Fig. 10.1
Hematoma due to a tourniquet applied too tightly
10.3.2 Iatrogenic Nerve Injuries
These may be related to locoregional anesthesia technique (see Chap. 6.4) or directly to the surgery [18]. The literature most often reports extreme cases (i.e., excising a nerve instead of a tendon [19]). However, arthroscopic maneuvers on the proximal interphalangeal (IP) joints or on the wrist are at high risk of nerve injury [20, 21]. Only experience, anatomical knowledge, and care can prevent these complications.
10.3.3 Lymphedema After Axillary Lymphadenectomy
10.3.4 Iatrogenic Arterial Lesions
The true incidence of these lesions is impossible to assess because – thanks to the presence of double vascular axes – they have almost no effect. They can be detected only during surgery, although this is rare because of the use of a tourniquet. They usually occur during the installation of the material. Prevention is by experience, anatomical knowledge, and careful and rigorous technique [26, 27].
10.3.5 Tendon Injuries
These include tenosynovitis or tendon rupture and can occur in 7 % of osteosyntheses, especially of the wrist. They are usually due to conflict with the material [26, 28]. Prevention requires experience and a rigorous osteosynthesis technique. The need to remove the material will be assessed by the surgeon. If the risk of tendon abrasion is important due to protruding pins or a cumbersome plate, material removal should be proposed. However, compact and low profile material, such as screws, can be left in place. The athlete is no exception to these rules, and material removal should be proposed based on these criteria.
10.3.6 Delay of Consolidation and Nonunion, Malunion, Stiffness, and Arthritis
These complications are discussed in specific chapters.
10.3.7 Fracture and Loosening of the Material
These complications may occur in up to 8 % of osteosyntheses (Fig. 10.2). They are promoted by early and poorly controlled mobilization. However, they do not necessarily result in failure or nonunion if detected early and the mobilization is modified [29].


Fig. 10.2
Loosening of a plate for a metacarpal fracture. The criteria of osteosynthesis have not been met with an intrafractural screw, and there is an insufficient number of distal screws
10.3.8 Bone Graft Complications
According to a recent meta-analysis, these complications can affect up to 19 % of grafts [30]. They include nerve damage, hematoma, fracture, and infection of the donor site. The most common complication is pain [31]. Different harvesting sites have their peculiarities: for moderate amounts of grafts, the distal radius and the olecranon are useful at the cost of a risk of fracture with mechanical consequences (Fig. 10.3). The iliac crest allows for harvesting larger amounts of grafts without functional consequences in case of fracture but should be performed under general anesthesia.
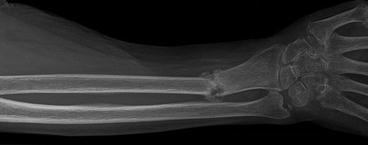
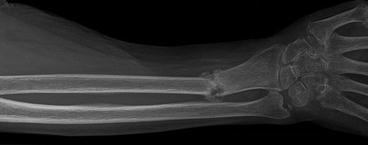
Fig. 10.3
Fracture of the lower fourth of the radius after bone harvesting for transplantation (proximal IP arthrodesis)
10.3.9 Complex Regional Pain Syndrome
The name of this disease is, in itself, subject to debate: algodystrophy, Sudeck’s syndrome, reflex sympathetic dystrophy, shoulder-hand syndrome, etc. It is a general complication of trauma, and is not related to the treatment, whether surgical or not. There are many different symptoms that can occur concurrently, to variable degrees: pain, significant edema greatly exceeding the traumatized area, erythrosis, hyperhidrosis, and stiffness. The diagnosis is mainly clinical, and the use of scintigraphy is not systematic. The treatment proposals are as varied as they are controversial. However, there are validated, preventive measures:
Locoregional anesthesia.
Good-quality perioperative analgesia.
Administration of 500 mg of vitamin C for 50 days; this treatment decreases the frequency of disorders from 10.1 to 2.4 % in the aftermath of wrist fractures [32].
Only a few curative treatments seem to be validated in the literature:
Corticotherapy
Rehabilitation
Pain management, specifically neuropathic pain
Sympathoplegic blocks [33]
In any case, this condition is problematic, both in its understanding and in its treatment, and treatment by a specialized team should be the rule whenever possible.
10.3.10 Complications of Bandaging (Tight Dressings)
This can cause swelling, pain, or ischemia and nerve damage. The signs are pain, a sensation of constriction, venous stasis with a bluish appearance of the skin (sometimes difficult to differentiate from a hematoma), paresthesias, or an ischemic appearance distal to the dressing. In case of doubt, redressing should be proposed. The dressing should meet the usual rules: comfort, cleanliness, and flexibility. Its renewal remains at the discretion of the practitioner.
10.3.11 Complications of Immobilization
Cast compression (Fig. 10.4) is a devastating complication, with a poorly assessed frequency. It can progress into a Volkmann syndrome, a neurological compression or pressure sores. These complications can be prevented by rigorous technique and regular monitoring, particularly to assess severe pain and dysesthesia [34]. The monitoring instructions must be given to the patient. The type of trauma (crushing, high energy) must be considered in the risk-benefit analysis.


Fig. 10.4
Cast compression. This type of lesion should not occur anymore
10.3.12 Complications of Local Anesthetics
The hand surgeon must often administer local anesthesia, and this implies low but non-negligible risks:
1.
Local nerve toxicity in cases of endonervous infiltration (especially with lidocaine).
2.
General toxicity, either by accidental injection into a blood vessel or by excess dose. Toxicity is related to the membrane stabilizing action and is twofold: first, neurocentral and, at higher concentrations, cardiac (arrhythmia, tachy-/bradycardia, cardiac arrest).
3.
Allergy: This complication is very unusual and consists of cross-allergies between some conservatives of epinephrine solutions and the para-amino benzoic acid of the local anesthetics of the amino ester group.
4.
Effect of the adjuvants mainly related to adrenaline and its vasoconstriction characteristics.
5.
Methemoglobinemia.
10.3.12.1 Are Complications in Hand Surgery More or Less Frequent Than in Other Specialties?
It is possible to divide the complications into two groups according to their compared frequencies:
Infection, nonunion (other than carpal scaphoid), and hematoma are usually rarer in hand surgery.
Stiffness, tendon complications, and reflex sympathetic dystrophy are usually more common in hand surgery.
10.3.12.2 Do High-Level Athletes Have an Increased Risk of Complications?
High-level athletes are not more prone to complications, and their prognosis is rather favorable in complications that are effectively resolved by rehabilitation, which are the most frequent. However, the high level of functional performance demanded can be a source of disappointment because minimal sequelae can have little impact on daily life but a high impact in a competitive environment.
10.4 Consent
Informed consent is now a legal requirement and a necessity in the surgeon-patient relationship, especially in a specialty such as hand surgery with such a high functional risk. This consent requires a detailed and fair explanation of the benefits and potential risks of the surgery and allows the patient to participate in the treatment decision. It leads to the patient signing a consent document (Box 10.2).









