18 Preventing the Second Hip Fracture
Addressing Osteoporosis in Hip Fracture Patients
Patients who have sustained a low-trauma or fragility fracture of the hip (i.e., from a fall from standing height or less)1 have a high relative risk of second hip fracture that ranges from 2.3 to 4.9.2–5 The risk is highest shortly following the fracture; 2.3% to 5% of patients with hip fracture will experience a second hip fracture within 12 months.6,7 Nearly one half of subsequent hip fractures occur within the first 2 years of the first hip fracture.2,5,6 Therefore, the time immediately subsequent to the patient’s presentation with a hip fracture is the most critical for secondary fracture prevention.
The patient with hip fracture has a high risk of future fracture, both because of the risk of falling and because of underlying osteoporosis, which is usually undiagnosed at the time of presentation. Eighty percent to 90% of fractures in 60- to 74-year old inpatients hospitalized for fracture treatment, and 90% to 95% of fractures in inpatients who are more than 75 years of age, can be attributed to osteoporosis.8 Paradoxically, interaction with these patient groups represents the best opportunity, even after hip fracture, for fracture prevention. It is well established that appropriate treatment of osteoporosis with calcium and vitamin D supplements and a bisphosphonate can increase bone mineral density (BMD) and prevent some future fractures in high-risk patients.9–15 Bisphosphonates have been demonstrated to lower the risk of subsequent hip fracture by 30% to 50% within 1 year of initiation in high-risk patients,9–11,16,17 because of altered bone remodeling that leads to improved bone architecture and strength, as well as an increase in bone density. Such treatment may also result in lower postfracture mortality rates.18,19 A clinical trial of zoledronic acid, an intravenous bisphosphonate, even demonstrated a decrease in all-cause mortality after hip fracture.16 An intervention to prevent falls is also important.20
However, even after hip fractures, which are the most serious and obvious consequence of osteoporosis, this care is often lacking.21–26 A systematic review of 37 articles on the diagnosis and treatment of osteoporosis following a fragility fracture found that, in a subset of 14 studies of patients with hip fracture, potential underlying osteoporosis was not investigated or treated in 49% to 96% of patients assessed in fracture clinics or by orthopaedic surgeons.23 Thus, the orthopaedic health care team that is engaged in treating and managing the patient with an acute hip fracture has an additional priority, which is to initiate a series of investigations and treatments for osteoporosis and falls that will reduce the high risk of a subsequent hip fracture.
Patient Profile
The mean age of a patient presenting with a hip fracture is between 74 and 83 years.6,7,19,27–32 The patient with an acute hip fracture often has preexisting mobility limitations, a history of falling, and multiple comorbidities. Cognitive impairment may be identified preoperatively and postoperatively in up to 50% of patients with hip fractures.27,33,34 Fracture patients who have cognitive impairment are less likely to be treated for underlying osteoporosis.28,35,36 With respect to osteoporosis treatment in patients with hip fracture and dementia, there exists an inappropriate point of view that “the horse is out of the barn” (i.e., it is too late to treat underlying osteoporosis because the fracture has already occurred). Nevertheless, treatment with bisphosphonates and with calcium and vitamin D supplementation has been demonstrated to be effective in decreasing the incidence of subsequent hip fracture in the elderly patient with hip fracture and Alzheimer’s disease.37,38 Thus, even the elderly patient with cognitive impairment who is at high risk of future fracture can benefit from osteoporosis treatment. These patients also require alterations to their physical environment and improvement of endogenous factors (e.g., eyesight, hearing, polypharmacy, and degree of sedation) to reduce their high risk of falls.
The most common site of origin of patients presenting to acute care hospitals with hip fracture is nursing homes. The rate of hip fracture among nursing home residents is approximately 3.5 to 5 times higher than in age-matched counterparts who live in the community: 2.3% to 10.4% of nursing home residents are reported to sustain a hip fracture each year.35,39–43 Osteoporosis is highly prevalent (61% to 85%) in nursing home environments, but only 25% to 36% of these patients receive treatment for osteoporosis.36,44–46 Even routine supplementation of residents’ diets with calcium and vitamin D in recognition of the known dietary deficiencies in this social cohort is lacking in many nursing homes.
Heart disease, cancer, diabetes, depression, arthritis, anxiety, and anemia are common in elderly patients with hip fracture. Up to 73% of elderly patients with hip fracture may have one or more medical comorbidities,27 both those listed here and others. Polypharmacy, or the regular administration of many medications to the patient, represents a barrier to the introduction of supplementation and prescription drugs to these patients. Nevertheless, patients with hip fracture who have an increased number of comorbidities have been reported to be more likely to continue with osteoporosis treatment at 1-year follow-up.31
Approximately one in four hip fractures occurs in men,7,18,19,47,48 and the first-year mortality rate after hip fracture is nearly twice as high in men (30%) compared with women (17%).49,50 The male patient with hip fracture is even more often overlooked for osteoporosis investigation and treatment.
The age at which hip fracture occurs appears to be increasing. Secular trends in hip fracture are for an increasing proportion of fractures to occur in the elderly old (i.e., >85 years of age). Osteoporosis treatment trials, like virtually all other medical trials, have not included large numbers of the elderly old subjects. Only more recently have osteoporosis treatment trials included significant numbers of the elderly old.19 Therefore, only a small amount of evidence is available to support osteoporosis treatment in the patient with hip fracture who is 85 years old or older. Notwithstanding this lack of data, serious consideration should be given to initiating antiresorptive medication and other measures such as falls prevention following a hip fracture, at least in community-dwelling or physically active patients with hip fracture who are 85 years old or older. Controversy exists over the indication for osteoporosis treatment in the severely demented or bed-bound nursing home resident who has a hip fracture.
Fracture Risk Assessment
The indications for osteoporosis treatment to prevent fractures were formerly based principally on BMD. This basis was problematic for several reasons: (1) half of all fragility fractures occur in patients whose BMD is in the osteopenic rather than the osteoporotic range51; (2) fracture risk based on BMD alone does not take into account the risk from falling; and (3) age is an important independent risk factor for fracture, especially hip fracture.
The World Health Organization (WHO) developed a Web-based Fracture Risk Assessment Tool (FRAX) based on a program of work undertaken at the WHO Collaborating Centre for Metabolic Bone Diseases at Sheffield University in the United Kingdom and led by Professor John A. Kanis.52,53 The FRAX allows health professionals to calculate the 10-year risk of hip fracture, as well as the 10-year risk of osteoporotic fracture, in male and female patients. Key patient demographics, such as age, sex, weight, height, and femoral neck BMD (if available), are entered into the Web site tool, as well as any clinical risk factors for osteoporosis, such as prior fragility fracture, parental history of hip fracture, smoking status, long-term use of glucocorticoids, rheumatoid arthritis, other causes of secondary osteoporosis, and daily alcohol consumption. These factors are assigned different weights, and the probability of future fractures is calculated as a percentage. For example, smoking and excess alcohol consumption are relatively weak risk factors, but a previous fracture and a family history of hip fracture are strong risk factors. The FRAX algorithms used to calculate the 10-year risk of fracture are based on studies of reference populations in Europe, North America, Asia, and Australia. A country-specific FRAX tool is available for the United States (black, white, Hispanic, and Asian ethnicity), Canada,53a the United Kingdom, Sweden, Germany, France, Austria, Belgium, Finland, Switzerland, Italy, Spain, Turkey, Lebanon, Argentina, Japan, Hong Kong, China, and New Zealand.
Other fracture risk models used as therapeutic decision tools exist. For example, in Canada tables by Siminoski and colleagues54 endorsed by Osteoporosis Canada, the Society of Obstetrics and Gynaecology of Canada, and the Canadian Association of Radiology perform a similar function for patients 50 years old and older. Age, sex, and BMD form the basis for calculation of a patient’s 10-year absolute fracture risk. Three bands of low risk (<10%), moderate risk (10% to 20%), and high risk (>20%) are established on graphs of BMD versus age, for men and for women. Two additional risk factors, history of fracture and use of glucocorticoid therapy for more than 3 months, each will increase a patient’s risk for future fracture to the next level: from low risk to moderate risk or from moderate risk to high risk. A person who has had a fragility fracture after the age of 40 years and is receiving glucocorticoid therapy is automatically considered to be at high risk, irrespective of age, sex, or BMD. An updated version released in 2010 has been validated in two large Canadian cohorts and shows concordance approaching 90% agreement with the Canadian FRAX system.54a
Determinants of Future Fracture Risk
Advanced Age
The mean age of patients with hip fracture ranges from 74 to 83 years across numerous studies,6,7,19,27–32 and most studies report a mean age of a least 80 years.6,7,27,28,31,32 From 54% to 77% of hip fracture patients are 75 years old or older at the time of fracture.18,19,29
These two factors, prevalent hip fracture and advanced age, both dramatically increase the risk for subsequent fracture,54,55 as noted earlier. Increasing age is associated with a higher rate of comorbidities and a greater number of medications,31 factors that increase the likelihood of falls and pose potential barriers to osteoporosis treatment.
Prior Fragility Fracture
A previous or prevalent fragility fracture substantially increases the risk for future fractures.2–5,7,53,54 Therefore all patients with hip fracture are at much higher risk of having another fracture, particularly of the hip. A common expression referring to this phenomenon is “fracture begets fracture.” Up to 10% of patients with hip fracture will experience a second hip fracture within 2 years of the first fracture.2,5–7,19,56
Tendency to Fall
Ninety percent of hip fractures occur as the result of a fall.57 Although only a small proportion of falls in persons 65 years old and older will result in a fracture, the tendency to fall is high among elderly persons and increases with age: one third of people 65 years old and older, and one half of those 85 years old and older, fall each year.58 In nursing homes, the tendency to fall is even greater, with a mean annual incidence of 1.5 reported falls per bed.59
Potential reasons for falls can include orthostatic hypotension, poor eyesight or hearing, and poor balance secondary to muscle weakness, stroke, or neurologic diseases. A falls prevention program should include investigation and treatment of these and other conditions. The subject of falls prevention is addressed in detail in Chapter 17.
Vitamin D Insufficiency or Frank Deficiency
Numerous studies have documented a high probability that patients with hip fracture present in a state of vitamin D insufficiency or frank deficiency. The definitions and cutoff values for vitamin D insufficiency and deficiency are under discussion and remain controversial. In a review of optimal serum vitamin D concentrations for multiple health outcomes, Bischoff-Ferrari and colleagues60 reported that a serum 25-hydroxyvitamin D concentration higher than 75 nmol/L was the most advantageous serum vitamin D level for fracture prevention, higher BMD, improved lower extremity function, reduced risk of falls, and reductions in tooth loss and periodontal disease. Even higher serum 25-hydroxyvitamin D concentrations of 90 to 100 nmol/L were recommended for prevention of hip fractures.60 Using this standard, blood serum levels of 25-hydroxyvitamin D that are lower than 75 nmol/L can be considered insufficient in patients with hip fracture. Vitamin D deficiency can now be considered to occur at blood serum levels lower than 50 nmol/L,61 although a more conservative definition of frank deficiency is a concentration lower than 25 nmol/L, a level at which osteomalacia and impaired muscle function may occur.
Vitamin D insufficiency is very common in patients with hip fracture when the foregoing measurements are used. By a more conservative definition, the incidence of unequivocal vitamin D insufficiency (<50 nmol/L) ranges from 62% to 91% in hip fracture populations and is even greater in nursing homes.61–66 Smaller numbers of these patients (10% to 40%) have a frank vitamin D deficiency (<25 nmol/L).30,61,66–68
Vitamin D not only influences bone mineralization and bone health but also is important in protein synthesis in muscle tissue that leads to improved muscle strength, particularly in the lower extremity.69 Thus, vitamin D insufficiency that results in muscle weakness may make a person more susceptible to falls and may thus increase fracture risk. Frank vitamin D deficiency in women at the time of hip fracture has been associated with atrophy of type II muscle fibers of the middle gluteal muscles, impaired lower extremity function, and an increased risk of falls at 1 year after the fracture.61,70 A meta-analysis of vitamin D supplementation studies showed that daily administration of 800 IU reduces the risk of falling by 22% when compared with calcium or placebo.60
Secondary Osteoporosis
An extensive review of the literature on causes of osteoporosis concluded that approximately two thirds of cases of osteoporosis in men, one half of cases of osteoporosis in perimenopausal and premenopausal women, and one fifth of cases of osteoporosis in postmenopausal women are due to secondary causes other than aging or menopause.71 Some of the more common secondary causes of osteoporosis include glucocorticoid use, alcoholism, renal disease, hyperparathyroidism (often associated with renal disease or vitamin D insufficiency), hypogonadism in female and male patients, calcium malabsorption, inflammatory bowel disease and inflammatory arthridities, cancer, and monoclonal gammopathy.71–77 Boonen and colleagues78 reported that up to 70% of male patients who have osteoporosis have non–age-related osteoporosis caused by conditions such as glucocorticoid use, alcoholism, and hypogonadism. In addition, low BMD secondary to osteomalacia, such as hypovitaminosis D, can be mistaken as osteoporosis. Thus, it is particularly relevant to investigate the male patient with hip fracture for secondary causes of bone loss, to exclude or identify (and treat) such conditions. In women, when osteoporosis is unusually severe or occurs at a younger age than usual, or when the medical history is suggestive, primary secondary causes of osteoporosis, such as subclinical hyperthyroidism, multiple myeloma, and Cushing’s disease, should be considered.
Different conditions, such as vitamin D deficiency, may require adjunct therapies. If such causes of bone loss are not identified and managed appropriately, then treatment of the associated osteoporosis may be suboptimal or ineffective. A rapid screening history may identify some of the common secondary causes of osteoporosis. A protocol of investigations is used when undiagnosed primary causes of secondary osteoporosis are suspected. These tests, which are adapted to the clinical situation, are listed in Table 18-1.
Table 18-1 Protocol of Investigations for Suspected Undiagnosed Primary Causes of Secondary Osteoporosis*
| Blood work | Complete blood count (CBC) |
| Parathyroid hormone (PTH) | |
| Alkaline phosphatase | |
| Creatinine | |
| Calcium | |
| 25-Hydroxyvitamin D | |
| Thyroid-stimulating hormone (TSH) | |
| Protein electrophoresis | |
| Tissue transglutaminase (test for celiac disease) | |
| Bioavailable testosterone (men only) | |
| Urinalysis | |
| Radiographs | Thoracic and lumbar spine (anteroposterior view; lateral view) |
* This investigational protocol conforms to the Canadian clinical guidelines for osteoporosis management.54a
Bone Mineral Density
According to 1994 and subsequent WHO guidelines,79,80 osteoporosis is diagnosed when BMD is 2.5 standard deviations (SD) or more below the young adult mean. Osteopenia (low bone mass) is defined as BMD that is more than 1 SD but less than 2.5 SD below the young adult mean. Using these diagnostic criteria, 87% to 96% of patients presenting with a hip fracture are diagnosed with either osteoporosis or osteopenia, and 48% to 61% have frank osteoporosis.19,48,81 These rates are even higher among patients with hip fracture in nursing homes.46
The question often arises when an elderly patient who has a typical osteoporotic hip fracture presents for treatment in the hospital: Does this patient require bone mineral densitometry for the osteoporosis to be correctly diagnosed and optimally managed? The existing guidelines were reviewed for provisions that apply to the patient presenting with an acute hip fracture. Although clinical guidelines generally recommend measurement of BMD for a definitive diagnosis of osteoporosis,79,82–86 there is some variation in the patient criteria that warrant BMD investigation of osteoporosis in 17 clinical practice guidelines for osteoporosis screening that were published in the United States, Canada, United Kingdom, and Australia.87 Whereas all the reviewed guidelines recommended screening of postmenopausal women less than 65 years old who had an additional risk factor (e.g., a prevalent fracture, although definitions of risk factors varied), and most recommended universal screening for women more than 65 years old, few guidelines addressed screening for osteoporosis in men.87 Osteoporosis Canada recommends BMD testing for targeted case finding among men and women less than 65 years old who have risk factors (e.g., prevalent hip fracture) and for all women and men 65 years old and older because of the increased risk of osteoporosis and fracture after that age.88 The National Osteoporosis Foundation in the United States recommends BMD testing in any person more than 50 years old who has a prevalent fracture.89
Does the Elderly Patient with Hip Fracture Require Bone Mineral Density Testing for Osteoporosis to be Optimally Managed?
With respect to the 10-year risk assessment of fragility fracture in the patient presenting with an acute hip fracture, the fracture risk tools applied to the elderly (i.e., age ≥70 years) patient with hip fracture usually arrive at an indication for pharmacologic treatment of osteoporosis. For example, in the FRAX tool for the United States,53 a 70-year-old woman who presents with an acute hip fracture and no other risk factors and a BMD T-score of –1.0 has a 20% 10-year probability of osteoporotic fracture. Another example would be an 80-year-old male patient in the United Kingdom who presents with an acute hip fracture and two other risk factors who would have a 21% 10-year probability of osteoporotic fracture if his BMD T-score is –2.0. A calculated risk of 20% or greater is considered a high risk for future fracture. The principal determinants of risk for osteoporotic fracture are (1) age, (2) prevalent osteoporotic fracture, (3) BMD, and (4) female gender. Because the elderly patient with hip fracture by definition has the first two risk factors, and because most of these patients are either osteopenic or frankly osteoporotic, elderly patients with hip fracture who present for treatment to the hospital are nearly always at high risk of future fracture (including hip) and thus have a strong indication for osteoporosis intervention.
Components of an Effective Osteoporosis Care Strategy
Correction of Vitamin D Insufficiency or Deficiency
Vitamin D insufficiency or deficiency is easily measured and is inexpensive to treat. Deficiencies are rapidly correctable, with minimal risk, through supplementation.68 Supplementation with vitamin D and calcium has been demonstrated to lower fracture rates in community-dwelling individuals who are more than 65 years old, as well as in individuals living in nursing homes.30,68 Vitamin D supplementation also improves the effectiveness of osteoporosis pharmacotherapy. Investigators reported that BMD significantly improved in patients with osteoporosis and osteopenia who did not respond to bisphosphonate therapy alone, after these patients were prescribed 1000 IU daily vitamin D.90
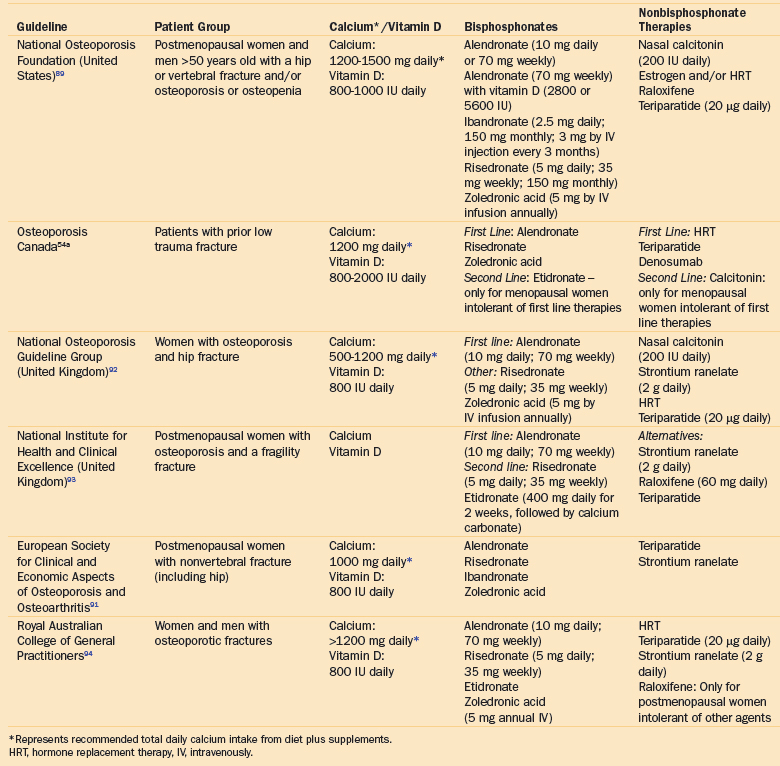
American,89 Canadian,54a European,91–93 and Australian94 guidelines for the management of patients with osteoporosis (with or without fragility fractures) recommend daily supplementation with calcium (500 to 1500 mg) and vitamin D (800 to 1000 IU). An increase in the recommended upper dose limit of vitamin D is under discussion by some experts. Optimal fracture prevention may require supplementation with more than 1000 IU of vitamin D, depending on latitude, housing status, and local fortification of dairy products with vitamin D.60 Nursing home residents may require substantially greater doses of vitamin D because of their age, immobility, and inadequate exposure to sunlight.68
The patient who is presenting with a hip fracture should be made replete for vitamin D. Initiation of supple- mentation in all hip fracture patients is recommended in hospital, followed by measurement of serum 25-hydroxy-vitamin D levels 3 months later.53a If a secondary cause of osteoporosis has been identified, blood and urine investigations are recommended prior to commencing therapy.53a,54a Whether bisphosphonate therapy should be started at the same time is controversial. Some authors recommend correction of vitamin D deficiency before administration of aminobisphosphonates, to avoid use of bisphosphonates in patients with actual or potential osteomalacia. However, many practitioners find it practical and safe to commence vitamin D supplementation at the same time as the initiation of bisphosphonate therapy. Initiation of pharmacologic treatment in a systematic way for hip fracture patients has been challenging, and many patients still do not receive therapy for prevention of future fractures. Initiation of pharmacologic therapy by protocol in hospital when the patient remains under the care of the orthhopaedic team and osteoporosis consultants is advantageous in this regard. Supplementation with 50,000 IU of vitamin D2 three times weekly for 4 weeks has been recommended for nursing home residents with serum 25-hydroxyvitamin D deficiency, to bring them back up to sufficient blood serum levels.68
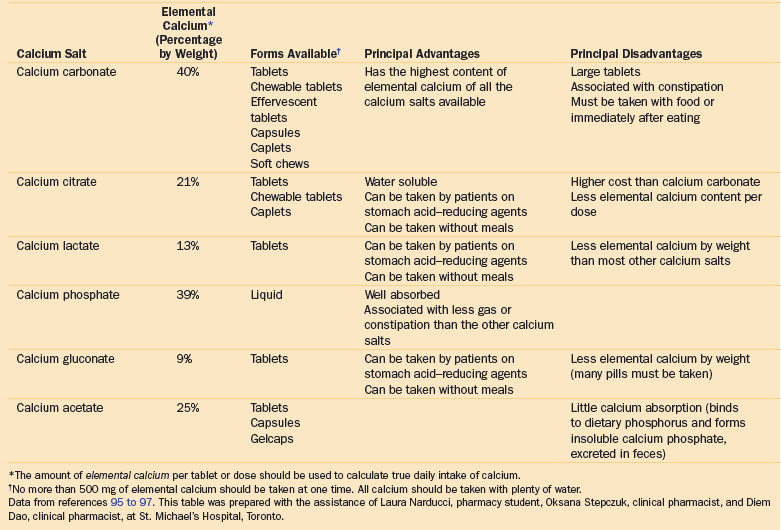
Calcium Supplementation
Calcium supplementation can be administered in a variety of forms (Table 18-2).95–97 A single dose should not exceed 500 to 600 mg of elemental calcium, to achieve maximum absorption. Thus, one or two daily doses may be required to meet international guideline recommendations for calcium supplementation (Table 18-3).
Table 18-3 A Selection of National Guidelines for Vitamin D and Calcium Supplementation and Pharmacologic Treatment for Patients Presenting with a Hip or Nonvertebral Fracture
Calcium carbonate, the most concentrated form of calcium supplementation, contains approximately twice the elemental calcium by weight of calcium citrate.96,97 Although calcium carbonate is inexpensive and widely available, many elderly patients reject it because of resulting constipation. When the large size of the tablets is a concern, alternate formulations such as effervescent tablets or soft chews may be suitable. Other forms of calcium, including calcium citrate, are available in smaller tablet sizes and smaller doses. Other options include crushing tablets and adding them to orange juice or other drinks. Calcium citrate is the preferred supplement for patients with achlorhydria, a common condition in the elderly, because of significantly higher absorption rates when compared with calcium carbonate.97 Calcium citrate may be a more convenient choice for nursing home residents, given that it does not need to be taken with meals. However, because of the smaller doses, the elderly patient may have to take a greater number of pills. The hospital or community pharmacist can be engaged to assist elderly patients with hip fracture in identifying a tolerable form of calcium administration.
The current recommendations for 1000 to 1500 mg of elemental calcium represent a total daily intake of calcium, from a combination of diet and supplements. Excess calcium intake may increase the risk of hypercalciuria and kidney stones. In elderly patients with decreased glomerular filtration rates, excess calcium can increase the risk of hypercalcemia and may also raise the risk of cardiovascular events.98 Additionally, because constipation resulting from calcium supplementation is a postoperative concern for the patient with an acute hip fracture, limiting calcium supplementation to 500 mg daily during the initial postoperative period may be prudent.
Falls Prevention
Most fragility fractures (90%) result from a fall.57 Patients with a high rate of falls, who also have low BMD, are at very high risk of fracture. A strategy for the prevention of future fractures requires an effective falls prevention program. Elements of such a program may include promoting physical activity to increase lower body strength and improve balance, adjusting medications to reduce side effects and interactions, ensuring that the physical environment is well lit and free of obstacles (including tripping hazards such as loose rugs and electrical cords), installing handrails and grab bars, having assistive devices (walkers, wheelchairs) within easy reach, and providing nonskid footwear or hip protectors. In addition, endogenous causes that may contribute to falls (e.g., orthostatic hypotension, poor eyesight or hearing, and inappropriate sedation) should be investigated. Falls prevention is discussed in detail in Chapter 17.
Bone Mineral Density Testing
As discussed in the earlier section on fracture risk assessment, the patient presenting with a hip fracture has a high probability of osteoporosis or osteopenia. Because the patient with hip fracture is also usually elderly (i.e., ≥70 years), he or she has a high calculable 10-year risk of a subsequent hip or other fragility fracture.53,54 The high risk of future fracture can often be assumed. As discussed earlier, BMD testing is therefore not always necessary before pharmacologic treatment for osteoporosis is begun when indicated in the elderly patient with hip fracture.99
BMD testing also provides an opportunity to educate both the primary care physician and the patient. In a study by Rozental et al100 on the initiation of osteoporosis treatment after fragility fracture of the wrist, the investigators found that primary care physicians who received the BMD values of their patients were approximately three times more likely to prescribe appropriate osteoporosis therapy than were physicians who received only a letter outlining national guidelines for osteoporosis evaluation and treatment. This finding is evidence that provision of BMD results to the primary care physician can be a powerful motivator for initiation of osteoporosis treatment in patients with a fragility fracture.
Providing and explaining BMD results can be motivating for patients as well and can increase compliance with osteoporosis therapy. Patients with osteoporosis or osteopenia who are aware of and understand their BMD results are more likely to be treated with osteoporosis medications and are also more likely to adhere to treatment than are patients who do not know their BMD results.101–103
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree