Previous Proximal Femoral Fracture and Proximal Femoral Deformity
John F. Tilzey and Richard Iorio
Key Points
Introduction
The presence of proximal femoral deformities secondary to previous fracture or orthopedic disease may make femoral reconstruction during total hip arthroplasty difficult, or impossible, with routine femoral implants and techniques.
Indications
During total hip arthroplasty (THA), most variations in anatomy of the proximal femur can be treated with standard femoral components, cemented and cementless. The proximal femur may be considered deformed when the anatomy precludes the use of standard total hip implants and requires complex techniques and atypical components more often associated with revision THA. This variation in anatomy may be due to developmental dysplasia of the hip or other developmental abnormalities, trauma with previous surgical intervention, or metabolic bone disease.
Berry1 devised a method of classifying femoral deformity principally determined by anatomic site with subclassification of deformity secondary to geometry: A = torsional anteversion or retroversion; B = angular such as varus and valgus, or flexion and extension; C = translational; and D = size alterations (larger or smaller bone than usual) and cause of the deformity (i.e., developmental, metabolic, previous osteotomy, or previous fracture) (Box 77-1). The anatomic site and the type of deformity will affect choice of implant, implant size, and need for possible osteotomy. The Paprosky classification of femoral deficiency2 is useful in preoperative planning with regard to choice of implant and surgical technique (Box 77-2).
Deformities of the femoral neck include excessive anteversion, as is most commonly seen in developmental dysplasia of the hip (DDH). Operative options for excessive anteversion include a low neck osteotomy and diaphyseal fixation with a fully porous-coated stem or a proximal modular stem with optimum stem version obtained by final placement of the stem within the proximal sleeve.
Deformity involving the greater trochanter can present as trochanteric overhang or proximal femoral varus malalignment. Therefore, straight access to the proximal femoral canal can be compromised, causing varus malalignment of the implant. A greater trochanteric osteotomy (see Case 3) trochanteric slide or a subtrochanteric osteotomy can be used to facilitate straight access to the femoral diaphysis. The proximal femur and the greater trochanter are repaired to the construct and lateralized; this can improve abductor muscle tension and lever arm moment.
With deformities of the metaphysis and the proximal femoral diaphysis caused by fracture malunion or previous corrective osteotomy, an osteotomy at the level of the deformity may be required to allow distal fixation and proximal reconstruction. In these cases, a proximal modular stem or an extensively porous-coated stem may be useful.
Metal-on-metal total hip resurfacing arthroplasty has become a popular procedure for patients with hip arthrosis, especially younger male patients, with a reasonably predictable intermediate outcome and a low complication rate.3 Mont and colleagues4 suggested that another potential advantage of total hip resurfacing arthroplasty is preservation of proximal native femoral bone, which may make hip resurfacing an option for those patients with a proximal femoral deformity, intramedullary sclerosis as in Paget’s disease, or retained hardware, which may make reconstruction with a stemmed femoral component more difficult.
Contraindications
Contraindications to arthroplasty in these complex cases are similar to those for primary THA. Patients with Paget’s disease in the active, lytic phase of bone resorption may have vascular proliferation and associated bone pain. THA performed during this phase may be associated with increased intraoperative blood loss, increased bone pain, perioperative systemic hypercalcemia and accelerated bone resorption, and increased risk of local bone resorption around the hip implants. This active, lytic phase of Paget’s disease may present a relative contraindication to total hip arthroplasty. Pagetoid lytic activity can be assessed with a technetium bone scan. Serum alkaline phosphatase is an indicator of bone formation, and urinary hydroxyproline excretion is an indicator of bone resorption. These levels may be used as markers, in conjunction with the bone scan, to correlate the extent and activity level of the disease. Preoperative medical management of the active lytic phase of Paget’s disease with systemic antiresorptive agents may decrease the risk of complications. Sarcomatous degeneration of pagetoid bone occurs in less than 1% of patients. If pagetoid changes become rapidly destructive and increasingly painful with associated cortical erosions, with or without a soft tissue mass, sarcomatous degeneration must be considered.
Preoperative Planning
Careful preoperative planning is mandatory in these complex cases and cannot be overemphasized. Deformity of the proximal femur, retained hardware, and sclerosis of the femoral canal can all be determined with the use of conventional radiographs. Occasionally, a CT scan may be useful in assessing possible fracture or nonunion. Magnetic resonance imaging is rarely useful unless sarcomatous degeneration is suspected. Obtaining previous operative reports and identifying which implants are in place can aid in extraction and may provide information that is useful for future planned reconstruction.
Magnification markers make templating of components more predictable. In cases where nonunion and retained hardware exist, preoperative workup routinely includes serum C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) as sensitive screening markers for occult infection.5 If these markers are elevated, then aspiration of the hip joint or biopsy of the nonunion site for culture is necessary. At the time of surgery, frozen section analysis of local tissue is performed on intraoperative tissue specimens from areas of retained hardware; this tissue is also sent for culture in the setting of conversion arthroplasty.
Templating of components on the anteroposterior (AP) and lateral radiograph will determine whether an osteotomy, either of the trochanter or at the apex of the deformity, will be required (Figs. 77-1 and 77-2). The lateral radiograph is useful to determine any apex anterior or posterior deformity because perforation of the femur can occur with a straight stem. For all complex cases, intraoperative fluoroscopy is used with the patient on a radiolucent operating table.
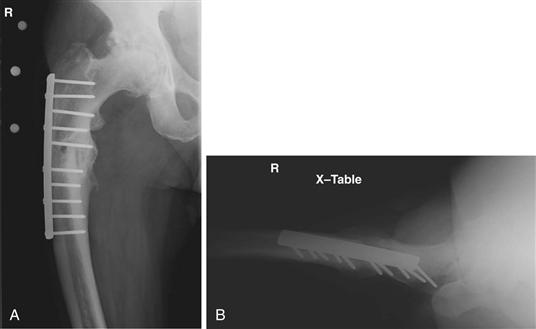
Figure 77-1 A, Preoperative anteroposterior x-ray and (B) lateral x-ray. Patient had previous open reduction and internal fixation of a subtrochanteric femur fracture with subsequent proximal femoral varus malunion.

Figure 77-2 Sequence of images using a digital templating system to correct deformity and to determine the appropriate femoral implant for reconstruction. A, Proximal femoral segment is outlined. B, Appropriate deformity is corrected. C, Fully porous-coated femoral implant is selected and sized. D, Postoperative anteroposterior radiograph.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








