neurovascular bundles should be identified and protected, and the oblique pulley should be conserved. The A1 pulley can be excised, however. The flexor tendon is gently freed from its adhesions and from the volar plate with a blunt spatula and a no. 15 blade. The tendon can then be moved laterally. In rare cases, the volar plate may need to be released from the metacarpal neck. The main medial and lateral ligaments should be conserved. A blunt elevator can be used to lift the intra-articular adhesions up to the dorsal part of the joint. The accessory collateral ligaments that are retracted in flexion can be sectioned. The joint should not be destabilized [48]. If the articular cartilage is damaged, arthrolysis and tenoarthrolysis are no longer indicated and arthrodesis in a functional position of approximately 20° of flexion should be considered [56, 57]. Prosthetic MCP arthroplasty for ball sports is questionable [55].
Postoperative Management
The released elements have a natural tendency to retract, setting the joint in the preoperative position. Postoperative treatment should start on the first day after the surgery and should aim at maintaining the range obtained through the surgery [23]. Swelling and pain should be prevented in the early postoperative hours. In some difficult cases and depending on the patient’s pain threshold, continuous analgesia may be administered with a catheter. Rehabilitation is analytic and global and as painless as possible. From day one, a postural brace stabilizing the joint in the final position should be worn at all times, except during rehabilitation sessions. Global or dynamic flexion or extension splints should be worn from postoperative day 8, depending on the area involved. The frequency of use depends on the patient’s tolerance. Assuming that the skin has healed, rehabilitation should be performed daily from the 15th day, and splints should be worn day and night and combined with physical therapy against scarring fibrosis.
Results
One of the prognostic factors is the time elapsed since the beginning of the stiffness, and it is responsible for cortical exclusion, muscle atrophy, and cartilage lesions. The goal is pain relief and stability with a useful range around the reference position of 20°. The adhesion of the hand to the ball depends on the pressure exerted by the opposition of the thumb and fingers, and the web opening (TMC) has a major effect on MCP mobility. To date, no series have been published on the results of treating MCP stiffness in ball sports.
Return to Sports Practice
The postoperative rehabilitation program is long, and the patient should be informed that the benefits from the intervention stabilize around the fourth postoperative week and are established after 3 months.
Key Points
MCP joint mobility is highly variable, and the useful sector is around 20°.
Stiffness in extension is well tolerated and responds more favorably to conservative treatment.
Stiffness in flexion penalizes technical movements in ball sports and is often treated surgically.
8.1.2.4 Stiffness of the Interphalangeal (IP) Joint of the Thumb
The IP joint is a trochlear joint with one axis of movement allowing flexion/extension. The two phalanges are joined by the volar plate, which is covered by the FPL, and the main and accessory collateral ligaments [46, 58].
IP joint stiffness may be articular or extra-articular [23].
The articular causes include traumatic, degenerative, or inflammatory disorders that alter the articular surfaces.
The extra-articular causes include fibrous retraction of the capsuloligamentous structures, skin lesions, and FPL or EPL lesion sequelae [59].
Normal Mobility, Useful Range
The normal articular ranges of motion are 30–40° in extension and 70–90° in flexion. Hyperextension has no specific function, while flexion adjusts the precision of the grip depending on the gesture being performed. The FPL stabilizes the IP joint in the 0° position during the key pinch. Fine grips are terminal pinch in IP extension or distal nail pinch when the IP joint is stabilized at approximately 45° of flexion.
Hume et al. [21] showed that the normal range of motion of the IP joint varies from 5° to 73° (the functional amplitudes are shown in Table 8.4). During gripping, the average degree of flexion of the IP joint is from 28° to 36°. Due to the shape and size of the ball, such a degree of flexion is not required for seizing a ball.
Hand movements in ball sports do not require an IP joint flexion beyond 20°. The IP joint should be at 0° extension to absorb energy when catching a ball (e.g., during volleyball, basketball, and handball). The IP joint should be stabilized in slight flexion (from 10° to 20°) when holding a ball. This angle supports the P2 pulp and opposes the other fingers, which in turn provides adhesion to hold the ball.
Impact of IP Joint Stiffness on Seizing a Ball
Stiffness in the useful range of motion 10°/0°/20° has little effect on technical movements. Beyond this range, stiffness in flexion may impair receiving and holding a ball and disrupt the technical level of performance. The hand must be able to conform to the shape of the ball. In stiffness in flexion, only the distal portion of the pulp will be used for seizing a ball, which reduces the possibilities for adhesions. The IP joint contracture also reduces the first web space opening and limits the fitting of the ball into the hand. In this position, the FPL loses some of its stabilizing properties (Fig. 8.20).


Fig. 8.20
IP joint stiffness in flexion, left thumb: (a) side view, (b) web view
Conservative Treatment
In principle, conservative treatment is indicated before surgery and when the articular cartilage is healthy, that is, in cases of extra-articular IP joint stiffness. The prognosis depends on the type of IP joint stiffness, the condition of the skin, and the possible involvement of the FPL. The treatment may last for 3 months.
Stiffness in Extension
Specific and global techniques should be used: place-hold exercises, postural, and any other means needed to prevent fibrosis. A dynamic short flexion splint of the thumb may be more specific for the IP joint because it stabilizes the MCP and P1. The flexion bandage is attached radially and should be used for 6 h a day. Postural splints are of little use here [50].
Stiffness in Flexion
Conservative treatment is more difficult because the FPL is usually involved. The treatment employs splints and the standard rehabilitation described above. The extension splint, which is attached in the direction of the opening of the hand, is adapted for the IP joint. The thermoformed short thumb splint stabilizes the MCP and includes P1. The extension band pulls on P2. The duration of use is approximately 8 h daily, and this better-tolerated splint should be worn at night as soon as possible [51].
Surgical Treatment
Surgery may be proposed after conservative treatment fails. The indication is based on the hand gestures in sports, associated pain, and the cause of the stiffness.
Stiffness in Extension
If the cartilage is healthy or slightly damaged, a dorsal tenoarthrolysis should be performed, together with skin cover if the lesions are complex. Homodigital flaps (Hueston type) are usually sufficient. Beasley’s approach in H can expose the EPL tendon. Any skin lesions are excised with the incision while incorporating the reconstruction flap. The recovery of skin flexibility is crucial. The tendon is released at its medial and lateral edges with a no. 15 blade. The tendon hook is used to lift the EPL tendon and expose the joint. The cartilage is then evaluated. A blunt spatula can be used to release any articular adhesions. If a P2 dorsal osteophyte is present, it should be excised with a 3-mm osteotome without weakening the EPL insertion. The nail matrix should be preserved to avoid iatrogenic onychodystrophy. In rare cases, the dorsal proximal insertion of the main ligaments on P1 should be sectioned [47].
If the articular cartilage is damaged and the joint is painful, it is preferable to perform an arthrodesis. Positioning the arthrodesis close to the extension (between 0° and 10°) seems to be the most appropriate in the context of ball sports. It should not exceed 20° of flexion.
Stiffness in Flexion
This condition is less well tolerated, is resistant to conservative treatment, and usually requires surgical intervention. Lesions of the FPL are often involved, and the indications for surgery depend on the state of the cartilage.
In case of arthritis, arthrodesis [60] is the treatment of choice (please see the corresponding chapter).
When the joint is healthy, the stiffness is secondary to lesions of the FPL and/or a volar skin retraction (following a traumatic wound). The anterior Bruner incision should be designed to incorporate the skin reconstruction procedure chosen. Different homo- and hetero-digital fasciocutaneous flaps can be used, and collateral bundles are controlled and protected. The FPL procedure depends on the lesions. A tenolysis should be nontraumatic and should respect the oblique pulley. Lengthening the FPL may be necessary and should be performed at the musculotendinous junction (of Le Viet or Rouhier), which allows an advancement of 15 mm [61, 62]. In rare cases, the volar plate can be released at the P1 neck without destabilizing the joint. Severe lesions of the flexor system may be an indication for an arthrodesis rather than a tendon graft, which is more complex and gives random results. Correcting the IP contracture is crucial for technical movements in ball sports.
Postoperative Management
The postoperative management is variable depending on the type of stiffness and the size of the lesions. It may include dynamic flexion splints worn several hours a day combined with rehabilitation therapy (please see the corresponding chapter). The postoperative treatment should be maintained for 3–6 months.
Results and Return to Sports
There are no published series on treating IP joint stiffness in ball sports. In extension stiffness, the return to sports should be possible within 10–12 weeks of arthrodesis surgery. In case of arthrolysis or tenoarthrolysis, the delay will be longer and will depend on the associated movements conditioned by the initial lesions (flap) and the pain resolution. In flexion stiffness, a return to sports is possible within 3–6 months, depending on whether the treated lesions were simple or complex (involving the joint, FPL tendon, and skin). The FPL action is important for ball sports, and arthrodesis is preferable in cases with a weak or even inactive FPL.
Key Points
Flexion stiffness in the IP joint of the thumb impairs athletic performance in ball sports, while an extension position between 0° and 20° will be of little consequence.
The prognosis depends on the type of lesion and on the state of the flexor tendon.
Arthrodesis is the procedure of choice if the joint is altered.
8.1.2.5 Contracture of the First Web Space
The Anatomy of the First Web Space
The Skin Envelope
The envelope is a plastic functional unit. The integumentary coating is formed by two isosceles triangles, the base of which defines the free edge of the web space. The dorsal skin on the social side is thin, flexible, and mobile. The volar skin is thicker and docked to the volar fascia by vertical septa [63].
Content
The Skeleton
The bony skeleton of the first web space is composed of a mobile segment (the TMC joint and first metacarpal) and a fixed segment (the second metacarpal).
The Muscles
The muscles that form the first web space are spread in a fan-like pattern between the first and second metacarpals [23], with one or several heads of insertion:
The first dorsal interosseous muscle
The first volar interosseous muscle (variable)
The adductor muscle of the thumb
The short flexor (deep beam)
The Aponeuroses
The aponeuroses of the first web space define three muscular compartments for the following muscles:
The dorsal interosseous muscle
The volar interosseous muscle (variable)
The adductor and short flexor muscles of the thumb
Neurovascular Structures
The neurovascular structures are divided into two networks (volar and dorsal) that provide vascularization (anastomoses) and innervation to the first web space.
Physiology
Several conditions are necessary for opposition to be normal [64]:
A high-quality dorsal and volar skin covering
A mobile and stable TMC joint
Preserved integrity of the driving muscles of the thumb column
Stable MCP joints of both the thumb and index finger
A normal thumb column length
Etiology
Sandzen [65] has proposed a simple classification system that is based on the structures involved (skin, muscles, bones, and joints) and the severity (mild, moderate, and severe). These three forms may be isolated or combined.
Isolated Cutaneous Forms
The isolated skin forms are often of thermal origin and have a retractable skin scar located at the free edge or on one of the dorsal or volar cutaneous functional units of the first web space. Any scar that runs through one side of the web space will shrink, especially if it is parallel to the free edge.
Muscular Forms
The muscular forms are traumatic, ischemic, or paralytic in the context of a compartment syndrome. Usually, there is retraction of the thumb adductor, which may also be caused by incorrect immobilization.
Osteoarticular Forms
The osteoarticular forms may have a direct cause (a fracture of the first metacarpal or its base or an articular fracture of the trapezium) or an indirect cause (ankylosis of the TMC joint by prolonged immobilization and/or improper positioning) [45]. Primary or posttraumatic TMC joint arthritis may cause stiffness when closing the first web space. TMC joint involvement is a prognostic factor because while releasing the muscles and skin during the surgical procedure may provide a satisfactory opening for the first web space, it is not certain that this procedure will restore automatic or active pronation of the thumb column, which is dependent on the TMC joint [66].
Acute Compartment Syndrome of the First Web Space
Acute compartment syndrome of the first web space is rare and may result from a severe crushing trauma. This syndrome should be suspected when there is tension of the first web space compartment and irreducible and painful adduction of the first column.
Clinical Examination
Mobility and Stability
The range of motion of each joint (normal values have been described in other chapters) should be measured with a goniometer and compared to the opposite side. The joint stability and strength should be tested. The following factors should be emphasized when there is closure of the first web space:
Compensatory MCP hyperextension may contribute to the Z deformation of the thumb. When the retraction of the first web space is old, this adaptation phenomenon allows holding larger cylindrical objects. The medial collateral ligament of the MCP can be distended and is associated with hyperextension of the MCP [67].
The capacity for progressively larger cylindrical grips.
The muscles of the first web space (C1) should be palpated to assess their vitality (Fig. 8.21).

Fig. 8.21
First web space retraction and muscle atrophy
The sensitivity of the first web space should be evaluated using the Weber test and Semmes and Weinstein monofilaments.
The Impact of First Web Space Stiffness and Useful Range on Ball Grip
The hand should be able to hold, hit, or propel a ball using specific technical movements. The useful range is based on the size of the ball and the gesture performed.
When catching a ball, the first web space should absorb the kinetic energy through complex retropositioning, opening, and opposition movements.
The correct handling of a caught ball is necessary to spin the ball during its propulsion. The hand completes the gesture and uses the energy developed by the upper limb.
At present, we cannot determine the mobility angles of the first web space required for perfect performance by ball athletes, and skills have not yet been modeled [70]. A study [71] has evaluated the adaptation potential by simulating a 30° and 60° closure of the web space. Due to a compensation phenomenon, the test results were poorer when grasping small objects than when grasping large and heavy ones. The decreased opposition and opening limits the pressure exerted by other fingers on the thumb when holding the ball. The “adhesion” capacity to hold the ball, which is needed when playing volleyball, is altered (Fig. 8.22). When the web space is retracted, adaptability is provided essentially by the medial collateral ligament of the MCP joint. The progressive stretching of this ligament maintains a commissural opening, but its amplitude and force are limited by deficiencies of the thumb adductor. It is also limited in depth because the apex of the triangular web space, which constitutes a true point of rotation (initially trapezoid metacarpal), shifts to the MCP of the thumb. Regardless of the etiology, retraction of the first web space will have major consequences on the functioning of ball athletes. Indeed, the diameters of different balls are such that an optimal range is essential for high-level athletes.
Fig. 8.22
Grabbing a volleyball without (a) and with (b) closure of the first web space
Investigations
Conventional radiography can be used to assess and compare the joints and bone of the first web space (C1) (Fig. 8.23). Magnetic resonance imaging (MRI) can assess the condition of first web muscles in old retractions. The functional quality of these muscles is a major prognostic factor. Other tests may be of interest for the etiologic diagnosis.


Fig. 8.23
Radiological views. (a) PA view: peritrapezial TMC and STT ankylosis with closure of the first web space, (b) lateral view: allows the analysis of the bony elements of the first web space
Treatment
Nonoperative Management
This treatment is almost always indicated before surgery being integrated into an overall strategy in preoperative preparation. The treatment constitutes the preoperative “link” between the physiotherapist and the patient. The results are unpredictable and depend on the etiology, stage of the stiffness, and initial lesions [72, 73].
There are few studies and no protocol has cu`rrently been established. The studies that do exist suggest the following:
A global and specific program of joint rehabilitation
“Place-hold” exercises
Working the tissues to relax the muscles and aponeuroses and remove adhesions
Web static postural splints that are regularly adapted to the increasing amplitude of the web opening. The duration and frequency should be adjusted according to tolerance, and resting splints can be used.
Surgical Management
Surgery should be performed after conservative treatment has failed. The surgery includes three steps: releasing the envelope, repairing it, if necessary, and reconstructing the various anatomical elements necessary for dynamic thumb functioning. The reconstruction flaps used in emergencies are indicated in the secondary surgery. The number and difficulty of procedures required depend on the severity of the initial lesions [74, 75].
The Release
The first step gives access to the muscles of the first web space and the TMC joint, if necessary. The procedure starts with the skin, and the operative strategy should include reconstructing the envelope.
A skin plasty may be sufficient for mild forms with retractable skin straps. Indications for plastic surgery depends on the elongation and/or deepening of the web space; Z-skin plasty (Fig. 8.24a); and double Z, “four flaps,” or trident (Fig. 8.24b) be used [76–78].
Fig. 8.24
Drawing of skin incisions for Z-plasty: Skin flaps must respect angles of 60º (a), trident with effect of elongation of the free edge and web opening (b)
A skin graft is indicated for moderate forms with lesions of the free edge and of the dorsal and/or volar sides (symmetrical or asymmetrical lesions) of the web. The incision should be vertical (Fig. 8.25) and perpendicular to the free edge of the web space.

Fig. 8.25
Vertical web incision before full skin graft
Some cutaneous loss is inevitable during the release, and the quality of the muscle base should be good. A full-thickness skin graft can be used to cover, as split-thickness grafts are prone to shrinkage. This graft can be performed in the same setting or after several days; daily dressings should be applied in the interval. Skin may be taken from the inner arm, which is a more esthetic donor site providing good match to dorsal skin of the hand. A temporary intermetacarpal pin is placed in the open web position to protect the graft and facilitate the dressings for 15 days [79].
In severe cases, the incision should cut the first web space in the middle, perpendicular to its free edge (Fig. 8.25). The musculoaponeurotic release begins with detaching the superficial head of the first dorsal interosseous of the first metacarpal and the deep volar fascia underneath. If necessary, the adductor is freed from its insertions on the second and third metacarpal by a volar incision in the M3 axis. The beam angle of the adductor is preserved. In very advanced forms, the head of the deep flexor must sometimes be freed or the first lumbrical must be excised. When all the tissues are fibrous (due to scarring), the C1 incision must be extended to the top while preserving the radial artery.
If these steps are insufficient in severe retraction, an arthrolysis of the TMC joint or even a total or partial trapeziectomy should be performed [80]. An M1/M2 intermetacarpal pinning in the open web position may be indicated at the end of the release before the surgical reconstruction.
Reconstruction of the First Web Space with Flaps
Local Flaps
Various types of fasciocutaneous flaps are available. Their advantage is providing vascularized, sensitive tissue with low morbidity.
Regional Pedicled Flaps
After the web space is maximally opened and the intermetacarpal pin is placed, the defect may require distant flaps.
Posterior interosseous flaps [83, 84] from the proximal third of the forearm do not sacrifice any major vascular axis (Fig. 8.26).

Fig. 8.26
Posterior interosseous flap for reconstruction of a complex lesion of the first web space
Antebrachial (Chinese) flaps [85] should be a second choice because of donor site morbidity due to sacrifice of the radial artery.
The inguinal McGregor flap [23] is a reliable flap that can be used in severe hand trauma. Given the advantages of the posterior interosseous flap, however, the inguinal flap is rarely used for reconstructing the first web space.
Free Flaps
Main fasciocutaneous free flaps may be used, but a lateral arm flap from the same limb is the flap of choice [86, 87]. Smooth, thin hairless skin similar to that of the first web space is necessary. The arterial anastomosis is performed end to side with the radial artery in the snuffbox or the first interosseous space. Other donor sites are also possible: the anterolateral thigh flap [88] pedicled on the circumflex artery and a flap from the back of the foot, with good matching but significant donor site morbidity [89]. Free flaps provide early rehabilitation but can cause donor and recipient site problems in athletes.
Postoperative Care
The postoperative dressing should keep the web space open and keep the thumb column in a functional position (Fig. 8.27). In the absence of intermetacarpal pinning, a web splint can be used and replaced by a removable thermoformed splint on the fourth postoperative day. Rehabilitation and edema prevention should start early. Metacarpal pins are widely used, especially if there is complex tissue damage and flap reconstruction. Antibiotic prophylaxis is not systematic and depends on the etiology of the stiffness and medical history. Once the skin is healed, measures to prevent tissue fibrosis and adhesions are started. Rehabilitation and physical therapy are performed for 3 months, and a static splint is worn for at least 3 months postoperative to establish the results.


Fig. 8.27
Postoperative immobilization of the web space
Complications
Nonspecific complications, such as hematoma, infection, and CRPS, are rare.
Specific complications include recurrence of the retraction, especially if the muscles of the first web space are not functional. Correct surgical indications, proper treatment, and postoperative management should reduce this risk. Specific complications of the reconstruction technique include skin and graft necrosis or flap loss. The complications are mainly associated with severe forms of web retraction. Smoking cessation during the preoperative period is imperative [92].
Outcome and Return to Sports
To our knowledge, no series have been published assessing the return to high-level ball sports after treatment of first web space retraction. To our knowledge, no study has determined which components of the TMC motion are most important for obtaining good results after a surgical release. Although the release should restore the radial and volar abduction angles, it has no significant impact on the DASH score. For mild forms, the results are satisfactory, and a return to ball sports should be possible after 3–5 weeks, depending on the patient’s healing. For moderate forms, the time extends to 2–3 months due to the longer healing times of deep tissues. For severe forms, a return to ball sports is uncertain and should be discussed on an individual basis, depending on the lesions. The quality of the motor muscles of the first web space and the TMC joint are decisive prognostic factors.
Preferred Treatment Methods for Athletes
The treatment should initially be conservative, with successive removable postural splints to loosen the web space, and should be followed by specific and global physiotherapy. Surgical treatment for high-level athletes should be carefully considered. Unlike other flaps with significant donor site morbidity, skin grafts and local fasciocutaneous flaps allow early return to sports, which may detain the recovery of athletes in high-level sports. The best option for moderate forms is a full-thickness skin graft. For severe cases, a posterior interosseous flap is the best option or a lateral arm free flap if this is not possible. The intermetacarpal pin must spare the TMC joint.
Prevention
Preventing first web space stiffness is achieved by respecting the principles of immobilization in a proper position, that is, in open opposition for orthopedic and surgical treatments. All lesions should be repaired, fractures should be stabilized, and the web space held open by a web splint or an intermetacarpal pin, depending on the severity of the lesions. Rehabilitation should be early and tailored to the patient.
Key Points
The recovery of the web space opening is essential for the correct execution of technical movements specific to high-level ball athletes.
Treating first web space trauma, whether isolated or associated with complex lesions of the first column, requires repairing all lesions and the preventing retraction of the web space.
Regardless of the nature of the trauma, immobilization rules should be strict. Prevention remains critical at all levels of patient management.
The prognosis depends on the quality of the TMC joint and the quality of the muscles of the first web space.
Suggested Readings
Glasgow C, Tooth LR, Fleming J (2010) Mobilizing the stiff hand: combined theory and evidence to improve clinical outcomes. J Hand Ther 23:392–400
The purpose of this review is to provide a clinically reasonable guide to intervention choices, by combining a sound understanding of theory with available research evidence. The importance of mobilizing splinting and exercise as treatment modalities in the management of joint contracture is demonstrated.
Goubier JN, Devun L, Mitton D, Lavaste F, Papadogeorgou E (2009) Normal range of motion of trapeziometacarpal joint. Chir Main 28:297–300
One hundred and one healthy subjects were analysed for the development of a database of normal active range-of-motion parameters of the trapeziometacarpal joint, with an in vivo protocol. The mean range-of-motion of the trapeziometacarpal joint was 41 degrees for flexion-extension, 51 degrees for abduction-adduction and 21 degrees for axial rotation.
Hume MC, Gellman H, McKellop H, Brumfield RH Jr (1990) Functional range of motion of the joints of the hand. J Hand Surg 15:240–243
There is little data reporting the functional ranges of motion required to perform activities of daily living. The authors measured both active and functional ranges of motion of the metacarpalphalangeal and interphalangeal joints during 11 activities of daily living. In the thumb, functional flexion postures averaged 21 degrees at the metacarpalphalangeal joint and 18 degrees at the interphalangeal joint using only 32 % of the available flexion.
Kalliainen LK, Schubert W (2005) The management of web space contractures. Clin Plast Surg 32:503–514
The authors present a review of the anatomy of the web and options for reconstruction of web space contractures.
8.1.3 Rehabilitation Protocol After Operative Release of Contracture
Abstract
For the ball sports athlete, joint contractures of the digits may have a detrimental effect on performance and lead to pain and injury during play. If nonoperative techniques fail to achieve the desired range of motion, surgical release may be required. This chapter discusses the general postoperative rehabilitation strategies for ball sports athletes and makes suggestions for specific rehabilitation programs following metacarpophalangeal joint, proximal and distal interphalangeal joint, and first web-space contracture releases. Areas for further research are also highlighted.
8.1.3.1 Introduction
Contractures are characterized by a reduction in active and passive joint range of motion (ROM) and can occur at an isolated joint or across multiple joints and digits. For cases where active but not passive motion is restricted, other causes such as tendon adherence or rupture must be considered (see Sects. 7.3 and 8.2). Many factors can lead to contracture formation including immobilization, previous surgery, and trauma; the common feature being the resultant soft tissue shortening. For ball sports athletes, this reduced ROM can impede ball handling, cause pain or discomfort during play, and interfere with general daily functioning.
This chapter will discuss the functional ROM required for ball sports athletes and the rehabilitation process following contracture release in the digits. Specific splinting, scar management, ROM, and strengthening procedures will be proposed as a means to facilitate the timely return of the athlete to his or her sport.
8.1.3.2 Functional Range of Motion
The impact of a joint contracture on an athlete’s performance will depend on both the location of the contracture and the particular ball-handling skills required. Sufficient finger extension and thumb abduction are needed to open the hand prior to catching a ball, and contractures limiting these movements will impede function and may lead to repeated reinjury of the affected digit. Finger flexion and thumb opposition are required for gripping and holding a ball, and restrictions to movement in these planes will reduce grip strength and control.
Hume et al. [93] measured the functional position of the fingers and thumb for 11 gripping activities; the mean range and flexion required are outlined in Table 8.5. It is important to note that full extension and flexion ranges are not necessary for these tasks. Specific data on the functional ROM used for different ball sports is not available; each patient’s requirements will need to be discussed, and, if necessary, ROM of the unaffected hand can be measured in grip positions used for the patient’s particular sport. This information serves as a guide to whether surgery is indicated in order to improve functional performance and provides a basis for rehabilitation goals.
Table 8.5
Function ranges of motion and mean flexion required for 11 gripping activities
Digit | Location | ROM required for gripping (°) | Mean flexion (°) |
|---|---|---|---|
Thumb | MCPJ | 10–31 | 21 |
IPJ | 2–43 | 18 | |
Finger | MCPJ | 33–73 | 61 |
PIPJ | 36–86 | 60 | |
DIPJ | 20–61 | 39 |
8.1.3.3 Surgical Considerations
It is generally recommended that nonsurgical treatment, such as splinting or serial casting, is attempted prior to surgical intervention [94]. If conservative measures fail to achieve sufficient lengthening of shortened tissue and restoration of active ROM suitable for the athlete’s function, then surgical release may be required. In the case of severe contractures, especially where there is reduced joint surface integrity, other surgical options, such as arthrodesis, may be more appropriate.
The surgical procedure usually takes the form of a sequential release starting with the most superficial structures and progressing to the level of the joint capsule. ROM is assessed after the release of each structure, and surgery progresses until functional ROM is achieved [95]. Tenolysis may be required in conjunction with a joint release if tendon adhesions are apparent (as discussed in Sect. 8.2.3). Advanced soft tissue cover options need to be considered for severe contractures, and if a Z-plasty provides insufficient cover, skin grafts may be required. Rehabilitation will be slower with grafted areas as they may need to be protected for 7–10 days before mobilization is commenced, and splinting may need to be modified to avoid any shearing forces on the graft.
As the structures involved and the degree of surgical release required vary for each contracture, it is important that the therapist has complete understanding of the surgery performed in order to establish safe and effective postoperative rehabilitation. The therapist must be aware of any limitations to full passive ROM and potential concerns related to joint stability. In all cases, it is unlikely for the intraoperative ROM to be fully maintained postoperatively, although further research is required to establish the proportion of intraoperative motion that should be expected at 3 months and longer after surgery.
8.1.3.4 General Rehabilitation After Contracture Release
The aims of joint contracture release are to increase joint ROM and to move the available movement into a more functional range. It is therefore essential that joint mobilization is commenced as early as possible after surgery in parallel with appropriate wound management. The overlapping phases of tissue healing are summarized in Fig. 8.28, and the therapy goals and interventions will be guided by these timescales in the presence of a healthy wound environment. Healing may be significantly slowed if complications arise, for example, infection, delayed wound closure, and tissue injury, and the therapist should carefully evaluate the wound or scar in order to determine the most appropriate care plan.
Fig. 8.28
Wound healing timescales and therapy goals
Edema Management
Edema management is important during the inflammatory and proliferative phases of the first 10–14 days. Excessive edema will increase the risk of wound separation, physically restrict joint ROM, and lead to increased adhesion formation as collagen is laid down. Elevation and the use of light compressive dressings are recommended to minimize postoperative edema [95].
Scar Management
Once the surgical wound is healed, during the proliferation and remodeling phases, scar management is essential to prevent scar contracture and adhesions restricting the available joint ROM. Scar massage is advised during the proliferation phase to influence collagen alignment and to move the scar tissue across the underlying soft tissues to minimize subcutaneous adherence [96]. Massage with active ROM helps prevent tethering of the tendon(s) to scar tissue, and massage with passive stretching of the scar encourages collagen realignment in a lengthened position. Scar massage is also important for desensitization, especially for scars to the palmar surface, due to the need for contact between the scar and the ball during play. Tolerance to touch can be increased using massage, exposing the scar to different textures and vibrations [97]. For thick, bulky scar tissue, silicone products are indicated to improve scar quality and minimize hypertrophic scarring [98]. These are usually worn overnight to allow unrestricted movement during the day for up to 8 weeks after wound closure. Ultrasound treatment may also be beneficial to increase the elasticity of adhesions [99].
Splinting
Splints are usually required to maintain and increase ROM. Static splinting may be used most of the time during the first 2–3 weeks to immobilize the joint in a position that maximizes the increased motion achieved in surgery and to protect the wound from disruption by excessive stresses. This may be continued at night for up to 12 weeks to prevent contraction of scar tissue, although the splint will need regular remolding to ensure the optimum position is maintained as edema subsides and ROM improves. In addition, dynamic or static progressive splints may be used intermittently during the day to passively increase ROM and lengthen structures not released by surgery [100]. As there is limited published research investigating the merits of different splinting protocols following contracture release, the splints discussed will be based on the author’s current practice; however, further research is required in this area.
Exercise
Active and passive ROM exercises should be commenced during the inflammatory period before fibroblasts lay the framework for the formation of new collagen. This will influence collagen alignment and orientation and optimize joint flexibility [95]. Early active mobilization will also minimize muscle atrophy and tendon-scar tissue adhesions; however, the newly forming collagen matrix is easily disrupted, and a balance must be achieved between protecting the wound and optimizing ROM. In practice, these patients are usually seen 1–2 days after surgery, where the postoperative dressings are reduced, light compressive dressings applied, and ROM and splinting commenced.
The patient needs to be prepared to carry out a frequent home exercise program. This should consist of gentle active and, providing there are no contraindications, passive ROM during the inflammatory and early proliferative phases. A place-and-hold technique is frequently used for the “passive” exercises in order to work on muscle recruitment and tendon gliding in addition to passive joint ROM. Exercise intensity and repetitions are increased as the proliferation phase progresses and remodeling begins. At this stage, the therapist may also use heat and passive stretches to maximize the flexibility of the soft tissue prior to treatment and joint mobilization techniques to improve joint glide.
Light, clean functional use of the hand is encouraged soon after surgery in order to prevent stiffness and maintain normal motor patterns. General isometric strengthening of the wrist is commenced approximately 1 week after surgery and is important to prevent deconditioning in patients that play competitive sport or usually carry out regular upper limb strength training. Cardiovascular exercise should be resumed only when the wound is healed to prevent wound breakdown or increased edema.
Strengthening of the affected hand is usually commenced at the beginning of the remodeling phase, once the wound is fully healed and pain and edema have subsided. Specific sports-related conditioning and heavy use of the hand are usually started at 6–8 weeks to allow sufficient tissue healing before heavier stresses are applied to the joint and surrounding soft tissues. Grip and/or pinch strength should be measured at this stage to highlight any deficit and allow improvement to be assessed. Upper limb proprioceptive training may also be required to facilitate the return to full musculoskeletal and athletic function [101].
Complications
Regular therapy input will allow monitoring of progress and prompt resolution of any postoperative complications. If there are signs of wound infection or delayed healing, medical attention should be sought. If ROM becomes restricted due to new scar tissue or tendon adhesions, the therapist should modify the rehabilitation program in order to address these issues. One rare but disabling complication of surgery or injury is the development of complex regional pain syndrome. This can present as marked edema, skin discoloration, increased hair growth, reduced ROM, and increased pain, all disproportional to the degree of tissue damage and continuing beyond the normal healing timescales [102]. In such instances, prompt referral to a specialist pain team and the use of pain management strategies, active mobilization, isometric strengthening, and functional restoration is recommended [102, 103].
8.1.3.5 Specific Rehabilitation Programs
There is limited published research investigating the efficacy of different rehabilitation methods after contracture release in the digits. In practice, rehabilitation is largely determined by which joint(s) have been released and the individual surgical goals. The common causes for contracture at each joint and the associated problems for ball sports athletes will be briefly discussed in the following section. Common postoperative therapy practices, with suggestions for ROM exercises, splinting, and strengthening, are outlined in Table 8.6. The timings for these interventions will depend on clinical presentation and the phase of healing, as discussed above. The number of therapy sessions and the length of treatment will depend on the nature of the surgery and the progress made within and between therapy sessions. Ideally the patient would be seen several times a week for the first 3–4 weeks to ensure that rehabilitation is advanced appropriately and to allow timely identification and management of any complications. Therapy is likely to continue until the patient has fully returned to their sport, or progress has reached a plateau, after which point it is unlikely that additional therapy will yield further gains. This plateau can be identified through continued use of objective measures during the later stages of rehabilitation, such as ROM, grip strength, and dexterity. However, full return to sport is usually planned for 12 weeks after surgery, with an expected ROM of slightly less than the intraoperative measure.
Table 8.6
Suggestions for postoperative rehabilitation after contracture release in the digits
Location of joint release and goals | Range of motion exercises | Splints | Strengthening exercises |
|---|---|---|---|
Dorsal MCPJ Increase active and passive MCPJ flexion Maintain or improve active MCPJ extension | Active Gross composite flexion/extension Isolated MCPJ flexion/extension with IPJs extended Isolated MCPJ flexion/extension with IPJs flexed Finger abduction/adduction Isolated extensor indices/extensor digiti minimi tendon gliding if index finger or little finger releases Passive and place-and-hold MCPJ flexion with IPJs flexed and extended Whole digit extension if MCPJ extension lag | Forearm-based position of safe immobilisation splint (Fig. 8.29a) Static progressive or dynamic MCPJ flexion splint (Fig. 8.29b) | General grip strengthening using graded sponge blocks or therapy putty Specific gripping activities replicating athlete’s sport using power-webs or other hand exercisers Intrinsic strengthening for isolated MCPJ flexion and abduction/adduction as preoperative contracture position will have limited function Wrist strengthening to counteract weakness due to postoperative immobilisation Dexterity training to improve motor skills |
Volar MCPJ Increase active and passive MCPJ extension Maintain or improve grip | Exercises as for dorsal MCPJ releases with the addition of: Passive IPJ flexion in MCPJ extension to stretch the intrinsics Place-and-hold digit extension to retrain extensors | Forearm-based MCPJ extension splint Dynamic MCPJ extension splint | General grip, wrist and dexterity work as with dorsal MCPJ release Resisted finger extension against putty or elastics Functional retraining including weight bearing through extended hand and wide gripping activities |
Dorsal PIPJ Increase active and passive PIPJ flexion Maintain or improve active PIPJ extension | Active Gross composite flexion/extension IPJ flexion/extension in MCPJ extension IPJ flexion/extension with MCPJs blocked at ∼70° flexion Isolated PIPJ flexion/extension Isolated DIPJ flexion/extension if DIPJ active ROM also reduced Passive and place-and-hold (caution must be taken if central slip released or injured previously) Isolated PIPJ flexion and combined DIPJ/PIPJ flexion prior to full gross composite flexion Emphasis on active/place-and-hold PIPJ extension following passive exercises | Hand or digit-based PIPJ extension splint (Fig. 8.30a) Hand or digit-based static progressive PIPJ flexion splints or elastic flexion strapping (Fig. 8.31) Dynamic PIPJ extension splint if extension lag (Fig. 8.30b) Exercise splint in MCPJ extension with IPJs free to target PIPJ ROM during exercise | Flexion strengthening with sponges, putty or other hand exercisers in MCPJ extension to strengthen the extrinsic flexors and in gross composite flexion to include the intrinsics Narrow grip activities encouraged to target maximum PIPJ flexion Resisted extension to strengthen intrinsic and extrinsic extensors Specific gripping activities to replicate the athlete’s sport Dexterity training to improve motor skills |
Volar PIPJ Maximise active and passive PIPJ extension Maintain or improve PIPJ flexion | Exercises as for dorsal PIPJ release with increased repetitions of: Passive and place-and-hold extension IPJ flexion/extension with MCPJs blocked at ∼70° flexion | Hand-based PIPJ extension splint, initially in MCPJ flexion if required (Fig. 8.31a) Dynamic PIPJ extension splint (Fig. 8.31b) | General grip and dexterity work as with dorsal PIPJ release Digit extension against putty or elastics Flicking Dynamic activities requiring digit extension, such as bouncing, throwing and catching |
First web-space Increase thumb abduction and opposition Maintain MCPJ and IPJ ROM | Active Opposition Palmar and radial abduction Gross composite thumb flexion/extension Passive and place-and-hold Abduction Composite thumb flexion | Abduction splint in mid-palmar thumb abduction (Fig. 8.32) | Pinch strengthening with putty or graded pegs Span activities, such as rehabilitation computer games with large grip attachments, opening/closing large lidded jars Grip strengthening in outer range |
Fig. 8.29
Splinting following dorsal MCPJ release. (a) Forearm-based “position of safe immobilization” splint. (b) Static progressive MPCJ flexion splint
Fig. 8.30
Extension splinting following PIPJ release. (a) Hand-based PIPJ extension splint. (b) LMB dynamic PIPJ extension splint
Fig. 8.31
Flexion splinting following PIPJ release. (a) Hand-based static progressive PIPJ flexion splint. (b) Digit-based static progressive PIPJ flexion splint. (c) Elastic flexion strapping
Fig. 8.32
First web-space abduction splint following first web-space release
Metacarpophalangeal Joint (MCPJ)
Reduced MCPJ flexion caused by chronic thickening of the dorsal capsule, shortening of the collateral ligaments, or dorsal skin scarring can lead to significant functional limitation, especially at the ring and little fingers, where MCPJ flexion contributes to power grip. Dorsal MCPJ release will increase MCPJ flexion with the goal of improving grip patterns and strength; however, tethering of the extensor tendons is common due to their superficial location at the MCPJ. Appropriate scar management is therefore essential to prevent the development of an associated MCPJ extension lag. Contractures limiting MCPJ extension are less frequent, but may result from chronic intrinsic tightness with secondary contracture of the volar plate [95]. There are few published studies looking at outcomes following MCPJ release, with much of this data originating from the 1970s. Anecdotal reports suggest that MCPJ releases are effective in increasing the overall function of the hand, but that maintaining intraoperative ROM is a challenge, especially at the ring and little fingers [95].
Proximal Interphalangeal Joint (PIPJ)
Injuries to the PIPJ are common in ball sports. Injuries that are particularly vulnerable to residual joint stiffness include intra-articular proximal phalanx fractures, fracture dislocations, central slip avulsions, and deep zone II flexor tendon lacerations [95]. Tenolysis is frequently performed in conjunction with joint release surgery at the PIPJ, necessitating a focus on active tendon gliding throughout rehabilitation. Dorsal PIPJ releases may be indicated when flexion is reduced and grip strength and/or grip control is affected. Volar releases are indicated when the restriction to PIPJ extension prevents the movement of the digit away from the ball during a catch. Without intervention, the digit may become repeatedly reinjured leading to a worsening of the contracture. Early rehabilitation following dorsal or volar PIPJ releases requires careful wound dressing to ensure minimal restriction to PIPJ flexion. Range of movement exercises need to be performed regularly as the PIPJ soon becomes stiff and scar tethering can occur. A review by Hogan and Nunley [94] suggested an average of 25–30° improvement in ROM is achieved with surgery for PIPJ flexion deformities. A lack of uniformity between studies prevented comparison of different treatment techniques; however, a need for close follow-up and regular therapy was emphasized.
Distal Interphalangeal Joint (DIPJ)
Contracture at the DIPJ that is sufficient to limit function is uncommon; pain and joint instability are usually more problematic, and arthrodesis in functional position may be the best option [104].
First Web Space
A large ROM at the MCPJ and IPJ of the thumb is not essential for functioning; however, contraction of the first web space limits opposition and notably affects function [93, 105]. Adduction contracture may result from scarring following open injury, prolonged immobilization in a poor position, or reduced ROM at the first carpometacarpal joint (CMCJ) following fracture, ligament damage, or osteoarthritis. Fracture, dislocation, and osteoarthritis of the CMCJ are discussed elsewhere (Sects 7.1.2, 7.2.2, and 8.5.1). For soft tissue restrictions to thumb abduction/opposition, such as scarring or tissue shortening, serial splinting should be trialed prior to surgery. If this does not restore sufficient abduction, contracture release is required. In severe cases, a CMCJ trapeziectomy or arthroplasty may be necessary (see Sect. 8.5.3). A recent study of 11 patients found that full abduction was achieved after first web-space release, but that opposition and grip strength remained limited. Patients with less opposition reported lower levels of functioning [106].
Complex Contractures
If the contracture release involves more than one joint on the same digit, or multiple joints on the same hand, splinting will need to be modified to incorporate the combination of joints released. Similarly, the exercise program should address ROM at each affected joint as well as in composite function. In these situations, it is essential to discuss priorities with the surgeon and patient and to ensure that sufficient emphasis is given to the joint(s) with the most important functional role.
Pediatric Patients
The rehabilitation process is slightly different for children as they can usually tolerate longer periods of immobilization without developing global hand stiffness. Postoperative management may involve 3–4 weeks full-time splinting or casting at end range for the operated digit. Mobilization and functional activities are commenced after this period, with night splinting continued for a further 4–6 weeks.
Key Points
For the ball sports athlete, the goals of rehabilitation following contracture release are always to maximize the available active ROM while allowing appropriate tissue healing. The therapist must use their clinical judgment to consistently find the balance between these opposing factors:
Pitfall
Potential consequences
Insufficient preoperative patient education
Reduced compliance with therapy and unrealistic expectations
Insufficient postoperative patient education
Poor compliance or overuse of splints
Aggressive early mobilization
Increased edema and delayed healing
Delayed postoperative therapy input
Tendon adhesions and soft tissue tightening
Poorly fitting or inappropriate splinting
Unnecessary restrictions to ROM, discomfort, and skin breakdown
Premature return to sports
Reinjury and increased edema
Emphasis on isolated ROM
Deconditioning and delayed return to full functioning
Discontinuing therapy too early
Lack of appropriate ROM, strengthening, and scar management progression
8.1.3.6 Conclusions
At present, therapy input should be guided by the nature of surgery, the stages of wound healing, and the patient’s particular goals. The role of splinting should not be overlooked, and a graded return to sports-related hand function is encouraged.
There is a lack of comprehensive research into the optimum rehabilitation program following contracture release in both the general population and ball sports athletes. Further investigation is needed to establish the functional ROM required for different ball sports activities in order to address the impact of contracture at the different joints. In addition, comparisons of the efficacy of different splinting programs and rehabilitation protocols would enable standardized evidence-based practice, and investigation of the difference between intraoperative ROM and final functional motion would lead to more accurate postoperative prognoses.
Suggested Readings
Hogan CJ, Nunley JA (2006) Posttramatic proximal interphalangeal joint flexion contractures. J Am Acad Orthop Surg 14:524–533
A review of published outcomes following surgical release of the volar PIPJ. Sixteen studies were identified, nine included information on postoperative splinting. The specific search criteria were not documented. The duration of splinting ranged from 4 weeks to 6 months. The type of splint was not mentioned and ROM measures were not comparable between studies.
Masden D, Higgins J (2011) Predictors of successful outcomes in first web space contracture release. Hand 6(1):50–55
An assessment of ROM and DASH scores within 7 years of first web-space release. Eleven participants were included, ten of whom had posttraumatic contractures. There was no significant difference between radial or palmar abduction of the affected and unaffected hands. Opposition and grip strength were significantly less in the affected hand. There was a moderate correlation between opposition of the affected hand and DASH score.
Glasgow C, Tooth L, Fleming J (2008) Which splint? Dynamic verses static progressive splinting to mobilise stiff joints in the hand. Br J Hand Ther 13(4):104–110
A discussion of the literature and theory behind dynamic and static progressive splinting to increase finger ROM. The authors highlight a lack of evidence behind the common assumption that static progressive splints are more effective in contracture resolution. They suggest that dynamic splints maximize the time a joint is held at optimal end range, promoting greater tissue growth. Postoperative splinting was not specifically discussed.
8.2 Old Tendon Injuries
8.2.1 Secondary Surgery of Finger Extensor Mechanism (Excluding Zones 7 and 8)
Abstract
Secondary reconstruction of the finger extensor mechanism following neglected lesions or failed treatment is difficult and leads to poor results compared to a satisfactory initial treatment. Appropriate treatment in emergency should be emphasized. Without correct treatment, a complete discontinuity of the extensor mechanism will lead to a progressive deformation of the finger with some degree of disability, particularly during ball sports. The extensor mechanism is a result of the fusion of the extrinsic and intrinsic tendon systems. It is a complex structure, and a lesion at any level may create an imbalance of the subtle arrangement between these two tendon systems. Swan neck and boutonnière deformities are typical examples. Surgical correction of these deformities is indicated only if the finger has a passive range of motion (dynamic splints or surgery may be required). In this chapter, we will describe the consequences of extensor mechanism discontinuity from distal to proximal, following Verdan’s classification. At each stage, we will describe the surgical techniques and the preferred treatment in ball sportsmen.
Directly underlying the fine dorsal skin, extensor tendons are poorly protected against laceration or subcutaneous rupture and are particularly exposed during ball sports. Reconstruction of chronic lesions is difficult and less satisfactory than initial repair. Importance of a satisfactory primary treatment should be emphasized.
8.2.1.1 Pertinent Anatomy and Physiology
Fingers
The extensor mechanism results from the fusion of the extrinsic (extensor tendons) and intrinsic (interosseous and lumbricals) tendon systems.
Extrinsic System
Except under the extensor retinaculum, the extensor mechanism has no synovial sheath. On the dorsal side of the hand and just proximal to the metacarpophalangeal joints (MCP), the tendons are joined by transverse fibrous bands called juncturae tendinae. At the MCP level, a fibrous expansion stems from the deep surface of the extensor tendon and inserts on the base of the proximal phalanx and the dorsal joint capsule. This expansion is under tension only in complete hyperextension of the MCP [107]. Each extensor tendon divides into three bands at the dorsal side of the proximal phalanx; the central slip inserts on the dorsal base of the middle phalanx, and two terminal bands reunite forming a conjoined tendon on the base of the distal phalanx.
Intrinsic System
Deep insertions of the interosseous muscles follow two different patterns [107]:
Osseous insertions on the lateral tubercle of the base of the proximal phalanx
Capsular insertion on the distal part of the MCP palmar plate
Superficial insertions follow three patterns (Fig. 8.33):
Proximal insertion form the sagittal bands (transverse fibers of the interosseous hood)
Middle insertions form the oblique fibers of the interosseous hood
Distal insertions:
The central fibers join the central slip and insert onto the base of the middle phalanx
The lateral fibers join the lateral tendons and insert onto the base of the distal phalanx
Fig. 8.33
Distal superficial insertions of the interosseous muscles. 1 Lateral fibers, 2 Central fibers, 3 Oblique fibers, 4 Sagittal bands, 5 Lumbricals, 6 Extrinsic tendons, 7 Central slip, 8 Lateral tendons. (G. Chick © 2012, all rights reserved)
Stabilizing Structures
The extensor mechanism is stabilized by transverse structures, which prevent its lateral dislocation in flexion (Fig. 8.34).
At the MCP level, each extensor tendon is passively maintained by the sagittal bands (insert onto the intermetacarpal ligament) and the expansions of the interosseous muscles which extend distally from the sagittal bands. This second stabilizing structure is dynamic.
At the proximal interphalangeal joint (PIP) level, the central slip and lateral tendons are connected to the flexor tendon sheath by the transverse retinacular ligament. The triangular ligament stabilizes both lateral tendons at the dorsal side of the middle phalanx, thus preventing their dislocation palmarly.
Fig. 8.34
Stabilizing structures of the extensor mechanism: 1 Transverse retinacular ligament, 2 Oblique retinacular ligament, 3 Triangular ligament, 4 Central slip, 5 Lateral bands. (G. Chick © 2012, all rights reserved)
Thumb
The extensor mechanism of the thumb results from fusion of an extrinsic system (extensor pollicis longus and extensor pollicis brevis) and an intrinsic system (abductor pollicis brevis, adductor and flexor pollicis brevis). The intrinsic system stabilizes the extensor pollicis longus on top of the first metacarpal head and contributes to the extension of the distal phalanx of the thumb.
Physiology
At the MCP level, extension relies on the extensor digitorum communis (ECD), extensor indicis proprius (EIP), and extensor digiti minimi (EDM). Lumbricals only participate in the regulation of extension.
At the PIP level, extension is mainly achieved by the lumbricals. The interosseous muscles and extensor tendons participate only when the MCP is in complete extension.
In the thumb, the EPL is essentially responsible for MCP extension and IP hyperextension. A complete EPL laceration provokes a swan neck deformity secondary to excessive tension on the EPB. Complete EPB and sagittal band rupture provokes a boutonnière deformity secondary to palmar dislocation of the EPL and MCP flexion.
Verdan’s Classification
The topographical classification of extensor tendon lacerations was described by Verdan and adopted by the International Federation of the Societies for Surgery of the Hand (IFSSH) (Fig. 8.35). This classification includes 8 zones in the fingers and 5 zones in the thumb, numbered from distal to proximal. The odd numbers coincide with the joints.
Fig. 8.35
The topographical classification of extensor tendon lacerations following the International Federation of the Societies for Surgery of the Hand (IFSSH). 8 zones in the fingers, 5 zones in the thumb (T) numbered from distal to proximal. (G. Chick © 2012, all rights reserved)
8.2.1.2 Secondary Lesions of the Extensor Mechanism in the Long Fingers
The consequences of extensor mechanism discontinuity will be presented from distal to proximal. Zones 7 and 8 are excluded.
Chronic Mallet Injuries Without Swan Neck Deformities (Zone 1)
Four weeks after the initial injury the lesions is considered as chronic [108].
Clinical Findings
Following untreated lesions, inappropriate or failed treatment, detachment of the extensor tendon from the base of the distal phalanx—with or without bone avulsion—may result in a permanent lack of extension of the DIP. This deficiency results in a cumbersome finger and some degree of disability particularly during ball sports.
The joint is usually swollen with local inflammation and skin fragility. The condition of the skin is crucial for treatment decision to avoid infection and skin dehiscence. Active range of motion and strength should be evaluated. In case of swan neck deformity, the other fingers and the contralateral hand should be systematically checked. Likewise, congenital hyperlaxity should be looked for.
Investigations
X-rays may show fractures, foreign bodies, or osteoarthritis.
Treatment
Conservative treatment is preferred in moderate deformity and disability, particularly if the joint is already stiff.
Conservative Treatment
Old mallet fingers without fracture or with bone fragments smaller than one-third of the articular surface may still be treated with a dorsal splint even after several months. The results seem to be comparable in secondary and acute cases [108]. Details of this treatment are given in the chapter dedicated to acute lesions.
Surgical Treatment and Postoperative Care
Surgical treatment includes secondary tendinous and dermotendinous repairs. DIP fusion is a salvage procedure for stiff or arthritic DIP joints.
Surgical Access to DIP
Care must be taken not to damage the nail matrix and to avoid cutaneous dissection and consequent skin necrosis. Access to the distal extensor insertion is through an H-shaped incision or a bilateral fishtail transverse incision into the joint crease (Fig. 8.36a).
Fig. 8.36
DIP fusion using memory staples. (a) An H-shaped approach. (b) Access to the joint after resection of the tendon callus. (c) Cartilage resection. (d) Insertion of the staple. (e) Compression effect of the staple. (G. Chick © 2012, all rights reserved)
Secondary Tendinous Repair (Tendon Advancement into the Bone)
The retracted distal extensor tendon and the fibrous tissue are exposed. Approximately 2–3 mm of fibrous tissue are resected, and the tendon is moved distally up to the bone and fixed using an anchor or a pullout suture. The DIP is stabilized in neutral position with 1 or 2 Kirschner wires for 6 weeks. After the wires are removed, a splint is prescribed for 2 additional weeks. When there is a persistent DIP lack of extension despite fusion of a small bone avulsion, the same procedure may be indicated, including bone fragment excision.
Dermotenodesis or Brooks-Garner Procedure
This technique [109], initially described by Brooks and Garner, is a transverse en bloc elliptical excision including skin, fibrous tissue, and callus. Skin and tendon are repaired as a single layer. A Kirschner wire is used to hold the DIP joint in neutral position for 6 weeks. Following wire removal and physiotherapy, a residual extension lag is usually observed.
Mallet Finger with Tendon Defect
Tendon grafts are not recommended [110]. Because these tendon defects are secondary to open injuries, DIP pining in extension for 6 weeks may encourage a subcutaneous fibrosis reaction and provide a functional tendon substitute [110]. During this treatment, PIP joint hyperextension should be prevented by a Beasley ring in order to avoid a swan neck deformity. DIP fusion is also an option.
DIP Fusion
DIP fusion is a salvage and definitive solution. It is indicated following failure of mobility-sparing procedures or in case of osteoarthritis or a stiff and painful joint. It may also be indicated when a bone avulsion is bigger than one-third of the articular surface. The degree of flexion of the joint should be adjusted considering finger opposition to the thumb: The recommended flexion is usually 0° for the index finger, 15° for the long finger, 20° for the ring finger, and 25° for the little finger.
Several devices are available for bone fixation. Each of these devices has pros and cons. The most common approach is a crossbow dorsal incision centered over the DIP joint. After dorsal capsulotomy, the joint is dislocated and thorough inspection of the cartilage usually shows that it is completely worn out. The cartilage of the head of the middle phalanx is excised with an oscillating saw. The cartilage of the base of the distal phalanx is usually more brittle and is removed with a rongeur.
K-Wire Fixation
Under fluoroscopy, a 10/10-mm K-wire is introduced in an in-and-out fashion from the distal into the middle phalanx. It is necessary to add an oblique anti-rotational K-wire. Both K-wires are cut subcutaneously. The drawbacks of this technique are pulp irritation by the extremity of the K-wire and a higher nonunion rate because of absence of compression. A complementary immobilization is mandatory until fusion is obtained, usually after 3 months.
Screw Fixation
Compression provided by screws increases the fusion rate. The main drawback of this technique is the inevitable extension of the DIP due to the strict positioning of the screw inside the medullary canal. The head of the screw may also irritate the pulp, but this inconvenience may be avoided by using headless screws.
Staple Fixation
New-generation staples provide stable fixation with compression without any pulp irritation. These memory staples are fixed inside the medullary canal, and compression is provided by the expansion of the distal and proximal segments (Fig. 8.36). A short immobilization is necessary for 2–3 weeks, after which the finger is left completely free. The results are encouraging but need to be confirmed. Nonunion is not rare, but most often well tolerated.
This last arthrodesis technique is the best option for ball sports because it avoids pulp irritation. Return to sport activity is proposed, provided that the joint is pain-free, after 6–10 weeks. The sequelae are minor or even absent when the ball is small as in handball.
Preferred technique in sportsmen in case of chronic mallet finger without swan neck deformity:
After failure of conservative treatment: Brooks-Garner technique
After treatment failure, osteoarthritis, painful stiffness, or fracture exceeding 1/3 of the total articular surface: definitive DIP fusion preferably with staples
Chronic Mallet Injuries with Swan Neck Deformity (Zone 1)
Physiopathology
Swan deformity is a PIP hyperextension combined with a DIP flexion (Fig. 8.37).


Fig. 8.37
Swan neck deformity following distal avulsion of the extensor mechanism
Each of these joint deformities provokes the other one, hence their functional interdependency. The swan neck deformity—which has various causes—leads to a simultaneous flexion and extension dysfunction.
In a late posttraumatic context, the swan neck deformity results from an old distal extensor mechanism lesion. Mismanaged, this initial tendon injury heals with an elongated callus and consecutive deficit of active DIP extension. The resulting tension of the central slip provokes a PIP hyperextension. This hyperextension is facilitated by palmar plate laxity and weakness of the transverse retinacular ligaments. Eventually, dorsalization of the lateral bands increases PIP hyperextension, and the traction of the flexor digitorum communis (FDP) increases DIP flexion (Fig. 8.38).
Fig. 8.38
Swan neck deformity. 1 Oblique retinacular ligament, 2 Lateral bands, 3 Transverse retinacular ligament, 4 Central slip, 5 Flexor digitorum profundus, 6 Tendon sheath. (G. Chick © 2012, all rights reserved)
Diagnosis
The diagnosis is evident when active extension provokes a deformity associating PIP hyperextension and DIP flexion. Both lateral bands form two conspicuous bands lifting the skin at PIP level. During active flexion of the finger, the movement starts in the DIP joint prior to the MP joint and ultimately in the PIP which may present a triggering effect.
If the deformity is not fixed, passive correction of the PIP hyperextension allows active extension of the DIP. This test proves that the distal flexion deformity is secondary to PIP hyperextension.
Differential Diagnosis
Physiologic swan neck deformities and patients with PIP hyperlaxity.
Swan neck deformities of articular origin, secondary to a periarticular lesion of a structure that normally prevents PIP hyperextension: palmar plate, flexor digitorum superficialis (FDS).
Other etiologies are of extrinsic or intrinsic origins: Extrinsic origins are related to an excessive traction of the central slip. Intrinsic etiologies are related to excessive traction of lumbricals and interosseous muscles, leading to PIP hyperextension, dorsal migration of the lateral tendons, DIP extension deficit, and DIP flexion deformity (Fig. 8.39).

Fig. 8.39
Swan neck deformity following neglected mallet finger of the little finger. Note the physiologic hyperextension of the other fingers
Treatment
The treatment of swan neck deformity must target the etiology of the deformity. Palliative treatments are considered if the cause is not amenable to treatment. Palliative treatments address PIP hyperextension. Simultaneous correction of the DIP flexion should be performed in all cases in order to prevent a recurrence of the swan neck deformity.
Many surgical procedures have been described.
Fowler’s Technique
Transection of the extensor tendon proximal to the PID joint allows rebalancing of the extensor mechanism by proximal retraction of the lateral bands and the callus. There is no risk of boutonnière deformity as long as the triangular ligament remains intact. This procedure is indicated for old mallet fingers with a DIP active extension deficit inferior to 35° in a reducible and flexible swan neck deformity.
The surgical technique [111] is performed through a short oblique incision at the dorsal side of the middle phalanx under local anesthesia and sedation. The tenotomy of the central slip is performed proximal to the triangular ligament which must be left intact. Active DIP extension is controlled preoperatively. After skin closure, two distinct splints are attached. One limits PIP extension over 20°, and the other one maintains the DIP in complete extension. Flexion of the PIP joint is still possible. The DIP splint is removed several times a day in order to allow active flexion exercises. Both splints are removed after 4 weeks.
Grunberg and Regan [112] demonstrated an improvement of DIP extension of 28° compared to the preoperative condition. Houpt et al. [113] report on complete extension recovery in 26 out of 35 patients. According to Chao et al. [114], this tenotomy does not completely correct the DIP extension lag, particularly when it is superior to 36° initially (partially over 46°).
However, even if the improvement is not complete, this technique is recommended in sportsmen because: The improvement in DIP extension may significantly ameliorate the function of the finger. The procedure is simple with minimal morbidity and allows early return to sports.
Shortening of Palmar Structures
Shortening of a palmar PIP structure maintains the joint in slight flexion and prevents hyperextension while allowing flexion. It is possible to shorten:
The skin: Dermodesis
The FDS: Swanson’s tenodesis [115]. The FDS is not interrupted, but is fixed into the neck of the proximal phalanx in order to maintain the PIP joint at 30° flexion. This tenodesis must be protected by a transarticular K-wire for 2 months.
The palmar plate: Capsuloplasty. The palmar plate is translated proximally and fixed onto the collateral ligaments.
Combination of two simultaneous procedures: Shortening of the palmar plate and FDS tenodesis by the Goldner procedure which preserves active flexion. This technique consists in the fixation of the distal end of the severed FDS onto the neck of the proximal phalanx and suture of its proximal end on its original insertion (ln 1).
Tenodesis Procedures Using Parts of the Lateral Bands of the Extensor Mechanism
The aim of these techniques is to reconstruct a pseudo-retinacular ligament that crosses the PIP joint anterior to its rotational axis. The swan neck deformity is corrected by stabilization of the PIP joint in slight flexion preventing hyperextension and also by restoration of DIP active extension. These procedures were described by Littler and subsequently by Zancolli with two variations [116].
Harvesting of the transferred slip is identical for all the techniques: Through a dorsolateral approach, the intrinsic lateral tendons of the extensor mechanism are exposed. A distally based lateral slip is taken from its lateral side (Fig. 8.40) after release of the oblique expansion of the retinacular ligament.
Fig. 8.40
Swan neck deformity correction by tenodesis using a slip from the lateral band. (G. Chick © 2012, all rights reserved). Illustration inspired by Revol and Servant [107]
The transferred slip may be rerouted following three patterns:
Under the cutaneous ligament of Cleland (Littler’s procedure)
Obliquely under the palmar plate (Zancolli’s 1, 1968)
Rerouted inside the flexor tendon sheath, entering at the level of the proximal edge of the A4 pulley, and coming out proximally to the PIP joint, at the distal edge of the A2 pulley (Fig. 8.41)
Postoperatively, the wrist should be immobilized in slight extension, MP flexion, and PIP and DIP extension. The splint should be kept for 4 weeks, followed by physiotherapy with a short digital protective splint that maintains the DIP joint in neutral extension for several weeks.
The use of the lateral tendon depends on the quality of the terminal tendon. In chronic mallet fingers, this is usually not good enough, and Zancolli-type-like techniques are not recommended.
Active Tenodesis SORL
The spiral oblique retinacular ligament reconstruction (SORL) was described in 1978 by Thompson et al. [117]. The aim of this technique is to recreate a spiral oblique retinacular ligament in order to correct swan neck deformity while sparing the integrity of the extensor mechanism itself. As distinct from the former tenodesis, this technique is appropriate for the treatment of mallet fingers with or without swan neck deformity. The procedure is a crossed dynamic tenodesis using a tendon graft (palmaris longus or plantar) that provides automatic extension of the DIP during active extension of the PIP (Fig. 8.42).
Fig. 8.42
SORL tenodesis (following Thompson and Littler). (1) Swan neck deformity ((a) Slack lateral band, (b) central slip, (c) palmar plate). Diagram of the graft: (2) lateral and (3) anteroposterior views. (G. Chick © 2012, all rights reserved)
The technique starts with a dorsal approach of the base of the distal phalanx. An anteroposterior canal is drilled through the base of the distal phalanx at the level of the normal insertion of the terminal extensor tendon. Another incision is made at the dorsoradial side of the PIP joint and a third one on the ulnar side of the proximal phalanx. After careful subcutaneous undermining, the graft is driven from the distal phalanx, along the radial side of the middle phalanx following the extensor lateral band, passes between the pedicle and the tendon sheath to reach the ulnar side of the proximal phalanx. A transverse osseous canal is drilled in the base of the proximal phalanx. The graft is fixed by two buttons, one on the pulp and the other one at the ulnar side of the proximal finger, after adjustment of the tension. The tension is appropriate when the PIP and DIP joints are in neutral position. Excessive tension must be avoided to prevent a boutonnière deformity. Postoperatively, the finger must be immobilized for 3 weeks in an intrinsic plus position before active mobilization is started. Kleinman [118] modified this original technique by pinning the DIP in neutral position and the PIP at 15° of flexion for 4.5 weeks and 3 weeks, respectively.
PIP Fusion
The fusion of the PIP joints is performed in various positions depending on the finger. It is a salvage procedure that puts an end to the sports career.
Recommended technique in sportsmen in case of chronic mallet finger with swan neck deformity:
When the DIP extension lag does not exceed 40°, Fowlers technique with simultaneous correction of the DIP flexion deformity is recommended.
When the DIP extension lag exceeds 40–45°, the SORL technique is used.
Middle Phalanx (Zone 2)
Injuries at the dorsal side of the middle phalanx may affect one or—less frequently—both lateral bands and/or the triangular ligament. Chronic lesions may lead to a DIP extension deficit or a swan neck deformity. The SORL tenodesis is an appropriate treatment for this condition. The reconstruction of one of the lateral tendons seems inappropriate in sportsmen.
Chronic Zone 3 Closed Injuries—Boutonnière Deformity (Zone 3)
Boutonnière deformities are usually secondary to central slip lacerations or avulsions (closed injury) with or without bone avulsion. This lesion occurs mainly in three circumstances during sports:
PIP Palmar dislocation
Forced flexion of an extended PIP
Direct trauma on the dorsal side of a flexed PIP
Mechanism of the Deformity
The rupture or avulsion of the central slip leads to a proximal migration of the extensor mechanism. The middle phalanx, only submitted to the force of the FDS, flexes without resistance and the triangular ligament stretches. Accordingly, the transverse retinacular ligaments retract progressively, pulling the lateral bands anterior to the PIP axis, thus acting as flexor tendons. The PIP joint extrudes between the two lateral bands as through a buttonhole. The DIP extends under the increased traction of the terminal tendon, and the hyperextension is progressively fixed by retraction of the oblique retinacular ligaments (Figs. 8.43 and 8.44).

Fig. 8.43
Boutonniere deformity. 1 Central slip, 2 lateral band, 3 central fibers. The rupture or avulsion of the central slip leads to a proximal migration of the extensor mechanism. With PIP flexion, lateral bands migrate volar to the axis of rotation of the proximal interphalangeal joint. (G. Chick © 2012, all rights reserved)

Fig. 8.44
Boutonnière deformity of the left ring finger. Notice the mallet finger deformity of the fifth finger
Skin vitality, active and passive ranges of motion, and functional impairment must be evaluated. Distinction between reducible and fixed deformity with retraction of the retinacular ligaments should be made. Haines test (Fig. 8.45) reveals a retraction of the oblique retinacular ligament. Initially, DIP hyperextension is reducible in any PIP position. Later, oblique retinacular ligament retraction limits DIP flexion when PIP is maintained in extension (positive Haines test).
Fig. 8.45
Haines test: The PIP joint is maintained in extension. It is impossible to passively flex the DIP due to oblique retinacular ligament retraction (fixed deformity). (G. Chick © 2012, all rights reserved)
Investigations
Lateral view of the PIP is sufficient (Fig. 8.46a). MRI may show an elongated callus of the central slip and shows the sheath and pulleys (Fig. 8.46b).
Fig. 8.46
(a) Strict lateral view. (b) Sagittal MRI shows palmar plate avulsion of the fifth PIP and a chronic rupture of the A2 pulley resulting in a bowstring deformity
Classification
Burton [119] described a classification of chronic boutonnière in three stages, to which Strauch [111] added a fourth stage:
Stage I—Flexible joints, reducible deformity. Passive PIP and DIP complete ranges of motion. Recent lesions.
Stage II—Fixed contracture, retracted lateral bands. The Haines test is positive, secondary to oblique retinacular ligament retraction. DIP flexion is still possible when PIP is flexed.
Stage III—Fixed contracture, joint fibrosis, collateral ligament, and palmar plate retraction. Passive ranges of motion are limited because of soft tissue retraction. Complete flexion of the finger is no longer possible.
Stage IV—Stage III + PIP joint osteoarthritis [111]. Limitation of passive mobility due to joint surface damage.
Treatment
Treatment protocol of this vicious circle of deformity depends on the reducibility of the boutonnière.
In a stiff boutonnière deformity, even after several months post-injury, physiotherapy including PIP extension splints and passive and active DIP mobilization must be tried. When complete PIP extension is obtained, dynamic splints must still be applied for 6–12 weeks. When complete PIP mobility cannot be obtained by conservative treatment, surgical arthrolysis including collateral ligaments release is necessary (Fig. 8.47). This may be the first stage of a two-stage procedure.
Fig. 8.47
PIP stiffness: (a) clinical picture, (b) lateral view, (c) anterior arthrolysis. The FDP tendon is shown on a vascular sling. Lateral slips of the FDS are seen anterior to the palmar plate
When complete PIP extension is obtained through conservative or surgical arthrolysis, many surgical options have been proposed. Indications depend on the stage of the deformity, level of disability, and characteristics of the lesion. Extensor mechanism reconstructions and tenotomies may be used separately or combined. These operations must be reserved to expert surgeons, in association with precise rehabilitation protocols that will be continued several months postoperatively [118].
Dolphin’s Distal Extensor Tenotomy [120]
Distal extensor tendon is exposed through a dorsal incision. The level of the tenotomy of the distal extensor tendon should be distal enough to preserve the distal insertion of the oblique retinacular ligament that is responsible for DIP extension during PIP extension. To restore DIP flexion limited by oblique retinacular ligament retraction, several surgical options have been proposed. Among these different techniques, mesh graft-like lengthening [121] has been proposed: There is no complete interruption of the extensor tendon, hence no suture and no postoperative immobilization. The procedure is performed under distal—purely sensitive—nerve block in order to precisely adjust the adequate lengthening through staged incisions according to the intraoperative recovery of active flexion.
Reconstruction of the Extensor Mechanism
Curtis reconstruction technique [122] recommended by Strauch [111] includes three successive stages (Fig. 8.48) which are adapted according to the progressive evolution of the treatment. All these procedures are performed under local anesthesia, and complete PIP mobility is always required. Local anesthesia allows continuous testing of active extension by the surgeon.
Fig. 8.48
Curtis’ staged reconstruction of boutonnière deformity: (a) Surgical approach. (b) Extensor tenolysis. (c) The transverse retinacular ligament is released and transected if necessary, allowing the lateral bands to migrate dorsally. 1 Lateral band, 2 Transverse retinacular ligament, 3 Transected transverse retinacular ligament. From Curtis et al. [122], illustration inspired by Strauch [111]. (G. Chick © 2012, all rights reserved)
A lazy S approach is made on the dorsal side of the PIP joint. The transverse retinacular ligament is released distally and proximally, and a tenolysis of the extensor tendon is performed. If complete extension is recovered, the procedure is finished.
When active extension is still incomplete, the transverse retinacular ligament is transected, allowing dorsal shift of the lateral bands. Complete active extension is recovered in 30–40 % of the cases, and a postoperative immobilization program is started with MCP at 70° of flexion and PIP and DIP in extension for 1 week. A PIP dynamic extension splint is then applied.
When a lack of active extension of 20° or less persists, a Fowler’s tenotomy is performed [123]. When active extension is complete, the procedure is finished (Fig. 8.49).
When extension deficit exceeds 20°, Curtis recommends shortening the central slip. His technique is to cut the central slip after release, to excise 4–6 mm, and to reinsert it at the base of the middle phalanx (Fig. 8.50). Reinsertion may be done using an anchor. The lateral bands are stabilized by repair of the triangular ligament by several sutures. Usually, the repair is protected by a trans-PIP 10/10 or 12/10 K-wire in extension for 5 weeks. Immediate DIP rehabilitation is encouraged to help early mobilization of the lateral bands.
After 1-year follow-up, Curtis et al. [122] reports 31° PIP extension improvement compared to the preoperative status with an extension deficit of 10°. For the patients who had a central slip reinsertion, the improvement was from 55° preoperatively to 17° postoperatively associated with an improvement of the postoperative flexion in 20 of 23 patients.
In case of a large tendon defect, a tendon plasty is necessary because the local fibrous tissues are not strong enough and should not be used. Using the palmaris longus for lateral band grafting is not recommended because of unreliable results. Several techniques have been proposed for central slip reconstruction (Fig. 8.51):
Fig. 8.51
Tendon plasties. (a) Snow’s plasty, (b) Burkhalter-Aiache’s plasty, (c) Littler-Eaton plasty. (G. Chick © 2012, all rights reserved)
Snow’s plasty uses a retrograde flap taken from the proximal part of the central slip that is flipped over distally at 180° and distally fixed onto the base of the middle phalanx with an anchor.
Burkhalter-Aiache’s plasty uses two longitudinal slips, taken from both lateral bands, that are sutured together dorsally over the PIP joint.
Littler-Eaton plasty uses both lateral bands that are cut at the level of the middle phalanx, proximal to the insertion of the oblique retinacular ligaments and lumbrical tendon. The two lateral bands are reflected longitudinally, displaced dorsally, and sutured together with PDS or Prolene stitches. This reconstructed central slip is reinserted at the base of the middle phalanx by an anchor.
A recent original technique [124] uses one slip of the FDS for central slip reconstruction (Fig. 8.52): The flexor tendon sheath is opened between A2 and A4 pulleys, thus exposing the distal FDS insertion on the middle phalanx. A transverse incision near A1 pulley exposes the FDS tendon that is split up to its insertion. The ulnar slip harvested for the plasty is cut at the A1 pulley level, preserving its attachment on the middle phalanx. A 3-mm anteroposterior canal is drilled into the base of the middle phalanx. The tendon slip is then passed through the canal from anterior to posterior and fixed dorsally to the central slip extremity by a strong Pulvertaft suture. Protected by a purely dorsal extension-blocking splint, gentle active early physiotherapy is started for 3 weeks.
Fig. 8.52
(a) Ulnar slip of the FDS tendon after tenotomy at the distal palmar crease level. This distally based tendon slip is then passed through a window between the A2 and A4 pulleys (b) 1 Radial slip of the FDS, 2 Remaining central slip of the extensor mechanism, 3 Ulnar slip of the FDS. (c) The tendon slip is then delivered from volar to dorsal through the base of the middle phalanx (d). The tendon is weaved into the remaining extensor over the proximal phalanx using the Pulvertaft technique. (G. Chick © 2012, all rights reserved)
The pioneers of this technique report on a clinical case with an end result of PIP active motion from 30° to 85°. In our own experience, we obtained the same result in two cases.
Oberlin et al. [125] described a reconstruction technique using the extensor indicis proprius (EIP), extended with palmaris longus graft. This must be considered as a salvage procedure for secondary surgery.
Indications in Sportsmen In Case of Chronic Boutonnière Deformity
There is no documented evidence evaluating the different surgical techniques or conservative treatment [126]. Publications report frequently on clinical cases or short series. There is general consensus on the broad lines of major indications [127]. Nevertheless, the choice of technique is subject to personal preferences and experience.
Stage 1: For acute lesions, the central slip should be repaired.
Stage 2: Anatomical reconstruction of the extensor mechanism as described par Curtis is the preferred option, staged according to the result of each step. In case of extensor tendon defect, our preferred method is to use a slip of the FDS tendon to reconstruct the central slip.
Stage 3: Rehabilitation and dynamic splint use are the first steps for treatment of stiff boutonnière deformities. Persistent refractory stiffness justifies arthrolysis. When complete PIP extension is recovered, indications are identical to stage 2.
When the flexion contracture is incompletely corrected and stays irreducible, any attempt at anatomical reconstruction will fail to restore satisfactory function, and indications should be excessively cautious. If disability is moderate, surgery should be avoided. Patients are usually disabled by the distal phalanx hyperextension that prevents complete flexion of the finger. A distal extensor tenotomy significantly improves the finger function.
Stage 4: Osteoarthritis precludes the former options. Surgical abstention, arthroplasty, or articular fusion should be considered. Functional results may be poor, and the patient should be informed.
Key Points
Treatment of a chronic deformity depends on its fixity.
Every fixed boutonnière must benefit from a rehabilitation and dynamic splint therapy before considering surgery.
An extension deficit of 20° of the PIP is usual in chronic boutonnière deformity. Surgery should not be considered at that stage because the results are unpredictable.
The different surgical options depend on the stage of the lesion and must be performed by specialized surgeons.
Proximal Phalanx (Zone 4)
Injuries of the extensor mechanism in zone 4 are usually partial considering the width of the tendon at the proximal phalanx level. If the initial laceration concerns less than 50 % of the tendon width and results in a permanent lack of extension, it is secondary to tendon adhesions. Conservative treatment is indicated. If the deficiency persists, tenolysis should be considered. If the initial injury is a complete laceration, excision of the elongated callus and secondary suture should be considered.
Metacarpophalangeal Joint (Zone 5)
Laceration in zone 5 results from a variety of causes.
Human Bites and Puncture by Human Teeth
These injuries may result in permanent deficiencies when the initial laceration is complete and the repair is postponed because of contamination; a secondary repair may thus be discussed when the wound is aseptic.
When the initial laceration is incomplete and results in lack of extension, a tenolysis is recommended after a sufficient follow-up period.
Tendon Laceration
If disability persists after an old laceration, resection of the elongated callus and secondary repair or tenolysis must be considered according to the type (partial or complete) of the initial lesion.
Injuries of the Sagittal Bands
Although rarely traumatic, injuries of the sagittal bands may result in extensor tendon subluxation at the MP level. This instability appears in case of discontinuity of the proximal 2/3 of the sagittal band usually following an injury of the radial sagittal band of the long finger. The position of this joint puts it at particular risk.
Sagittal Band Closed Rupture
The subluxation of the extensor tendon in flexion at the dorsum of the MP joint may mimic a trigger finger. It may be a cause of delayed diagnosis. Sometimes, the metacarpophalangeal joint stays in flexion, and ulnar deviation and the initiation of active MP extension are lost; when the finger is placed in extension, the position can be actively maintained. The contralateral side must be evaluated before surgery is considered, especially for congenital hyperlaxity. Rayan and Murray [128] described three types for these sagittal band lesions (Table 8.8).
Table 8.8
Rayan and Murray’s classification [128] of extensor tendons at the dorsum of the MP joint
Type I | Contusion without tear of the sagittal bands and without instability |
Type II | Tearing of the sagittal bands with snapping of the extensor tendon, but without complete dislocation |
Type III | Tendon dislocation into the groove between the metacarpal heads |
Type I and II: These lesions are rarely symptomatic although pain may persist for 1 year [128]. The condition is called “Boxer’s knuckle.” In case of persistent pain, edema, and limitation of mobility beyond 3 months, exploration is recommended by Koniuch et al. [129]. These authors report on nine patients with extensor tendon subluxation, with partial ulnar sagittal band tear in seven cases and radial tears in four. In 25 patients, they found a synovitis reaction around a foreign body, chondral lesions, or palmar plate avulsion. Following active physiotherapy and dynamic splinting, eight out of nine patients recovered complete function. All reported complete pain relief (Fig. 8.53).
Fig. 8.53
(a) Partial rupture of the radial sagittal band of the long finger (type 2) 3 weeks after the initial injury; (b) direct suture; (c) the repair is stable in MP flexion, thanks to a release of the ulnar sagittal band
Type III: In case of neglected injury or failed conservative treatment after 3 weeks, secondary direct suture of the ruptured sagittal band is usually still possible. After 3 weeks, direct suture is not possible, and several reconstruction methods have been proposed. These procedures were initially suggested for treatment of rheumatoid deformities (Fig. 8.54). They are rarely used primarily because initial treatment of the acute lesion is always preferable and because old lesions are usually reparable in these young patients.
Fig. 8.54
Extensor tendon instability at the dorsum of the MP joint. Different surgical options for secondary stabilization. (a) Direct suture is possible up to 3 weeks after injury. (b) Wheeldon plasty by suture of the ulnar sagittal band to the intermetacarpal ligament. (c) McCoy plasty. (G. Chick © 2012, all rights reserved)
In any case, the contralateral sagittal band should be released at the same time. This release should be performed as palmar as possible, namely, just adjacent to the intermetacarpal ligament. The ligamentoplasty should be long enough to allow complete excursion of the extensor tendon and MP joint flexion. Tensioning should be done at 50° flexion, which is the position of immobilization for 5 weeks. Intraoperatively, the stability of the extensor tendon on top of the MP joint should be tested during the complete articular range of motion. The technique described by Carroll et al. [130] and recommended by Strauch [111] uses a radial slip of the extensor tendon, harvested proximal to the MP joint and preserving its distal continuity. This slip is passed at the level of the radial collateral ligament and then sutured to itself, thus centralizing the extensor tendon. Postoperatively, the MP joints are immobilized in extension for 6 weeks before rehabilitation is started. The author [130] reports painless stabilization with complete extension recovery in all cases and no recurrence. Watson et al. [131] uses anchorage by the deep intermetacarpal transverse ligament. Immobilization of the MP at 20–25° of flexion for 3 weeks is recommended. Watson reports on 16 patients who recovered 90° of MP flexion on average without tendon instability. All the patients were pain-free. No complications were recorded, and no complementary surgery was necessary. McCoy and Winsky [132] uses anchorage on the lumbrical muscle. The ulnar juncturae tendinae may be used and fixed on the radial sagittal band remnants or on the deep intermetacarpal ligament as described by Wheeldon [133]. An active dynamic transfer using the lumbrical muscle has recently been described [134].
Metacarpal Level (Zone 6)
Untreated lesions at the metacarpal level result in a callus elongation which may lead to a lack of strength and pain. In old lesions, because of fibrous continuity, even a complete extensor digitorum communis (ECD) deficiency may not result in functional disability. Tendons severed at the metacarpal level do not retract, thanks to the support of juncturae tendinae. This allows secondary tendon repairs including callus resection and secondary direct suture, even after several weeks. When a direct suture is not possible, a side-to-side suture to the adjacent tendon or graft interposition may be considered. In case of large tendon defect, a two-stage reconstruction using silicone rods should be considered, particularly if the subcutaneous tissues are inadequate.
8.2.1.3 Secondary Lesions of the Extensor Mechanism of the Thumb
Mallet Thumb Injury (Zone T1 and T2)
Old lesions in zone 1 and 2 are treated similar to those in the long fingers.
Zone T3
Lacerations on the dorsal side of the thumb MP joint may damage the extensor pollicis longus (EPL), the extensor pollicis brevis (EPB), or both. The treatment of neglected lesions includes excision of the callus of elongation and a direct secondary suture. In case of permanent MP flexion due to EPB ulnar subluxation with forceful gripping of a racket, the tendon should be reduced and stabilized on the dorsum of the MP joint [135].
First Metacarpal Level (Zone 4) and Trapeziometacarpal Level (Zone 5)
Lacerations in zone 5 involve the EPB tendon, abductor pollicis longus (APL), and rarely the EPL. If there is no wound complication, the tendon is repaired by direct suture after callus excision. Isolated EPB defects should be preferentially treated by EPL tenodesis onto the EPB. In case of associated old lesions of EPB and EPL, EPL repair should be prioritized. Reconstruction may be performed using direct secondary suture, tendon graft, or possibly tendon transfer using the EIP.
8.2.1.4 Tenolysis of the Extensor Mechanism and Intrinsic System
Adhesions of the extensor mechanism may be difficult to demonstrate because it may be obliterated by associated retraction of the intrinsic system or retinacular ligaments. The diagnosis relies on a careful clinical examination.
Surgical treatment is considered only after failure of a well-applied lengthy conservative treatment. Postoperative rehabilitation and dynamic splinting should always be pursued long enough to consolidate the results.
Wide tissue undermining must be avoided as much as possible during tenolysis. Approaches must be short and far from the tendons in order to limit recurrence of adhesions between tendon and skin. A blunt periosteal elevator and a thin blade are usually effective. In zone 6 and further, it is necessary to use a drain to avoid hematoma [110].
Tenolysis in Zones 4-5-6
Adhesions of extensor tendons in zones 4-5-6 are demonstrated by the Kilgore test. Passive flexion of the proximal phalanx blocks the PIP and DIP in extension. Passive PIP flexion provokes MP hyperextension. This demonstrates adhesions of the extensor tendon on the metacarpal, the MP joint, and/or the base of the proximal phalanx.
During extensor tenolysis, care should be taken to separate the tendon from the joint capsule and to check the mobility of the interosseous expansions.
When the test is still positive at that point, it means that the extensor mechanism and the interosseous expansions are retracted. In this case, Kilgore suggests performing staged tenotomies—like mesh graft incisions—at the level of the proximal phalanx. Littler suggests resection of the central tendon and of the oblique fibers of the interosseous expansion at the level of the proximal phalanx. At this point, the test should be negative.
Kilgore’s test assesses the mobility of the extensor tendon and should not be mistaken for the Finochietto test, which assesses interosseous function. Normally, when the MP is held in extension, the middle phalanx can be flexed passively and actively. If this is not possible, it denotes blocking of the PIP joint is secondary to intrinsic system retraction. More evidence is brought by the inversed test where MP flexion relaxes the interosseous and allows middle phalanx flexion, thus confirming that the extensor mechanism is not involved. The treatment is to excise the oblique fibers of the interosseous expansions. In the most severe cases, interosseous muscle insertions should be released from the metacarpals [110].
Tenolysis in Zone 2
Adhesions of the extensor mechanism are frequent in zone 2 in boutonnière deformities. These adhesions are responsible for the DIP complete lack of flexion that is exacerbated by the retraction of the oblique retinacular ligament demonstrated by Haines’ test. Most often at this stage, tenolysis is not successful in restoring active motion; Dolphin’s tenotomy should be preferred.
Key Points
Tenolysis should be considered only after failure of a long-term conservative protocol.
Kilgore’s test evaluates the extensor mechanism and should not be mistaken for Finochietto’s test, which evaluates interosseous muscles function.
Suggested Readings
Garberman SI, Diao E, Peimer CA (1994) Mallet finger: results of early versus delayed closed treatment. J Hand Surg [Am] 19:850–852
The study was intended to evaluate two similar patient populations whose sole differentiating factor was time delay to initial treatment (before 2 weeks and after 4 weeks). Fourty patients with soft tissue and bony mallet finger were evaluated. A fracture fragment greater than or equal to one-third of the articular surface of the distal phalanx, open injuries, and DIP joint subluxation were excluded from analysis. Splinting was as effective in the delayed treatment population as it was in the early treatment population. The authors recommend extension splinting for early or late closed mallet fingers if they fulfill the selection criteria outlined. The success rate is equivalent or better than results previously reported for surgical treatment, and complications associated with surgery are avoided.
Ahmad F, Pickford MS (2009) Reconstruction of the extensor central slip using a distally based flexor digitorum superficialis slip. J Hand Surg 34A:930–932
The authors describe the successful use of a distally based slip of the flexor digitorum superficialis tendon for the reconstruction of an incompetent central slip of the extensor mechanism. The flexor digitorum superficialis tendon was transferred from volar to dorsal through the base of the middle phalanx and then woven through the extensor tendon over the proximal phalanx. The technique is straightforward and appears to be robust. One case report is described.
8.2.2 Old Flexor Tendon Injuries
Abstract
Reestablishing satisfactory function after a neglected flexor tendon laceration or a failed repair remains one of the most difficult challenges in hand surgery. One-stage grafting carries the risk of compromising existing function. This procedure is indicated only either when the patient requires the special action or when no extensive scarring or contracture of the finger is present. Otherwise, two-stage grafting is recommended. At the operation, the tendon sheath and pulley system should be preserved as much as possible—at least the A2 and A4 pulleys. Palmaris longus and plantaris are the best donor tendons because of their small size. Early mobilization may help limit the formation of adhesions. Closed flexor tendon ruptures can be caused by hidden pathologies of the carpal bones and joints. Radiocarpal arthrography was useful in identifying the site of the lesion responsible for the rupture. Free tendon grafting followed by early controlled mobilization is preferred, since use of the tendon of another finger as a tendon transfer may compromise function of the donor finger unnecessarily. To prevent recurrence of tendon rupture, the sharp bone must be resected. Flexor tendon adhesion can occur in phalangeal fractures, failed primary tendon repairs, crush injuries, infections, and flexor tendon grafting. Indication for tenolysis includes a well-motivated patient with a supple digit and a wide discrepancy between active and passive ranges of finger motion. The procedure consists of meticulous division of all restraining adhesions of the flexor tendons and a careful preservation of annular pulleys. Active and passive movements with place-and-hold finger exercises are performed to gain maximum tendon gliding.
8.2.2.1 Neglected Flexor Tendon Injuries
Natural History
Most flexor digitorum profundus (FDP) tendon lacerations in zones 1 or 2 are now repaired primarily with excellent results. Although patients with uncomplicated FDP tendon injuries are easy to examine at initial presentation, they often present late to hand surgeons. This includes patients with missed or neglected injuries or those with associated medical conditions that have delayed surgical treatment. The athlete often comes in after the season with loss of flexion of distal interphalangeal (DIP) joint. Direct repair can be still performed after 3 weeks, when the short vinculum to the FDP has remained intact and maintained the proximal tendon stump in a distal location. Lacerations that have been neglected for over 3–6 weeks may have degenerative change of the tendon stump and the tendon sheath. Injuries resulting in segmental tendon loss are also impossible to repair.
Imaging
In most cases, the tendon stump is located distally. Though, this may be uncertain until surgical exploration. Ultrasound or magnetic resonance imaging (MRI) can be used to localize the tendon stump preoperatively. It is difficult to identify the proximal stumps of the tendon in the carpal tunnel on ultrasound.
Nonoperative Management
Delayed cases or segmental tendon loss cannot be adequately treated with primary repair. When primary repair is impossible, three alternatives are available: observation, DIP joint arthrodesis, or tendon reconstruction.
The late treatment of FDP laceration or rupture with a full functional flexor digitorum superficialis (FDS) tendon is controversial. Most of the useful motion is maintained when the FDS is functional. Many patients with a severed FDP and an intact FDS can do well in daily living and can be treated conservatively. This is particularly true when the DIP joint is not hyperextensible.
Surgical Management
When passive motion at the DIP joint has been maintained, the choice for surgical treatment includes DIP joint arthrodesis/tenodesis and free tendon graft. In my opinion, the tendon graft is better indicated in a high-level athlete who needs restoration of a mobile digit especially on the dominant hand. If the patient accepts the handicap and needs a faster return to competition, DIP fusion is considered.
Arthrodesis/Tenodesis
Severe phalangeal fractures or crushing injuries usually result in extensive scarring around the flexor tendon. Scarring around an area that received significant trauma may cause joint contracture. In this situation, tenodesis, or arthrodesis, may be preferred to free tendon grafting. If damage at the PIP joint results in a contracture, tenolysis and PIP joint release can be combined with a DIP joint fusion.
Tendon Grafting
Indication
The restoration of FDP function is a valuable procedure which improves grip. The procedure is probably more reasonable for power grip on the ulnar side of the hand (i.e., in the ring and little fingers) than on the radial side of the hand. Tendon grafting for the index and long fingers is indicated only when the patient requires the action because of a special interest or occupation, as in athletes [136].
Tendon grafting is more pertinent when the FDS is not pulling through completely and there is limited active PIP flexion.
It is necessary to discuss with the patient details of tendon grafting and its risk of compromising existing function (i.e., loss of proximal interphalangeal (PIP) motion). The surgeon must understand that while passing the tendon graft through or around the FDS, injury may occur that ultimately results in the formation of adhesions.
One-Stage or Two-Stage?
The precise indications for one-stage tendon grafting are controversial, though satisfactory results have been demonstrated with tendon grafts through an intact FDS with varying indications in carefully selected patients [136, 137, 138].
Indications for a one-stage grafting depend on several factors, including the age of the patient, the condition of the finger, functional status, the occupational of the patient, and the patient’s individual desires. Prerequisites include acceptable circulation, adequate passive movements of all joints, a well-healed wound without extensive scarring, and a neurovascularly intact digit with at least one digital nerve intact.
Two-stage reconstruction should be considered when intraoperative assessment demonstrates excessive scarring or an inadequate pulley system.
In these patients, the decision needs to be made whether to reconstruct the flexor tendons with one-stage grafting or not.
A temporary silicone spacer is needed to develop a smooth-gliding bed around the implant before placing a tendon graft. Two-stage grafting for severe injuries has been described in many other books; in this section, techniques for one-stage free tendon grafting in athletes are described.
Surgical Techniques
Before surgery, the wound should be well healed, and the joints should have intact maximum passive motion. Patients presenting with joint contracture should undergo a hand therapy protocol to regain as much passive digital motion as possible before tendon grafting.
The surgery should be carried out under tourniquet control. Midlateral or zigzag (Bruner) approach is used based on surgeon preference and/or on the presence of preexisting surgical or traumatic scar. I prefer a zigzag incision to expose the tendon system, although the midlateral approach has the advantages of placing the scar away from the area of grafting and of providing a healthy bed of subcutaneous tissue over the sheath and graft.
At operation, the injured tendons excised and replaced with a tendon graft secured to the base of the distal phalanx at the FDP insertion and joined to a proximal motor in the palm or distal forearm (Fig. 8.55). When the palm is relatively scar free, the graft may be placed from the palm to the fingertip. If the palm is also scarred, then the graft should be extended from the fingertip to the distal forearm. Care should be taken to ensure the preservation of as much of the healthy tendon sheath and pulley system as possible—at least the A2 and A4 pulleys. Surgical principles to be followed include placement of only one graft in one finger, never sacrificing an intact FDS, ensuring that the graft is of small caliber with its ends fixed away from the tendon sheath, and ensuring adequate graft tension.
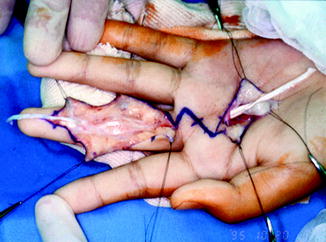
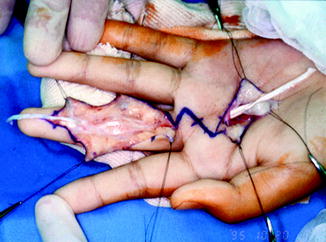
Fig. 8.55
Intraoperative findings of one-stage grafting. The palmar surface of the tendon sheath was identified through a zigzag skin incision, and the harvested plantaris tendon is interposed
The harvested tendon is anchored to the base of the distal phalanx. One centimeter of the FDP stump is preserved and reflected to its insertion in the distal phalanx. We prefer the “button-on-the-nail” technique using a stainless-steel wire suture drilled through the distal phalanx, but acknowledge risk of nail deformity, looseness, and infection. Distal fixation of the graft has involved a number of techniques over the years [139], although the use of bone anchors for distal attachment has been recently preferred. The surgeon should make an effort to minimize the dorsal cortical penetration by placing a finger over the proximal nail bed during the drilling process. This can produce a strong bone-tendon juncture with less damage to the distal phalangeal bone and fingernail bed than with the “button-on-the-nail” method.
Proximally, a Pulvertaft weave is used to complete the proximal juncture just distal to the insertion of the lumbricals [137]. When the distal suture is done first, the wound can be more easily closed in the extended position and the appropriate graft length determined in the palm. The FDP is used for the motor, unless it is of poor quality, in which case the FDS can be used. The appropriate tension is achieved by observation of the resting position of the finger during passive flexion and extension of the wrist. The finger tension is set a little tighter than the other fingers.
Tendon Selection for Grafting
Grafts must meet certain criteria, such as low donor site morbidity and sufficient length and diameter. The palmaris longus and plantaris tendons are commonly used owing to their small size, low donor site morbidity, and easy accessibility. Both tendons can be easily harvested with a tendon stripper.
Tendon grafts require considerable length, not only to bridge the gap but also to allow interweaving. The palmaris longus tendon averages 3 mm in width and 15 cm in length, which usually provides enough length for a single digit. The plantaris tendon is usually 12–18 cm in length. The plantaris provides a thinner graft than the palmaris longus and thus more rapidly revascularized. The palmaris longus is the first choice if a strong tendon is required, whereas the plantaris has the added benefit of additional length if needed.
The long toe extensor of the second and third toe is used if neither is available.
Extrasynovial tendon grafting is the most common technique used today. Failure of the graft due to formation of adhesions is decisive for the final result. There is recent biological evidence supporting the use of intrasynovial grafts. The toe flexors to the second through fifth toes are intrasynovial grafts and have the potential to heal with fewer adhesions. The toe flexors are less accessible compared to extrasynovial tendons. After the toe flexor is harvested, flexion of the toes is slightly limited. This is, perhaps, not suitable for an athlete, because of potential deficit in the foot.
Postoperative Care
Tendon Grafting
The surgeon and therapist must communicate regarding preoperative status, the condition of the tendon, and the status of the pulleys.
Traditional treatment involves 3 weeks of immobilization in which a posterior plaster splint is applied. The splint is replaced at 21 days, and an active exercise program is started. Full passive extension of the digit is not permitted for several additional weeks. It is our belief that postoperative immobilization after free tendon grafting may eventually lead to adhesion between the tendon and the surrounding tissues that compromise functional result.
The same early mobilization exercises developed after primary repairs are applied after free grafting. This program may help limit the formation of adhesions. We believe strongly in the importance of postoperative mobilization following free tendon grafting, although its role in this case is controversial. Some authors (Goldner and Coonrad [140]; McClinton et al. [141]; Pulvertaft [137]) prefer postoperative immobilization for 3 weeks. Tonkin et al. [142] reported on the results of one-stage tendon grafting in 49 patients who were managed postoperatively by either immobilization for 3 weeks or early controlled mobilization. They observed that postoperative management did not affect the final outcome.
Our preferred postoperative protocol is immediate early controlled mobilization with a modified Kleinert elastic band technique. Intensive physiotherapy with passive flexion and active extension of the IP joints started on the first postoperative day. A thermoplastic dorsal blocking splint with rubber bands is used to hold the wrist at 30° of flexion, the metacarpophalangeal (MCP) joint at 50° of flexion, and the PIP and DIP joints at full extension. Active extension to the limits of the splint is performed against the rubber band, and passive flexion is helped by the patient pushing down on the tips of the fingers. Positioning in constant flexion with a splint can lead flexion contracture of IP joint. The proximal phalanx is held in flexion by the therapist and the IP joint extended. The patients are made to perform three to six repetitions hourly for 2 and 3 weeks. The range of motion, frequency, and number of repetitions are increased according to the progress of the rehabilitation program. After several days, the patients are encouraged to do the “place-and-hold” technique once for each set. After 3 weeks, the dorsal splint is changed to a neutral wrist splint with the MCP, PIP, and DIP joints at nearly full extension to increase the excursion of the tendon (Fig. 8.56). At 6 weeks, the hand is protected by a dorsal splint only, and active flexion exercise is encouraged. Active finger use is permitted at 12 weeks postoperatively.


Fig. 8.56
Modification of the passive flexion splint with rubber bands. The dorsal splint is placed to a neutral wrist splint with the MCP, PIP, and DIP joints at nearly full extension to increase the excursion of the tendon
Joint contractures may occur early or late during rehabilitation. This complication can be treated with protected passive stretching and dynamic splinting techniques to achieve adequate motion. If this fails, surgical release can be performed.
Either excessively violent rehabilitation or poor surgical technique may result in breakdown at the proximal or distal juncture of the graft. If recognized early, the graft can be salvaged by treating the rupture like an acute flexor tendon injury.
Quadriga syndrome is one of complications of inadequate tensioning or adhesions limiting excursion. If surgical procedure prevents proximal excursion of the FDP, the adjacent fingers will lose some distal excursion as a result of sharing a common muscle belly when the repaired finger has reached maximal flexion. This also may occur either when one FDP is advanced too far distally in a reattachment procedure in zone I or when the tendon graft is too short. The treatment includes graft lengthening, tenolysis, or graft excision to allow the other normal adjacent fingers to flex fully.
When the graft is too long, lumbrical-plus finger may occur. The lumbrical origin is pulled proximally with proximal movement of the graft. Tension on the lumbrical muscle will paradoxically cause extension at the PIP joints. This complication can be treated with tenodesis of a half-slip of FDS tendon.
Outcomes and Return to Sport
Arthrodesis/Tenodesis
Most arthrodesis/tenodesis require protection with plastic splint during daily activity for at least 12 weeks. Protection during athletic activity should continue until the joint is fused. If fusion has been judged complete, the athlete resumes competition in a carefully molded splint or taping.
Tendon Graft
There have been only six recent studies describing the results of FDP reconstruction using one-stage tendon grafting (Table 8.9). Tonkin et al. [142] reported on both one-stage grafting and two-stage grafting in a number of cases with varying local tissue conditions and analyzed the factors that influenced the improvement of interphalangeal joint active motion. They concluded that the method of reconstruction, site of the proximal suture line, source of the tendon graft, interval between injury and reconstruction, length of follow-up, and postoperative management did not affect the surgical result. Fingers retaining an intact superficialis tendon achieved superior outcomes. Our long-term review [138] showed that all but one patient had good to excellent results according to the ASSH and Strickland criteria. One patient had growth arrest of the epiphyseal line at the distal phalanx at follow-up. Thus, we recommend bearing in mind that excessive dissection and formation of transosseous tunnels around growth plate may result in growth disturbances.
Table 8.9
Reports of one-stage flexor tendon grafting for neglected flexor digitorum profundus tendon injuries
Series | Total number of cases | Age at reconstruction (years) | Graft tendon | Interval between injury and reconstruction (months) | Postoperative rehabilitation | TAM (°) | Active DIP joint flexion (°) |
|---|---|---|---|---|---|---|---|
Goldner and Coonrad [140] | 18 | 5–40 | Plantaris | 9 (1–12) | Immobilization for 3 weeks | ND | 32 |
Bora [143] | 20 | 0.3–13 | 19 Plantaris, 1 PL | 12 (1.5–48) | Immobilization for 3 weeks | ND | ND |
McClinton et al. [141] | 100 | 1.5–60 | 80 PL, 18 extensor | Unknown | Immobilization for 3 weeks | ND | 48 |
Tonkin et al. [142] | 49 | 8–72 | ND | Unknown | Immobilization for 3 weeks, early controlled mobilization | 196 | ND |
Sakellarides and Papadopoulos [144] | 50 | 18–60 | 35 Plantaris, 15 PL | 1.5–72 | Immobilization for 3 weeks | ND | ND |
Liu and Yang [145] | 15 | 17.3 (13–21) | PL | 2.1 (0.5–3.5) | Immobilization for 1 week | 181 (145–230) | 33 (15–55) |
Yamazaki et al. [138] | 7 | 11 (7–15) | 6 Plantaris, 1 PL | 25 (3–78) | Early controlled mobilization | 237 (195–275) | 49 (20–80) |
Before the athlete returns to competition, progressive resistive should have started. Timing of resistive exercise is important. To avoid rerupture at insertion of the graft, the patient should be protected from further trauma until healing and remodeling of the tendon graft are completed. Heavy use or resistive exercises should not be permitted until 24 weeks from the surgery. Proper management can significantly reduce tendon rerupture.
Preferred Method of Treatment for Athletes
With appropriate surgical technique and the correct indications, one-stage grafting for neglected flexor tendon injuries can result in satisfactory result. It would seem reasonable to use the one-stage reconstruction in athletes with a finger in good condition.
8.2.2.2 Bridge Graft for Closed Flexor Tendon Ruptures
Natural History
Most flexor tendon ruptures result from avulsion of the FDP tendon at its insertion. Although not common compared to rheumatoid arthritis, closed flexor tendon ruptures caused by hidden pathologies of the carpal bones and joints have been reported, namely, fracture of the hook of the hamate, Kienböck’s disease, scaphoid nonunion, pisotriquetral osteoarthritis, pisotriquetral instability, lunate fracture, and chronic lunate dislocations. 12.8 % of flexor tendon ruptures had occurred in the carpal tunnel, and two of the ten had associated abnormalities of the carpal bones. Flexor pollicis longus (FPL) tendon and FDP tendon of the little finger were most frequently affected in ten patients with flexor tendon ruptures. Yamazaki et al. [146] reported 21 patients with closed rupture of the flexor tendons caused by carpal bone and joint disorders and described usefulness of radiocarpal arthrography as a diagnostic test.
Physical Findings
A detailed history and clinical examination allow diagnosis of flexor rupture. However, especially in chronic cases, diagnosis is often delayed or missed. In most patients, the closed flexor tendon rupture occurs when mild resistance forces are applied to the finger or spontaneously. In some cases, flexor tendon attritions and rupture cause discomfort within the region of the synovial sheath of the digit.
The mechanism of these tendon ruptures is attrition from passage back and forth over a rough bone surface, the latter having perforated the dorsal wall of the carpal canal. The tendon that ruptures depends on the location of the bone perforation into the carpal tunnel. The affected digit provides useful information about the location of the disorder. Disorders with an ulnar location in the carpal tunnel, such as the hook of the hamate and the pisotriquetral joint, contact and may abrade the FDP tendon of the little finger, particularly. The neighboring FDS tendon of the little finger and the FDP tendon of the ring finger may subsequently be affected. The FPL tendon lies over the ulnar surface of the scaphoid, and nonunion of the scaphoid may cause FPL tendon rupture. The lunate forms the dorsal wall of the carpal tunnel and contacts the FDP tendon of the index finger, the tendon located most dorsally in the carpal tunnel. Therefore, a lunate abnormality in which bone penetrates the volar capsule is most likely to cause attrition of flexor tendons of the index finger.
Imaging
Ultrasound, MRI [147, 148], and three-dimensional computed tomography (CT) imaging has been reported to be a useful tool for diagnosing flexor tendon injury and pinpointing the site of rupture, which is crucial for preoperative planning and thus avoiding unnecessary surgical exploration. In patients with flexor tendon rupture caused by carpal bone and joint disorders, detection of the underlying pathological lesion before surgery is also extremely important for the treatment, because surgical approach of the lesion is needed to prevent flexor tendon rerupture. To prevent recurrence, the sharp bone must be resected and the capsule/periosteum repaired. Nonunion and osteoarthritis with instability often require bone grafting. Plain X-ray of the wrist is often unhelpful, unless special views are taken. Radiography in a carpal tunnel view, radiography in an oblique lateral view in supination, conventional tomography, and CT imaging can help providing diagnosis of the pathologies. MRI is also useful. However, it is often difficult to differentiate the causative lesion of the tendon rupture from other abnormal lesions by these diagnostic imaging studies, especially in the elderly or in manual laborers who have preexisting abnormal lesions, including osteoarthritis, instability of the carpus, and radiographic evidence of previous trauma. Radiocarpal arthrography is very useful in identifying the site of the lesion responsible for the flexor tendon rupture [146]. Radiocarpal arthrography was performed in 13 patients in our series, and capsular perforation was demonstrated by contrast medium leakage into the carpal canal in 11 patients. A high percentage of cases in our investigation displayed contrast medium leakage (Fig. 8.57) that subsequently corresponded to the disruption of the periosteum or capsule at surgery. And the nearest tendons were ruptured. Generally, the lesion from which contrast medium leaks will identify the tear and, hence, the bony causes of the tendon rupture.


Fig. 8.57
Radiocarpal arthrogram showing leakage of contrast medium (arrow) into the flexor tendon sheath in pisotriquetral joint arthritis. The lesion from which contrast medium leaks will identify the bony cause of the tendon rupture
Nonoperative Management
There is no nonoperative treatment for this complication. If the pathological lesion is left unreconstructed, rupture of the neighboring tendon can occur.
Surgical Management
The goals of surgery are to reconstruct flexor tendon function and to prevent flexor tendon rerupture. The affected tendon(s) invariably have frayed stumps, with a long defect between the ends. Thus, tendon suture is impossible. The options of tendon reconstruction include DIP joint arthrodesis, tenodesis, cross transfer of flexor tendons from adjacent fingers, buddying to adjacent flexors, and free tendon graft.
The DIP joint can be fused later, or if the PIP joint is functional, the finger can be left alone. Many patients do well in daily living without a profundus tendon in the setting of a well-functioning FDS. Our preferred management is to bridge the graft, because independent motion of the DIP joint is reconstructed only by tendon grafting and bridge grafting in the palm has relatively good results compared to zone 2.
Tendon graft should be done early to prevent myostatic contracture in the affected digit. If the tendon rupture is neglected, myostatic contracture may result in incorrect tension of the tendon graft at surgery and reduced grip strength. During operation, a curved and zigzag incision is made on the palm between distal palmar crease and proximal crease. The patients underwent release of the carpal tunnel for exposure of the pathological lesion and the tendon stump. We used this method to check the neighboring tendon which is often frayed. The volar capsule/periosteum of the lesion is perforated at the site of the tendon rupture. The free/sharp bone fragment is excised. In tendon grafting, the palmaris longus tendon or the plantaris tendon is harvested. The proximal stump is pulled well until myostatic contracture is released. The remnant tendon is trimmed out, and the interpositional or transfer tendon is sutured to the refreshed stump with interlacing or Pulvertaft weave suture. The junction of the graft with the stump is placed away from the carpal area to prevent adhesion of the tendon stump within the carpal tunnel. Correct tension is achieved by observation of the resting position of the finger and the IP joint during passive flexion and extension of the wrist. One patient in whom the transverse carpal ligament was resutured developed carpal tunnel syndrome subsequent to surgery, and we now recommend that this is not done.
Postoperative Care
Postoperative management following free tendon grafting is important. This procedure incurs the risk of postoperative contracture in the interphalangeal joint. Postoperative immobilization after free tendon grafting may eventually lead to adhesions that compromise functional result. Early mobilization after FDP reconstruction may solve these problems because it provides gliding between the grafted tendon and the sheaths. The postoperative protocol in our preference is immediate early controlled mobilization with a modified Kleinert elastic band technique for 3–4 weeks. The Duran method is also performed to prevent contracture of IP joint. Thereafter, the hand is protected by a dorsal splint only, and active flexion exercise is encouraged. Active finger use is permitted at 12 weeks postoperatively. Dorsal blocking splint with rubber band is hardly used in the thumb.
Outcomes and Return to Sport
We reported the results in the finger after 13 free tendon graft reconstructions followed by early controlled mobilization; total active range of motion was averaged 213° [146]. Outcome, as measured by the American Society for Surgery of the Hand criteria, was excellent in 1 finger, good in 11, and fair in 5. The active range of motion of the thumb interphalangeal joint in three cases improved from 0° to 33° on average (range 10–40°). Outcome, as measured by Buck-Gramcko criteria, was good in two patients and fair in one. In our series, the mean patient age was 68 years. Although this was relatively high, results were satisfactory after tendon grafting, and outcome did not depend on patient age or on the interval between tendon rupture and reconstruction. The postoperative grip strength ratio averaged 84 % (range 57–126 %). Tendon reconstruction does not improve grip strength. This also may be because of the presence of an intact FDS tendon in the affected finger in our cases and/or the relatively small contribution of the one FDP tendon to entire grip strength.
Return to sports criteria is the same as that of tendon graft in neglected tendon injury.
Preferred Method of Treatment for Athletes
We believe that free tendon grafting is reasonable; while this technique has the risk of adhesion and rerupture, use of the tendon of another finger for transfer may compromise function of the other finger unnecessarily. Independent motion of the DIP joint is reconstructed only by tendon grafting. The postoperative management with early controlled mobilization is relatively effective.
8.2.2.3 Tenolysis for Flexor Tendon Adhesions
Natural History
The causes of restricted finger motion after extra-articular phalangeal fractures include flexor tendon adhesions, extensor tendon adhesions, joint contracture, skin contracture, malunion of the phalanges, and combinations of these factors. Flexor tendon adhesions tend to occur with fractures of the proximal and middle phalanges and are associated with fracture malalignment and displacement, fractures with palmar angulation, crush injury, and excessive prolonged immobilization. It has been suggested that even minor abrasions of the epitenon of the flexor tendons could become focal points for adhesions at a fracture site. Exostosis formation interferes with excursion of the overlying flexor tendon. The adhesions were widespread and not only adjacent to the fracture. The tendon adhesions were not only between the tendons and the bony floor of the flexor sheath but also between the tendons and the sheath [149]. The location and density of the adhesions were very variable and unrelated to the fracture type, the immobilization period or the interval between fracture and tenolysis. Their presence beyond the site of fracture is probably due in part to fibrin formation in the edema which inevitably follows the primary injury and also due to bleeding within the flexor sheath after the injury. Immobilization for several weeks after injury also allows the adhesions to mature such that many hand surgeons worldwide now advocate mobilization of phalangeal fractures, after a variety of stabilization activities, within 24–48 h.
Adhesions are the most common of complications after failed primary tendon repairs, crush injuries, infections, and flexor tendon grafting. An adequate therapy program should be used to limit the formation of adhesions and can mobilize through some adhesions.
Nonoperative Management
If the adhesions are not serious, a conscientious therapy may restore full function. Nonoperative restoration of flexor tendon performance in severely damaged fingers is difficult. Once a patient’s progress has plateaued and a significant difference between passive and active range of digital motion exists and satisfactory function cannot be restored, then a tenolysis may be considered.
Surgical Management
Flexor tendon tenolysis for the treatment of adhesions is thought to be successful after phalangeal fracture [150]. Once surgical release has been successfully accomplished, full range of motion is usually regained. Surgical release of restrictive adhesions has been considered as the potential final salvage procedure following tendon repair, conventional grafting, or staged reconstruction, when tendon and pulley integrity are maintained and the involved joints are supple. The best candidate for tenolysis is a patient whose repaired tendon has localized adhesions that limit gliding. When there has been no significant improvement for several months despite a conscientious therapy program, the decision to perform the procedure should be considered.
If the procedure is unsuccessful, the patient’s hand function may be even worse than before surgery. The patient must be informed that if the findings at surgery show an excessive scarring or poor tendon integrity, it may be necessary to change to the implantation of a silicone tendon implant as the first step of two-stage grafting.
The appropriate timing for tenolysis for tendon adhesion is controversial. Waiting 3 months following primary repairing and 6 months following grafting before performing tenolysis has been recommended. The fractures should be healed, and wounds must have minimal reaction around scars. Joint contractures must have been mobilized and a near normal passive range of digital motion achieved. Every effort should be made to achieve full passive digital joint motion before surgery, because the concomitant tenolysis and joint release are prejudicial to the final result.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree