Prevention of Venous Thromboembolism in Surgery of the Hip
Clifford W. Colwell Jr.
Key Points
• Assess all patients for factors increasing the risk of venous thromboembolic events (VTE).
• Having total hip arthroplasty (THA) puts patient in a high-risk group.
• THA patients are often older, with comorbidities that increase the risk of VTE.
• Multiple methods of VTE prophylaxis are available.
• Low-molecular-weight heparin (LMWH)
• Vitamin K antagonist (VKA) (warfarin)
• Aspirin
• Boots
• Bleeding is a concern for all types of prophylaxis.
• Continue to assess clinically for VTE during hospitalization and at follow-up.
Introduction
Prophylaxis for venous thromboembolic events (VTE) for total hip arthroplasty (THA) patients is an accepted fact. However, the method of prophylaxis is the topic of ongoing controversy. The incidence of VTE, including deep venous thrombosis (DVT) and pulmonary embolism (PE), is unacceptably high without any type of prophylaxis (Table 28-1). Although prophylaxis has been recommended since 1986,1 more is known about the epidemiology and risk factors, and methods for determining the presence of VTE and methods of prophylaxis have evolved. Low-molecular-weight heparins (LMWHs) have been available since 1993, and new oral anticoagulants. Compression devices have also been available for many years, but a recently developed portable compression device may alter nonpharmacologic prophylaxis. Various guidelines are available; confusion often surrounds which guidelines should be followed for optimal patient outcomes. A government agency and the accreditation body for hospitals have mandated that THA patients must be assessed and provided with prophylaxis after surgery. In this chapter, we will discuss all of these issues.
Table 28-1
VTE Prevalence After THA and Hip Fracture Surgery (HFS) Based on Mandatory Venography in Patients Who Received Placebo or No Prophylaxis
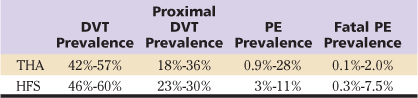
DVT, Deep vein thrombosis; PE, pulmonary embolism; THA, total hip arthroplasty; VTE, venous thromboembolism.
From Geerts WH, Pineo GF, Heit JA, et al: Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 127:2297–2298, 2005.
Epidemiology and Risk Factors
Thromboprophylaxis in THA begins with assessment of each patient’s risk for VTE. Given that surgery and orthopedic surgery of the lower extremity, specifically, automatically place our patients in the high-risk category, initial assessment for other factors that put the patient at even higher risk of VTE is done during preparation for surgery. This assessment may affect the type of prophylaxis prescribed and the length of time prophylaxis should be continued by the patient. Many available assessment tools8–13 provide checklists for risks and often suggest prophylaxis based on these risks (Box 28-1). Patients should be assessed perioperatively and during recovery for any signs or symptoms of VTE, in addition to receiving prophylaxis. Assessments should be documented in patients’ records to communicate with other healthcare professionals regarding assessment findings. Patients should be educated about clinical VTE signs and symptoms, so they can appropriately report these findings to their physician. Clinical signs alone, however, are notoriously flawed with respect to an accurate diagnosis and should be adjudicated by objective tests, which are almost universally carried out by duplex ultrasound.
Evidence suggests that proximal DVT is more important than distal DVT in terms of its sequelae and risk of development of subsequent PE.14 Proximal DVT occurs in veins above the knee, from the popliteal upward. Because these vessels are larger, the thrombosis is usually more significant and, if dislodged, could cause a larger PE. Studies have shown, however, that between 20% and 30% of thromboses that originate in the distal veins propagate to proximal veins and can cause PE.15–17 Calf vein thrombi are not totally benign: a high proportion leave residual venous abnormalities, including persistent occlusion and/or venous valvular incompetence,18 and post-thrombotic syndrome (PTS) develops in 5% of patients after total knee arthroplasty (TKA) and THA.19 Therefore, prophylaxis to prevent proximal and distal DVT, as well as PE, appears to be important.
Genetics and Clotting Factors
Genetic factors, including mutations of factor V Leiden, prothrombin gene G20210A, have been reported to increase the risk of VTE in the population. One study of TKA or THA patients indicated that the prothrombin gene mutation G20210A was significantly represented in those in this group with symptomatic VTE (P = .0002).20 A tendency toward increased risk of VTE was found with factor V Leiden mutation (P = .09).20 However, because 90% of the population who had these genetic risk factors did not have a VTE, general preoperative genotype screening is of questionable value.
Clotting factors, which have been associated with VTE, include increased levels of factor VIII21 and fibronectin.22 However, these factors have not been examined in relation to orthopedic surgery patients and VTE. Also implicated is a low level of high-density lipoprotein (HDL),23 although this has not been studied in the orthopedic surgical patient. Another study reports a positive relationship between plasma cholesterol ester transfer proteins and increased coagulability in young males,24 although again, whether this would transfer to surgical patients is not known.
Recently, two genetic variants of the enzyme that metabolizes warfarin, cytochrome P-450 2C9 (CYP2C9) and vitamin K epoxide reductase (VKORC1), have been associated with differences in patient response to warfarin doses.25 One study of this genetic-based dosing in TKA and THA has been reported.26 This study of 92 patients proposed an algorithm for warfarin dosing after orthopedic surgery that took into consideration genetic type, clinical variables, current medication, and preoperative and postoperative laboratory values. With validations, a safer, more effective process for initiating warfarin therapy could be provided.
Pathophysiology
In discussing thrombosis, the difference between venous thrombosis and arterial thrombosis needs clarification. Thrombosis in arteries is usually triggered by underlying arteriosclerosis and is composed mainly of platelets that deposit in the sclerotic rough area. Venous thrombosis is composed mainly of clotting proteins, with platelets playing a very minor role. Therefore, the methods used to prevent one type of thrombosis do not necessarily work for the other type of thrombosis. The essence of this chapter is the occurrence of venous thrombosis following THA.
Clinical Features and Diagnosis
Diagnosis
Doppler duplex ultrasound is a major tool used in practice and in research to detect DVT in patients with joint arthroplasty of the lower extremities. Because venous ultrasound is noninvasive, has almost no contraindications, and can be used as a repeated measure, it has become the most widely used test for clinical detection of symptomatic and asymptomatic DVT.27 Doppler ultrasound is also used by some surgeons as a screening tool to determine whether any thrombi are present at the time of hospital discharge. Screening has not been shown to be effective in changing an existing protocol because of short hospital stays after THA.28 Although compression venous Doppler ultrasound has been shown to have high specificity in the thigh in almost all institutions,27,29 this specificity is not maintained in the calf by all institutions.
Because no standardized documentation procedure exists for Doppler ultrasound that allows central adjudication, venography is still considered the “standard” for large VTE prophylaxis studies of new anticoagulants seeking approval by the United States (U.S.) Food and Drug Administration (FDA). Venograms are rarely done in clinical practice to detect symptomatic DVT because of the invasiveness of the procedure, exposure to radiation and contrast agents, the cumbersome nature of the procedure, and resultant pain.
After lower extremity orthopedic surgery, 50% of deaths are caused by vascular events30 and death may occur within a matter of minutes, making prophylaxis critical. Diagnosis of symptoms of PE, after a check for an elevated D-dimer blood test, is currently done most often by computed tomographic pulmonary angiography (CTPA), although some institutions continue to use ventilation-perfusion (V-P) lung scans. Lung scans are categorized as normal, low probability, and high probability. An angiography study is done as follow-up to confirm the PE after an intermediate probability V-P scan. A study comparing these two techniques found that the procedures were similar in diagnosing PE and determined that 0.4% (2/561) of patients who had CTPA and 1.0% (6/611) of patients who had a V-P lung scan later developed a PE.31 Either method appears to be acceptable in diagnosing PE; however, a few failures with both screening methods have been reported.
Treatment
Pharmacologic Prophylaxis
The category of drugs most commonly used worldwide for VTE prophylaxis is LMWHs. These drugs are given subcutaneously in different doses with different timing, depending on the particular drug, but do not require laboratory monitoring or dose adjustment. Extensive data have shown that this category of drugs is safe and effective, although concern still exists about related bleeding. Fondaparinux, also given subcutaneously, is a synthetic pentasaccharide used for prophylaxis. Another drug commonly used is warfarin, a VKA, which is given orally. Warfarin is dosed by checking the prothrombin time using the international normalized ratio (INR) to adjust the warfarin dose (Table 28-2). The point at which each of these agents provides inhibition in the coagulation cascade is shown in Figure 28-1. Aspirin is prescribed in various doses and often is used as part of a multimodal approach. Meta-analysis has shown low-dose unfractionated heparin or aspirin prophylaxis to be more effective than no prophylaxis, but both are less effective than other prophylactic regimens in this high-risk THA patient group. Each of these drugs has the potential to cause unwanted bleeding.
Table 28-2
Pharmacologic Prophylaxis Options for THA
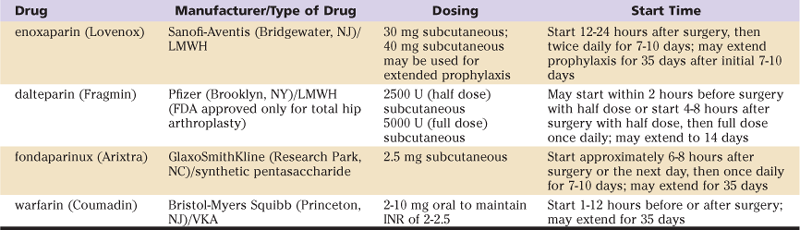
INR, International normalized ratio; LMWH, low-molecular-weight heparin; THA, total hip arthroplasty; VKA, vitamin K antagonist.
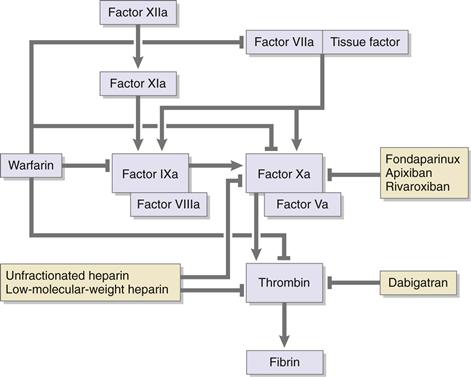
Figure 28-1 The points at which each VTE prophylactic drug agents provide inhibition in the coagulation cascade. (Redrawn from Colwell CW Jr: Prophylaxis for deep vein thrombosis after total knee arthroplasty. In Lieberman JR, Berry DJ, Azar FM [eds]: Advanced reconstruction: knee, Rosemont, Ill, 2010, American Academy of Orthopaedic Surgeons.)
Oral anticoagulation with adjusted-dose warfarin sodium is the most common and the longest practiced prophylaxis protocol by a majority of orthopedic surgeons in North America. Adjusted-dose warfarin has the potential advantage of allowing continued prophylaxis after hospital discharge provided the infrastructure is available to continue home therapy effectively and safely. Oral anticoagulation should be administrated in a dose sufficient to prolong the INR to a target of 2.5 (range, 2 to 3) (see Table 28-2). The half-life of warfarin is 36 to 42 hours, and its effects can be reversed with vitamin K. The initial oral anticoagulant dose may be administered before surgery or as soon after surgery as possible. However, even with early initiation of oral anticoagulation therapy, the INR does not usually reach the target range until the third postoperative day. The effectiveness of adjusted-dose warfarin is shown in Table 28-3.
Table 28-3
Major Randomized Trial Results
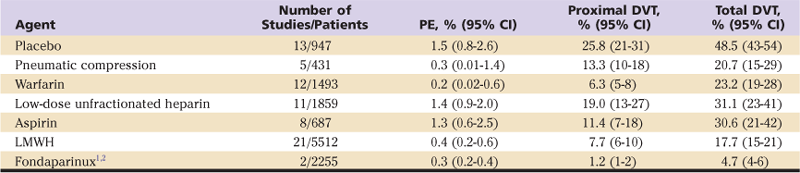
CI, Confidence interval; DVT, deep vein thrombosis; LMWH, low-molecular-weight heparin; PE, pulmonary embolus.
Data from Turpie AG, Bauer KA, Eriksson BI, Lassen MR: Postoperative fondaparinux versus postoperative enoxaparin for prevention of venous thromboembolism after elective hip-replacement surgery: a randomised double-blind trial. Lancet 359:1721–1726, 2002; Lassen MR, Bauer KA, Eriksson BI, Turpie AG: Postoperative fondaparinux versus preoperative enoxaparin for prevention of venous thromboembolism in elective hip-replacement surgery: a randomised double-blind comparison. Lancet 359:1715–1720, 2002; Freedman KB, Brookenthal KR, Fitzgerald RH Jr, et al: A meta-analysis of thromboembolic prophylaxis following elective total hip arthroplasty. J Bone Joint Surg Am 82:929–938, 2000.
The safety of using warfarin prophylaxis requires that patients understand the benefits and the risks of this medication. Clinical studies report a major bleeding event similar to that seen with placebo (Table 28-4). Many factors, including medications, smoking, alcohol, foods, and changes in activity, may interact with warfarin. Because many patients are discharged with warfarin prophylaxis, patients must be made aware of these interactions and must monitor themselves for any symptoms of over-anticoagulation. Optimal use of warfarin requires consideration of the time frame of its effects, use of the INR for close monitoring of effects and interacting factors, patient education, and a systematic approach.
Table 28-4
Major and Minor Bleeding As Defined by Study for Anticoagulant Treatment Type
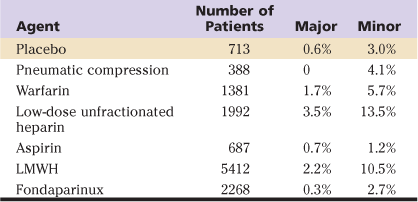
LMWH, Low-molecular-weight heparin.
Data from Turpie AG, Bauer KA, Eriksson BI, Lassen MR: Postoperative fondaparinux versus postoperative enoxaparin for prevention of venous thromboembolism after elective hip-replacement surgery: a randomised double-blind trial. Lancet 359:1721–1726, 2002; Lassen MR, Bauer KA, Eriksson BI, Turpie AG: Postoperative fondaparinux versus preoperative enoxaparin for prevention of venous thromboembolism in elective hip-replacement surgery: a randomised double-blind comparison. Lancet 359:1715–1720, 2002; Freedman KB, Brookenthal KR, Fitzgerald RH Jr, et al: A meta-analysis of thromboembolic prophylaxis following elective total hip arthroplasty. J Bone Joint Surg Am 82:929–938, 2000.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








