13
Pronator Syndrome
Kevin D. Plancher
History and Clinical Presentation
A 35-year-old woman presents to our office with symptoms of forearm discomfort consisting of fatigue-like pain and numbness in her hand. She works long hours on a computer and reports that this repetitive activity is what reproduces the symptoms in her right arm; however, she denies any symptoms at night. The condition has been gradually getting worse.
Physical Examination
The patient presents with symptoms of general forearm pain in addition to paresthesias and hypersthesia in the thumb, index finger, long finger, and radial half of the ring finger. There is pain on flexion of the long finger at the proximal interphalangeal (PIP) joint. Sensory symptoms are also present over the thenar eminence in the distribution of the palmar cutaneous nerve.
Patient experiences pain on palpation of the median nerve in the proximal forearm. In addition, the pronator teres muscle can be tender, firm, or enlarged. Tinel’s sign is present on the nerve site just distal to the elbow and paresthesias increase with mild compression of the proximal muscle mass of the pronator teres. Phalen’s test is negative.
Diagnostic Studies
Electrodiagnostic tests are suggestive, but not always diagnostic. Although slowing will often show in the forearm, it does not always show in the carpal canal. The threshold testing with Semmes-Weinstein monofilaments may reveal decreased sensibility over the distribution of the median nerve.
Needle electromyography (EMG) may be useful if fibrillations, positive sharp waves, and reduced interference patterns are noted in the pronator quadratus and flexor pollicis longus (FPL). It is important to note that the EMG does not differentiate median nerve lesions at the pronator teres from those more proximal.
PEARLS
- EMG slowing in the forearm, not in the carpal tunnel
- Tinel’s sign in the proximal forearm
- Pain on long finger flexor digitorum superficialis (FDS) flexion
- Negative Phalen’s test
- No nocturnal symptoms
- Numbness of the palmar cutaneous branch of the median nerve
- Pain on resistance to pronation
PITFALLS
- Numbness of the radial 3½ digits.
- Full knowledge of the anatomy to avoid a complication on exploration is essential.
Differential Diagnosis
Carpal tunnel syndrome
Compartment syndrome
Pronator syndrome
Diagnosis
Pronator Syndrome of the Right Arm
Pronator syndrome is defined by functional problems of the median nerve due to some mechanical abnormality at the level of the forearm. This disturbance in function is often related to the path of the nerve through the middle of the pronator teres muscle. A concise and clear physical exam is the best indicator for diagnosis of pronator syndrome, which is similar to carpal tunnel, but less common. Both syndromes involve the median nerve and therefore have similar symptoms; the syndromes are usually differentiated based on the physical exam. Keys to the physical exam are to note the areas of tenderness and the presence of a positive Tinel’s sign. It is possible that both conditions coexist with medial nerve entrapment at the proximal forearm and the wrist. Correlating the physical exam with the EMG study aids in correctly diagnosing the patient’s symptoms. No motor symptoms or weakness is present with a pronator syndrome.
Surgical Management
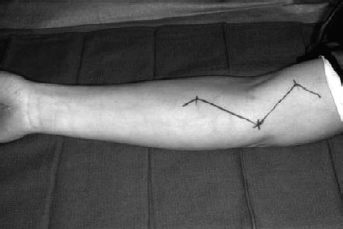
The initial incision usually begins 5 cm proximal to the elbow flexion crease unless either a supracondyloid process or accessory bicipital aponeurosis has been identified. If this is the case, the incision should begin no less than 10 cm proximal to the crease (Fig. 13–1).
The incision curves distally just medial to the biceps tendon, zigzags across the antecubital crease, and curves back medially for 5 cm in the proximal forearm.
Next, the medial antebrachial cutaneous nerve is identified and isolated as it continues along the basilic vein. The median nerve is then identified and isolated in a similar manner.
If a supracondyloid process or accessory bicipital aponeurosis had been identified preoperatively, the median nerve is identified and isolated in the most proximal portion of the incision and then traced distally. The supracondyloid process or accessory bicipital aponeurosis is then dealt with if present. It is important to explore the median nerve completely, as other, more proximal, sites of compression may exist at the same time.
The median nerve is then dissected distally. The bicipital aponeurosis is incised and the nerve followed to the proximal end of the superficial or humeral head of the pronator teres. Retraction of the head is needed to identify any variation in the nerve’s path in relation to the two pronator heads. Any tendinous or fibrous bands within the pronator are identified and incised (Fig. 13–2).
In those cases where the median artery penetrates the median nerve, interfascicular dissection may be used to enlarge the passage. Great care should be taken to avoid ligation of the artery. It is the dominant blood supplier to the median nerve 30% of the time and also significantly serves the index and long fingers in some cases.