46 Primary bone tumors are those originating in bone (rather than metastasizing to bone). The treatment of benign and malignant primary spinal column tumors is diverse and complex. Most of these tumors present as a solitary lesion. The age, site, clinical presentation, and cell type must be considered prior to initiating treatment. There are benign and malignant primary bone tumors. The neoplastic tissue is usually of mesodermal (bone, cartilage, fibrous, vessels, notochord) origin (Table 46.1). Table 46.1 Classification of Benign and Malignant Primary Bone Tumors
Primary Spinal Tumors
![]() Classification
Classification
Tissue of origin | Benign tumor | Malignant tumor |
Fibrous | Fibrous dysplasia | Malignant fibrous histiocytoma |
Cartilage | Osteochondroma | Chondrosarcoma |
Bone | Osteoid osteoma | Osteosarcoma |
Hematopoietic | Plasmacytoma | |
Vascular | Hemangioma | |
Notochord | Ecchordosis | Chordoma |
Unknown | Giant cell tumor | Ewing sarcoma |
 Workup
Workup
History
The clinical presentation of primary bone tumors varies. A thorough history and physical examination will help direct the most appropriate care. Signs and symptoms of the tumor include persistent back pain, difficulty maintaining balance, wide-based gait, fatigue, bowel or bladder incontinence, paresthesias, and weakness of the extremities.
Physical Examination
A thorough physical examination should be performed in all patients with a solitary spine lesion, because the lesion may represent a metastasic deposit from a palpable organ such as the breast, prostate, rectum, testes, or thyroid. Moreover, sacral chordomas are often palpable on rectal examination.
Spinal Imaging
Conventional radiographs are obtained to evaluate the level of the lesion, the local anatomy, and the overall spinal alignment. A bone scan is helpful to confirm the solitary nature of the tumor. Computed tomography (CT) defines bony architecture and demonstrates characteristic findings of hemangiomas, osteoid osteomas, and osteochondromas. Magnetic resonance imaging (MRI) provides additional information about soft-tissue extension and neural involvement.
Special Diagnostic Tests
The precise diagnosis of the tumor is often dependent on obtaining tissue for pathologic analysis. A biopsy should be performed and thoroughly analyzed prior to proceeding with definitive care unless the patient has a progressive neurologic deficit due to spinal cord compression. However, most patients do not present with a progressive neurologic deficit even in the presence of marked spinal cord compression. Initiation of corticosteroids usually stabilizes the patient’s neurologic function and provides some pain control in the short term. However, a biopsy should ideally be obtained prior to initiating steroids because corticosteroids have an oncolytic effect on myeloma and lymphoma, which might impair the diagnostic workup. Suboptimal technique in performing the biopsy may decrease the ability to perform complete excision of the tumor. A core needle biopsy rather than an open biopsy is preferred because a core needle biopsy minimizes contamination of the biopsy tract compared with an open biopsy. Minimizing contamination preserves surgical options, which include en bloc excisions. If the core needle biopsy is not diagnostic, then an open biopsy is indicated.
An emergent decompression with concomitant frozen section analysis is warranted in the rare individual presenting with a severe acute neurological injury or progressive neurological deficit. A posterior biopsy and decompression procedure preserves more surgical options and can function as the first stage of an en bloc excision if deemed necessary. If the pathologist suspects a primary malignant bone tumor, then the thecal sac should be decompressed and an experienced spine tumor surgeon with expertise in en bloc excisions should be consulted as soon as possible. Minimizing local contamination with tumor cells is essential to decrease the likelihood of local recurrence and preserve treatment options. Decompression, tumor removal, and definitive stabilization are considered if carcinoma is identified on the frozen-section analysis.
 Treatment
Treatment
En bloc excisions of benign and malignant primary bone tumors of the spine can prolong survival and decrease the incidence of local recurrence more than intralesional excisions can. Although many symptomatic benign primary bone tumors can be successfully treated with an oncologic intralesional excision (complete removal of pathologic and reactive tissue), an en bloc marginal excision should be considered for patients with benign or malignant tumors isolated to the distal sacrum (below S2), the vertebral body, or the posterior arch of the vertebra. En bloc excisions of benign tumors involving the proximal sacrum or pedicle of the vertebral body may not be warranted because of the morbidity associated with these complex resections. Benign tumors involving the pedicle can be completely removed with an en bloc marginal excision combined with an intralesional excision of the tumor within the pedicle. En bloc excisions of tumors involving the proximal sacrum or vertebral body and pedicle are usually reserved for patients with malignant primary bone tumors.
Maintaining spinal stability by obtaining a solid fusion is especially important when treating patients with aggressive benign (giant cell tumor and osteoblastoma) and low-grade malignant (chordoma and low-grade chondrosarcoma) primary bone tumors, because these tumors have a relatively high incidence of local recurrence. A local recurrence in the setting of a solid fusion is a less challenging situation than a local recurrence in the presence of spinal instability. Appropriate oncologic excisions, combined with meticulous fusion techniques and biomechanically sound reconstructions, improve oncologic and functional outcomes by decreasing the incidence of local recurrence and increasing the likelihood of obtaining a stable spine fusion.
Conventional radiation therapy is not usually advised for the treatment of benign or malignant primary bone tumors. Most benign primary bone tumors are successfully treated with nonoperative measures or an appropriate oncologic excision. The potential benefit of decreasing the incidence of local recurrence thus does not usually outweigh the risk of malignant transformation or damage to the surrounding tissue following radiation therapy. Conversely, radiation therapy is not used for most malignant primary bone tumors because many of these tumors (chondrosarcoma, chordoma, and osteosarcoma) are relatively radioresistant. Ewing sarcoma and osteosarcoma are generally best treated with neoadjuvant chemotherapy followed by an en bloc excision for definitive local control. However, radiation therapy may decrease the incidence of local recurrence in patients with Ewing sarcoma with residual microscopic disease following an oncologic excision with contamination. Additionally, stereotactic radiation therapy has been used to treat primary spinal sarcomas that have been deemed unresectable. Lymphoma is usually treated with chemotherapy alone, but radiation therapy is a useful adjuvant when necessary. Radiation therapy is also useful for patients with plasmacytoma and myeloma.
 Complications
Complications
Incomplete resection of a lesion is associated with a high rate of recurrence for certain primary bone tumors. Other surgical complications, including infection, bleeding, failed fusion, and neurologic injury, are seen when surgical reconstruction is undertaken.
 Outcome
Outcome
The outcome is dependent on the type of tumor and the adequacy of resection.
Suggested Readings
Bergh P, Kindblom LG, Gunterberg B, Remotti F, Ryd W, Meis-Kindblom JM. Prognostic factors in chordoma of the sacrum and mobile spine: a study of 39 patients. Cancer 2000;88(9): 2122–2134 PubMed
This study reports the improved local control and survival of patients with sacral or mobile spine chordoma treated with en bloc excisions compared to intralesional excisions.
Boriani S, Bandiera S, Biagini R, et al. Chordoma of the mobile spine: fifty years of experience. Spine 2006;31(4):493–503 PubMed
Forty-eight patients with chordoma involving the mobile spine were evaluated. Fourteen of these patients who received radiation alone, intralesional excision, or a combination had a local recurrence and died. Intralesional, extracapsular excision combined with radiation therapy resulted in local recurrence in 12 of 16 patients (75%), whereas only 6 of 18 patients (33%) who underwent en bloc excision had a local recurrence.
Boriani S, Biagini R, De Iure F, et al. En bloc resections of bone tumors of the thoracolumbar spine. A preliminary report on 29 patients. Spine 1996;21(16):1927–1931 PubMed
The Weinstein-Boriani-Biagini (WBB) surgical staging system is discussed. This system divides the vertebra into 12 radiating zones in clockwise order from 1 to 12. This system allowed the authors to treat 29 patients with an en bloc resection uniformly. No local recurrences were reported.
Boriani S, De Iure F, Bandiera S, et al. Chondrosarcoma of the mobile spine: report on 22 cases. Spine 2000;25(7):804–812 PubMed
These authors concluded that en bloc excision, with wide or marginal histologic margins, is the suggested management for chondrosarcoma of the spine. Three local recurrences occurred in 12 patients who had an en bloc excision compared to 10 recurrences in 10 patients treated with an intralesional excision. All patients who had an en bloc excision were alive at last follow-up, while 8 of 10 patients who had an intralesional excision had died.
Boriani S, De Iure F, Campanacci L, et al. Aneurysmal bone cyst of the mobile spine: report on 41 cases. Spine 2001;26(1):27–35 PubMed
These authors concluded that selective arterial embolization may be the first treatment option for aneurysmal bone cysts affecting the spinal column because 75% (3/4) of patients were cured with embolization. Moreover, embolization did not affect subsequent surgical treatment options.
Delauche-Cavallier MC, Laredo JD, Wybier M, et al. Solitary plasmacytoma of the spine. Long-term clinical course. Cancer 1988;61(8):1707–1714 PubMed
Nineteen patients with plasmacytoma of the spine were treated with chemotherapy and radiation therapy. They reported an expected 85% 10-year survival. Dissemination or local recurrence was observed in 13 of 19 patients.
Garg S, Mehta S, Dormans JP. Langerhans cell histiocytosis of the spine in children. Long-term follow-up. J Bone Joint Surg Am 2004;86-A (8):1740–1750 PubMed
Twenty-six children with biopsy-proven Langerhans cell histiocytosis involving the spine were evaluated. Patients with solitary lesions were treated symptomatically with a spinal orthosis and followed clinically and radiographically. Two (8%) patients required surgical treatment for progressive deformity. These authors concluded that aggressive surgical management is usually not indicated for these patients.
Kawahara N, Tomita K, Murakami H, Demura S, Yoshioka K, Kato S. Total en bloc spondylectomy of the lower lumbar spine: a surgical technique of combined posterior-anterior approach. Spine 2011;36(1):74–82 PubMed
Ten patients with a spinal tumor of the lower lumbar spine underwent total en bloc spondylectomy (TES) by combined posterior-anterior approach. The authors found that the lumbar nerves were preserved by the combined posterior-anterior approach for spinal tumors of L4 or L5.
Lin PP, Guzel VB, Moura MF, et al. Long-term follow-up of patients with giant cell tumor of the sacrum treated with selective arterial embolization. Cancer 2002;95(6):1317–1325 PubMed
The authors describe a reasonable alternative to surgical intervention for large giant cell tumors involving the sacrum or spinal column. They conclude that embolization should be considered in the treatment of this difficult disease because the risk-to-benefit ratio of surgical intervention with or without radiation therapy is probably higher than that of embolization.
Mankin HJ, Lange TA, Spanier SS. The hazards of biopsy in patients with malignant primary bone and soft-tissue tumors. J Bone Joint Surg Am 1982;64(8):1121–1127 PubMed
These authors showed that biopsy-related problems occurred three to five times more often when the biopsy was performed at a referring institution rather than the treating center. The optimal treatment plan was altered in 18% (60/329 patients) of patients, and the prognosis and outcome were adversely affected in 8.5% (28/329) of patients. These authors concluded that the surgeon and the institution should be prepared to perform accurate diagnostic studies and to proceed with the appropriate definitive treatment or refer these patients to a treating center prior to biopsy.
Marco RAW, Gentry JB, Rhines LD, et al. Ewing’s sarcoma of the mobile spine. Spine 2005;30(7): 769–773 PubMed
This study evaluates a homogeneous group of patients with Ewing sarcoma of the mobile spine who were treated with multiagent chemotherapy combined with radiation therapy for definitive local control. These patients demonstrated improved survival rates compared to patients treated with radiation therapy alone. However, these patients had a high risk of local recurrence and postlaminectomy kyphosis. The authors concluded that current spinal resection and reconstruction techniques may lead to improved oncologic and clinical outcomes.
This is an excellent comprehensive review of the potential pitfalls involved with spine tumor surgery of the cervical, thoracic, lumbar, and sacral spine.
Rao G, Ha CS, Chakrabarti I, Feiz-Erfan I, Mendel E, Rhines LD. Multiple myeloma of the cervical spine: treatment strategies for pain and spinal instability. J Neurosurg Spine 2006;5(2): 140–145 PubMed
The authors report the results of radiotherapy and surgical treatment of patients with myeloma involving the cervical spine. The authors suggest that external-beam radiation can effectively treat most patients with clinical or radiographically documented instability.
Schoenfeld AJ, Hornicek FJ, Pedlow FX, et al. Osteosarcoma of the spine: experience in 26 patients treated at the Massachusetts General Hospital. Spine J 2010;10(8):708–714 PubMed
The authors confirm a poor prognosis for patients with osteosarcoma of the spine. They find that a combination of therapies, including surgery, chemotherapy, and high-dose radiation, achieve adequate short-term survival, but the 5-year mortality rate remains high.
Sundaresan N, Schmidek H, Schiller A, Rosenthal D, Eds. Tumors of the Spine: Diagnosis and Clinical Management. Philadelphia, PA: WB Saunders; 1990
This is an excellent review of the evaluation and treatment of benign and malignant primary bone tumors.
Tomita K, Kawahara N, Baba H, Tsuchiya H, Fujita T, Toribatake Y. Total en bloc spondylectomy. A new surgical technique for primary malignant vertebral tumors. Spine 1997;22(3): 324–333 PubMed
These authors provide a step-by-step description of their en bloc spondylectomy technique.
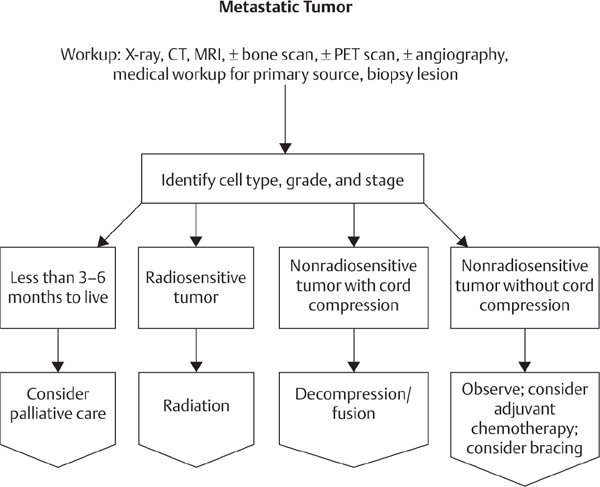
CT, computed tomography; MRI, magnetic resonance imaging; PET, positron emission tomography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







