Proximal Osteotomies of the First Metatarsal
Robb A. Mothershed
An increase of the first intermetatarsal angle, or metatarsus primus adductus, has long been recognized as a major contributing factor in the deformity of hallux abducto valgus.
This component of hallux abducto valgus has been addressed by proximal osteotomies for decades. A transverse plane osteotomy of the first metatarsal base for the repair of hallux abducto valgus deformity was first described in 1901 by Loison (1), and it was performed in 1903 by Balacescu (2). After a number of modifications, the procedure became more favorable in the late 1960s and early 1970s. The procedure began to lose its popularity over the last 15 years because of certain complications that were believed to be inherent to the procedure, including first metatarsal elevatus, shortening of the metatarsal, failure of the fixation, and delayed union. Subsequently, surgeons began to appreciate that most of these deficiencies resulted from surgical technique, inadequate fixation, and an insufficient period of non-weightbearing postoperatively. The perceived complications associated with the closing base wedge osteotomy also led surgeons to consider other forms of proximal osteotomies such as the crescentic and chevron. The favorability of the crescentic and chevron osteotomies has been replaced by the opening wedge osteotomy because of the advancement of fixation devices. Other surgeons have expanded the limitations of more distal procedures such as the Austin osteotomy because the distal procedures are technically easier to perform and the patient can remain weightbearing during the postoperative period. However, the proximal osteotomies still are effective, particularly in patients with severe deformities and in patients with high intermetatarsal angles. The technical advances in surgical technique, rigid internal fixation, and the institution of a non-weight-bearing interval in the postoperative recovery have demonstrated that these procedures can provide consistently good results.
INDICATIONS
In the past, the only indication for a base osteotomy was a severe hallux valgus deformity with a high intermetatarsal angle. The indications for a base osteotomy have been expanded as the procedure has been more critically evaluated. When evaluating a patient with a hallux abducto valgus deformity, there are other factors to consider, such as the flexibility of the deformity, the sagittal plane position of the metatarsal, the age of the patient, the presence of associated deformities, and whether there has been previous surgery to the first metatarsal. All of these factors are extremely important to consider when evaluating the patient with a hallux abducto valgus deformity to achieve the most successful result. The proximal osteotomy of the first metatarsal is a procedure that is indicated far more often than it is performed.
HIGH INTERMETATARSAL ANGLE
The primary indication for a base osteotomy has classically been an intermetatarsal angle greater than 15 degrees. A deformity of this magnitude is more difficult to correct with a distal osteotomy because it is approaching the upper limits for the amount of possible correction with the procedure. The proximal osteotomy is more effective in correcting a deformity with a high intermetatarsal angle than a distal osteotomy because of the mechanical principles of the placement of the osteotomy. The design of a proximal osteotomy of the first metatarsal allows for a greater degree of correction of the deformity with the apex of the osteotomy in close proximity to the base of the metatarsal. The greater distance between the apex and the distal portion of the metatarsal creates a greater lateral movement of the head of the metatarsal. The parallel relationship that is created with the second metatarsal prevents the creation of a negative intermetatarsal angle in the distal segment of the bone. The performance of a proximal osteotomy in a patient with a high intermetatarsal angle produces a more rectus appearance to the foot that maintains correction of the deformity for longer periods of time than a distal osteotomy.
RIGID FIRST RAY
The flexibility of the first ray is an important factor to consider when evaluating the hallux abducto valgus deformity. If the deformity has a rigid component and the intermetatarsal angle is moderately high, then this would be a strong indication for a proximal osteotomy. A rigid deformity is more resistant to a distal osteotomy because the soft tissues cannot be relied on to help maintain correction of the deformity as in a flexible deformity. Another good indicator preoperatively of a rigid deformity is the amount of space between the first and second metatarsal bases on an anterior-posterior (AP) radiograph of the foot. If the metatarsal bases are more closely approximated, then the deformity is more likely to be rigid. There is a high probability that the hallux abducto valgus deformity will recur if a distal osteotomy is performed in a rigid deformity with a moderate intermetatarsal angle. A proximal osteotomy of the first metatarsal is more effective in correcting a deformity of this type with less chance of recurrence.
ELEVATED FIRST METATARSAL
An equally important factor to consider when evaluating a hallux abducto valgus deformity is the sagittal plane position of the first ray. The sagittal plane position of the first metatarsal can be evaluated clinically by comparing the plantar level of
the first metatarsal to the second. Another good indication of an elevated first metatarsal is the presence of a callous plantar to the second metatarsal head or pain beneath the second metatarsal head. A lateral weight-bearing radiograph can also provide information of the sagittal plane position of the first metatarsal. An elevated first metatarsal can be more appropriately addressed at the base of the metatarsal. A greater degree of plantarflexion can be achieved with a proximal osteotomy of the first metatarsal because a small amount of plantarflexion at the base translates into a larger amount at the head of the metatarsal. If a similar amount of plantarflexion could be achieved with a distal metatarsal osteotomy, it would more abruptly change the vectors of the flexor and extensor tendons crossing the joint. This change in vectors would have a greater disruption of the muscular balance of the first metatarsal phalangeal joint. An abnormal sagittal plane position of the first metatarsal can be more effectively corrected with a proximal osteotomy of the first metatarsal base.
the first metatarsal to the second. Another good indication of an elevated first metatarsal is the presence of a callous plantar to the second metatarsal head or pain beneath the second metatarsal head. A lateral weight-bearing radiograph can also provide information of the sagittal plane position of the first metatarsal. An elevated first metatarsal can be more appropriately addressed at the base of the metatarsal. A greater degree of plantarflexion can be achieved with a proximal osteotomy of the first metatarsal because a small amount of plantarflexion at the base translates into a larger amount at the head of the metatarsal. If a similar amount of plantarflexion could be achieved with a distal metatarsal osteotomy, it would more abruptly change the vectors of the flexor and extensor tendons crossing the joint. This change in vectors would have a greater disruption of the muscular balance of the first metatarsal phalangeal joint. An abnormal sagittal plane position of the first metatarsal can be more effectively corrected with a proximal osteotomy of the first metatarsal base.
JUVENILE HALLUX ABDUCTO VALGUS
The development of hallux abducto valgus deformity in young patients represents significant deforming forces acting on the foot. The juvenile hallux abducto valgus commonly has a larger intermetatarsal angle and a smaller medial eminence than that found in the adult deformity. The juvenile hallux abducto valgus has a high association with other deformities and if present they must be addressed. Banks et al (3) found that 66.7% of the cases reviewed with juvenile hallux abducto valgus had a metatarsus adductus angle greater than 15 degrees. The presence of pes planovalgus and equinus has long been associated with juvenile hallux abducto valgus deformities. In the juvenile patient, the correction of the hallux abducto valgus deformity must be maintained over decades. Many studies have shown that there is a higher incidence of recurrence of the deformity in the juvenile patients who undergo a distal soft tissue procedure or distal osteotomy. The primary reasons cited for reoccurrence of the juvenile deformity was inadequate correction of the intermetatarsal angle with a simple bunionectomy at the time of the initial surgery (4,5 and 6). It is because of this greater deforming force that a proximal osteotomy must be performed to restore normal muscle function about the first metatarsal. The intermetatarsal angle in the juvenile patients must be reduced to zero or a slightly negative value to minimize the possibility of recurrence. If other deformities such as pes planovalgus, metatarsus adductus, or equinus are present, then they must be addressed at the time of surgery to ensure a successful result. The most effective correction of a juvenile hallux abducto valgus deformity is addressed with a proximal osteotomy of the first metatarsal.
HALLUX ABDUCTO VALGUS WITH METATARSUS ADDUCTUS
A hallux abducto valgus deformity in the presence of metatarsus adductus requires special consideration. The metatarsus adductus foot functions as if the intermetatarsal angle is significantly larger than it appears at first glance. The amount of metatarsus adductus correlates directly to the severity of the deformity. Banks et al (3) reviewed 72 cases and found 48 had a metatarsus adductus angle greater than 15 degrees. Other studies have discussed a statistically significant and direct relationship between patients with an increasing metatarsus adductus angle and an increasing hallux abductus angle (7,8). The initial radiographic evaluation of hallux abducto valgus with metatarsus adductus is often misleading because a large hallux valgus deformity is present with little intermetatarsal splaying. The true intermetatarsal angle can be estimated by the following formula: The true intermetatarsal angle is equivalent to the metatarsus adductus angle minus 15 degrees plus the intermetatarsal angle.
This formula will provide a better determination of the magnitude of the hallux abducto valgus deformity present. It is imperative in the patient with a metatarsus adductus and hallux abducto valgus deformities to reduce the intermetatarsal angle to zero or a slight negative value to minimize the chance of recurrence. If a distal osteotomy is performed in a patient with metatarsus adductus, there is a high probability that the hallux abducto valgus deformity will recur. The presence of metatarsus adductus and hallux abducto valgus often constitutes a severe deformity that can be more effectively corrected with an osteotomy at the base of the metatarsal.
IATROGENIC DEFORMITIES
The patient who has had previous hallux valgus surgery often presents with a difficult challenge. In many of these cases, there has been an overzealous resection of the medial eminence, which leaves little opportunity for a distal metatarsal osteotomy. A second problem arises when an underlying structural deformity is present that was not initially addressed. In any case that there has been previous surgery, the integrity of the bone of the first metatarsal head must be considered. The presence of previous fixation devices can disrupt the integrity of the bone stock, especially if there are multiple or large devices. An osteotomy through a suspect metatarsal head may lead to complications. An osteotomy through the same site can be avoided with a proximal osteotomy as well as correct for any previously unrecognized sagittal plane deformity. In the recurrent hallux valgus deformity, the most effective and reliable correction is with a proximal osteotomy of the first metatarsal.
CONTRAINDICATIONS
An osteotomy of the first metatarsal base should be limited in certain patient populations, especially in those patients who appear to be noncompliant. Osteotomies should be avoided in patients who are unable to remain non-weight-bearing until the osteotomy has healed. Frequent or early weight-bearing in the postoperative period may lead to a delayed union, nonunion, or malunion of the osteotomy. These undesirable results can lead to complications, such as lesser metatarsalgia, lesser metatarsal stress fractures, or chronic foot pain. Less than favorable results may require additional surgery and a more prolonged recovery to correct the complication.
The presence of a shortened first metatarsal should be carefully evaluated before considering a first metatarsal osteotomy. Traditional proximal osteotomies of the first metatarsal such as closing base wedge, crescentic, and chevron have limited applications because of the further shortening of the metatarsal than can occur following the procedure. An opening wedge osteotomy of the first metatarsal base is indicated in those patients with a greater degree of metatarsal shortening, in order to maintain the current length or in some cases to provide a small degree of lengthening. The advancement in rigid
internal fixation devices in the last few years has significantly enhanced the stability and performance of an opening wedge osteotomy of the first metatarsal base.
internal fixation devices in the last few years has significantly enhanced the stability and performance of an opening wedge osteotomy of the first metatarsal base.
ANATOMIC CONSIDERATIONS
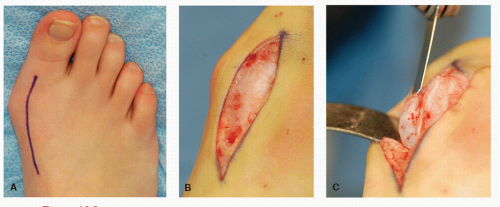
The most effective incision is placed from the first metatarsal-cuneiform joint to the proximal phalanx of the hallux. The initial incision is placed at the level of the first metatarsophalangeal joint (MTPJ) and then extended proximally to the first metatarsal-cuneiform joint, after the first MTPJ is released and the medial eminence excised (Fig. 28.1). The single incision approach has been performed for decades without any sequalae. After completion of the proximal portion of the incision, dissection is carried through the relatively thin subcutaneous tissues. The previously defined tissue planes at the first MTPJ may be followed into the proximal portion of the first metatarsal. Often times a branch of the medial dorsal cutaneous nerve is identified at the proximal aspect of the incision.
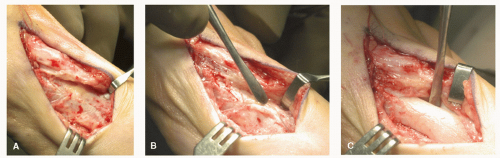
The nerve branch can easily be retracted into the medial subcutaneous tissues. After clearance of the superficial fascia from the deeper structures, the deep fascia can be incised medial to the extensor hallucis longus tendon, being careful to maintain enough of a margin for closure of the fascia. Once the deep fascia is reflected, the extensor hallucis longus tendon can be retracted laterally, allowing for better exposure of the periosteum over the base and shaft of the metatarsal. The periosteum is incised from the proximal and medial extent of the first metatarsal base and is extended laterally and dorsally on the first metatarsal shaft and then medially and distally toward the previous periosteal incision at the first metatarsal head (Fig. 28.2A). The periosteum is reflected from the first metatarsal with a Freer elevator, allowing exposure of the medial and lateral aspects of the metatarsal base (Fig. 28.2B and C). It is important not to free the periosteum from the area adjacent to the proposed apex of the osteotomy; otherwise, the stability of the osteotomy may be compromised. The periosteum should be handled with care and reapproximated at closure, because it does provide blood supply to the healing osteotomy. The
anatomical layers are reapproximated in a stepwise fashion at the completion of the procedure. Good anatomical dissection is essential to facilitate closure of the tissue planes.
anatomical layers are reapproximated in a stepwise fashion at the completion of the procedure. Good anatomical dissection is essential to facilitate closure of the tissue planes.
TECHNIQUES
CLOSING BASE WEDGE OSTEOTOMY
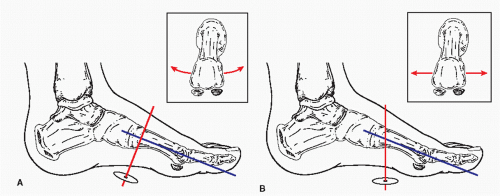
The modern version of the oblique osteotomy of the first metatarsal base was created at the Podiatry Institute in 1977 (9). The osteotomy can better accommodate the use of two points of fixation and it allows the surgeon to place the apex of the osteotomy more proximally, thus providing a longer radius arm for correction. The use of an axis guide can facilitate the performance of the osteotomy. The axis guide provides an accurate means of assessing and implementing concomitant dorsiflexion or plantarflexion of the distal portion of the metatarsal with closure of the osteotomy. It is important to understand the hinge-axis concept when performing the osteotomy to facilitate its performance. An intact cortical hinge can act as an axis of rotation for the base wedge osteotomy. The traditionally perceived axis for a hinged osteotomy of the first metatarsal was perpendicular to the long axis of the bone (Fig. 28.3A). As a result of the anatomic declination of the first metatarsal in the human foot, rotation of the distal segment of the first metatarsal around this axis after a closing base wedge osteotomy would tend to create elevation of the metatarsal head from the weightbearing surface. If the osteotomy is designed so the axis is perpendicular to the weight-bearing surface, then full rotation of the distal segment of the metatarsal can occur without elevating or plantarflexing the metatarsal head in relation to the weightbearing plane (Fig. 28.3B).
The sagittal plane orientation of the axis must be maintained to prevent elevation of the metatarsal head; however, the frontal plane orientation can be manipulated to influence the ultimate position of the metatarsal head in the weight-bearing plane. Manipulation of the axis in the frontal plane is based on the presumption that the axis remains perpendicular to the weight-bearing surface in the sagittal plane (Fig. 28.4A).
If the axis is maintained perpendicular to the weight-bearing surface in the frontal plane, then the lateral rotation of the distal metatarsal segment maintains the metatarsal head on the weight-bearing surface. The manipulation of the superior pole of the axis laterally creates a dorsomedial hinge, and plantarflexion of the distal segment of the metatarsal occurs with lateral rotation or closing of the base wedge osteotomy (Fig. 28.4B). Conversely, when the superior pole of the axis is tilted medially, a plantar medial hinge is created, and dorsiflexion of the distal segment occurs with closing of the base wedge osteotomy (Fig. 28.4C). In the patient with normal alignment and length of the metatarsal, it is important to plantarflex the distal segment to offset the degree of shortening and subsequent elevation of the metatarsal, which could occur with straight translocation of the metatarsal.
The hinge-axis concept is essential to the execution of the proximal closing wedge osteotomy of the first metatarsal. The width of the first metatarsal determines whether a 0.035- or 0.045-inch Kirschner wire (K-wire) is used as an axis guide and is drilled through the base of the first metatarsal to represent the proposed hinge site of the osteotomy. The K-wire should be inserted dorsally and medially in the metatarsal just distal to the intended apex of the osteotomy to allow reciprocal planing of the osteotomy. The surgeon must be mindful of the growth plate in juvenile patients. The wire is then drilled into the metatarsal perpendicular to the weight-bearing surface at the appropriate angle in the frontal plane to effect the desired manipulation of the distal aspect of the metatarsal that is necessary for each individual patient (Fig. 28.5A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree