6
Pyogenic Arthritis
Kevin D. Plancher
History and Clinical Presentation
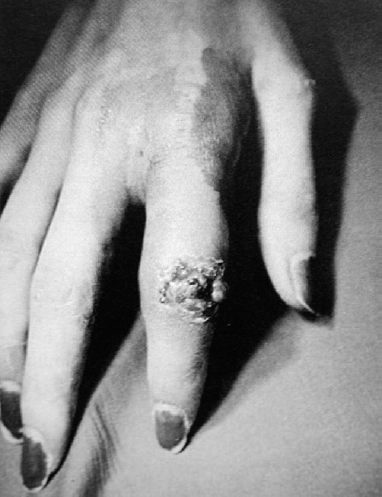
A 35-year-old, right hand dominant woman presented with a swollen right index finger. She reported previously having a large piece of wood that entered her finger near the metacarpophalangeal (MP) joint, but stated that she had removed the wood. A puncture wound was present over the joint and she has had progressive tenderness of the finger and increased pain with activity. Her wound has now dramatically changed after spending the weekend working in the garden.
Physical Examination
Examination reveals a warm finger with a joint effusion and surrounding soft tissue edema at the proximal interphalangeal (PF) joint of the index finger. Active and passive joint range of motion is painful. The painful joint with no evidence of cellulitis was aspirated through skin that was sterilized. The fluid obtained was turbid.
Differential Diagnosis
Gout
Psoriatic arthritis flare
Systemic lupus erythematosus
PEARLS
- Diagnosis can be confirmed on aspiration.
- Early intervention avoids cartilage damage in a joint.
- Always send aspiration to the lab for cell count.
PITFALLS
- Assume that joint swelling will resolve with elevation and conservative treatment (antibiotics)
- Avoid a small incision under local anesthesia rather than wide debridement and irrigation in an operating room under regional anesthesia.
- Never assume the type of infection until the labs and culture and sensitivities dictate the correct antibiotic treatment.
Diagnostic Studies
Synovial fluid analysis includes Gram stain, cultures, and sensitivity testing. In septic arthritis, the joint fluid contains a white blood cell count over 50,000/mm3. The polymorphonuclear count should be over 75% and the synovial fluid glucose is 40 mg or lower.
Radiographs are taken to rule out an occult fracture and to assess the joint space for loose or foreign bodies. When treatment is been delayed, radiographs can be useful to determine the extent of articular cartilage destruction and bone loss.
Diagnosis
Pyogenic Arthritis Index Finger
Based on the clinical exam and the laboratory values of the synovial fluid, Gram stains, and cultures, the diagnosis of pyogenic arthritis was ruled in as the diagnosis. The most common organism isolated from septic hand joints is Staphylococcus aureus. Contamination of the joint can occur by several mechanisms including hematogenous or contiguous spread and postoperative infectious. Direct implantation of organisms can also occur from a hand injury during a brawl, or penetration from a nail, knife, etc. High suspicion for joint infection is important when the MP joints are involved. This is the case because these joints are the major target sites for lacerations secondary to coming in contact with human teeth during fistfights.
Nonsurgical Treatment
Because septic arthritis can cause articular cartilage destruction and osteomyelitis, aggressive surgical treatment is recommended. Nonsurgical treatment is not recommended for any open joint laceration that is suspected to have occurred from a bite or contact with a contaminated object.
Surgical Treatment
Once the diagnosis has been made (Fig. 6–1), the patient should be started on appropriate antibiotic (Table 6–1) and proceed with aggressive treatment of incision and drainage of the joint. This aggressive treatment is important to minimize the cartilage destruction and osteomyelitis.