Previous Acetabular Fracture
Michael D. Ries
Key Points
Introduction
Total hip arthroplasty (THA) is an effective treatment for post-traumatic arthritis. However, results of THA after previous acetabular fracture are generally less favorable than results of primary THA for osteoarthritis or inflammatory arthritis.1–9 After prior acetabular fracture, a number of issues may increase the complexity of THA; these include protrusio deformity, cavitary bone defects, segmental peripheral bone loss, prior infection, retained hardware, limb shortening, sciatic nerve palsy, abductor deficiency, and heterotopic bone formation.
Patients with post-traumatic arthritis after prior acetabular fracture can present to the reconstructive surgeon with a wide spectrum of challenges. However, favorable results can generally be achieved with careful preoperative planning and use of surgical techniques, including removal of hardware when necessary, identification of the sciatic nerve, bone grafting or modular augmentation of acetabular defects, use of a large cementless cup or cage with screw fixation, and perioperative radiation therapy or nonsteroidal anti-inflammatory drugs (NSAIDs), to minimize the risk of recurrent heterotopic bone formation.
Indications/Contraindications
Indications for THA after prior acetabular fracture include pain unresponsive to conservative therapy resulting from post-traumatic arthritis or avascular necrosis, and functional impairment caused by limited hip range of motion or limb shortening. Active infection is a contraindication to THA. Factors that may increase the risk of failure or complications after THA include prior infection, high patient activity level, and abductor deficiency.
Preoperative Planning
Radiographic Evaluation
Radiographic evaluation includes an anteroposterior (AP) view of the pelvis, as well as AP and lateral views of the affected hip. Additional Judet views can be helpful to delineate bony deformity in the anterior and posterior columns, the presence of discontinuity, and the location of retained hardware. Acetabular fractures that involve the anterior or posterior columns disrupt the anatomy of the medial acetabular wall (Fig. 76-1). Medialization of the cup to the acetabular floor will result in cup placement medial to the anatomic position of the acetabulum. Prior fracture of the posterior wall without fracture of either column does not disrupt the floor or medial wall of the acetabulum so the cup can be medialized to the anatomic acetabular floor (Fig. 76-2).
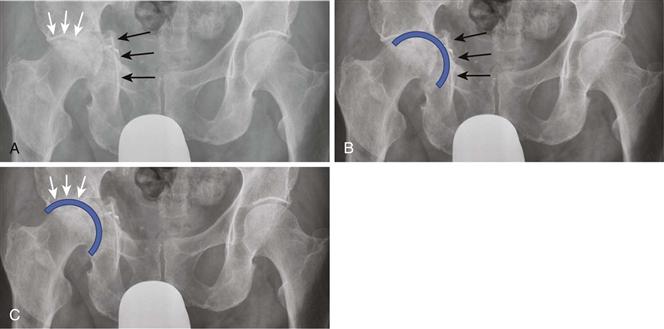
Figure 76-1 A, An anteroposterior (AP) pelvic radiograph demonstrates a healed acetabular fracture with medial displacement of the acetabular floor (black arrows). The superior acetabular dome (white arrows) was not involved in the fracture and remains in its anatomic position. B, If the acetabular cup is medialized to the acetabular floor, the center of the hip will be displaced medially relative to its native anatomic position. C, If the cup is positioned along the superior dome and lateral to the acetabular floor, the cup center will be restored to its prefracture anatomic location.
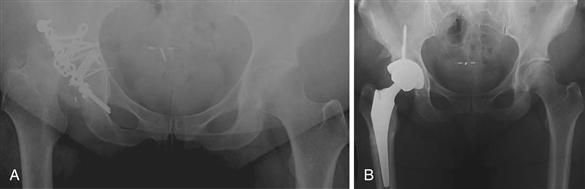
Figure 76-2 A, An anteroposterior (AP) radiograph illustrates a fracture of the posterior wall that has been plated. However, the columns were not fractured, so the acetabular floor is not displaced. B, A postoperative radiograph illustrates that the cup has been medialized to the acetabular floor and the hardware removed. Because the acetabular floor was not displaced, the hip center remains in its anatomic position.
Prior acetabular trauma, which included a fracture of the anterior or posterior column or a transverse fracture, typically results in a deformity in which the inferior hemipelvis is displaced medially. Figure 76-3A illustrates a healed transverse acetabular facture with retained screws in the anterior and posterior columns. Kohler’s line (yellow line) on the (left) noninvolved acetabulum is illustrated from the medial border of the sciatic notch to the lateral border of the obturator foramen. However, the hemipelvis inferior to the sciatic notch (white arrow) of the right post-traumatic hip has been displaced medially. Figure 76-3B illustrates the templated position of an acetabular cup, which has been medialized to the acetabular floor. However, because the acetabular floor and teardrop (purple arrow) are displaced medially, the cup is medial to the anatomic position of the sciatic notch (black arrow). This will result in medialization of the hip relative to the upper hemipelvis.
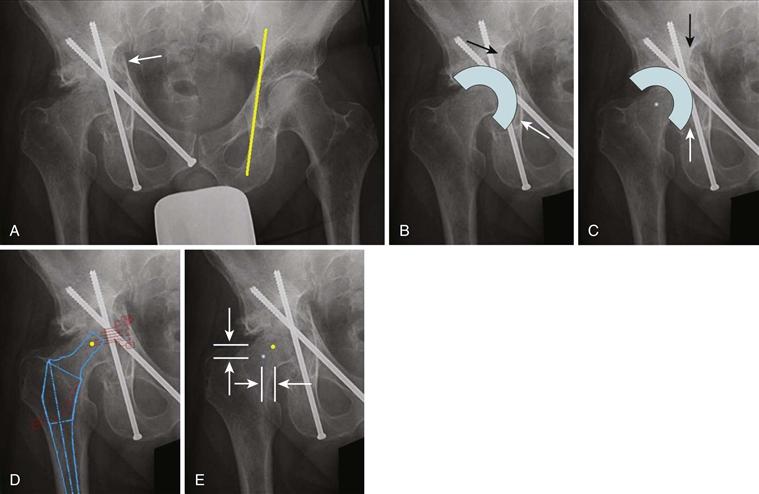
Figure 76-3 A, An anteroposterior (AP) pelvic radiograph illustrates a healed transverse acetabular fracture with post-traumatic arthritis. Kohler’s line (yellow line) on the (left) noninvolved acetabulum extends from the medial border of the sciatic notch to the lateral border of the obturator foramen. The acetabular floor inferior to the sciatic notch (white arrow) of the right post-traumatic hip has been displaced medially. B, The templated position of an acetabular cup that has been medialized to the acetabular floor will result in excessive medialization of the hip relative to the normal anatomic hip center. Because the acetabular floor and teardrop (white arrow) are displaced medially, the cup is medial to the anatomic position of the sciatic notch (black arrow). This will result in medialization of the hip relative to the upper hemipelvis. C, A more favorable cup position is illustrated. The cup is lateralized relative to the existing acetabular floor. The inferior cup (white arrow) is now lateral to the teardrop but is no longer displaced medially relative to the anatomic position of the sciatic notch (black arrow). The templated hip center is illustrated at the center of the cup. D, After the acetabular component position has been templated, the femoral component should be templated. The center of the templated femoral head is illustrated as a yellow dot. E, The center of the templated acetabular cup (shown in Fig. 76-3C) and the center of the templated femoral head (black dot in Fig. 76-3D) are illustrated. The expected change in leg length (distance between vertical arrows) and lateral offset (distance between horizontal arrows) can be determined by the difference in position of the center of the acetabular cup and the center of the femoral head.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








