22
Posterolateral Corner Hamstring Figure-Eight Reconstruction
Isolated injury to the posterolateral structures of the knee is uncommon. The overall incidence of acute posterolateral rotatory instability (PLRI) has been reported to be less than 2% of all acute ligamentous knee injuries.1 These injuries are usually associated with injury to the anterior and posterior cruciate ligaments.2, 3 Because of this, there must be a high degree of clinical suspicion for injury to the structures of the posterolateral corner (PLC) when evaluating a patient with cruciate ligament involvement. Physiologic, or chronic, PLRI may exist in the absence of an acute injury to the knee. In these cases, the cruciate ligaments are often spared. Overall, the consequence of unrecognized and untreated PLRI can be failure of a reconstructed cruciate ligament.4–7
Much of the confusion regarding the diagnosis and treatment of PLRI is caused by the difficulty in understanding the anatomy and biomechanical function of the PLC structures. Seebacher and associates8 developed a three-layer anatomic concept of this area, including some of the following structures (Fig. 22-1): the iliotibial band (ITB), the lateral collateral ligament (LCL), the popliteus muscle and tendon, the popliteofibular ligament (PFL), the arcuate ligament, the biceps femoris muscle and tendon, the middle-third capsular ligament, the lateral gastrocnemius tendon, and the fabellofibular ligament. Recently, the importance of the LCL and PFL in preventing posterolateral instability has been reported.9–11 The PFL (Fig. 22-2) represents a direct, static component of the popliteus tendon from the posterior aspect of the fibular head to the anterior aspect of the lateral femoral epicondyle.12, 13 Much of the overall resistance to posterior tibial translation, varus rotation, and external rotation is provided by the PFL.10 The complex anatomy of the PLC makes it difficult to primarily repair its structures, and it is often necessary to use auto- or allograft tissue in reconstructing this region.
Ligament length relationships on the lateral and posterolateral aspect of the knee has been studied by Sidles and associates.14 Their study showed that, in a moving knee model, near isometry is maintained from the fibular head to the lateral femoral epicondyle. More specifically, it showed a more favorable length change between the anterior aspect of the fibular head and the posterior aspect of the epicondyle and between the posterior aspect of the fibular head and the anterior aspect of the epicondyle. Using this isometry data, Larson15 developed a surgical technique using a free semitendinosus tendon graft to reconstruct the LCL and PFL. A graft extending from the posterior aspect of the fibular head to the anterior aspect of the epicondyle represents the PFL and popliteus tendon. Similarly, a graft from the anterior aspect of the fibular head to the posterior aspect of the epicondyle represents the LCL. The actual anatomic insertion sites of the popliteus tendon and LCL on the lateral femoral epicondyle reflect this relationship. The technique described in this chapter is a modification of Larson’s technique.
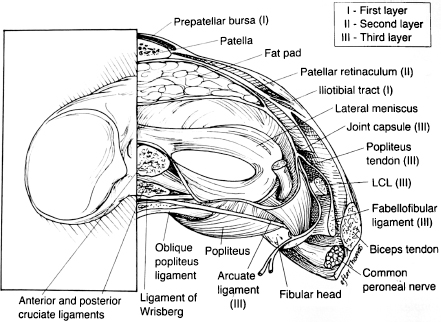
Figure 22-1 Coronal section of the knee illustrating the three-layer anatomic concept of the posterolateral knee structures. (Adapted from Chen FS, Rokito AS, Pitman MI. Acute and chronic posterolateral rotatory instability of the knee. J Am Acad Orthop Surg 2000;8:98, with permission.)
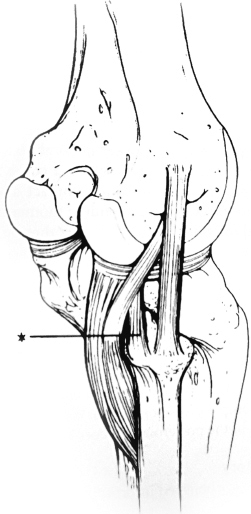
Figure 22-2 The popliteofibular ligament (asterisk) arises from the posterior aspect of the fibula and joins the popliteus tendon as a static attachment. (From Veltri DM, Warren RF. Anatomy, biomechanics, and physical findings in posterolateral knee instability. Clin Sports Med 1994;13;602, with permission.)
Surgical Idications
As stated earlier, having a high degree of clinical suspicion for PLRI will aid in its diagnosis. A careful review of the history, physical examination, and imaging studies is crucial to diagnosing and preoperatively planning for a patient with suspected PLRI.
History
A posterolaterally directed blow to the medial tibia with the knee in extension is the most common mechanism of injury that results in acute injury to the PLC.16 Although less frequent, injury to the PLC can occur in a noncontact, hyperextension and external rotation motion. The patient may report pain to the posterolateral aspect of the knee and complain of neurologic symptoms. Many studies have confirmed peroneal nerve involvement with this type of injury.1, 3, 17, 18 In the absence of an acute injury, chronic instability may be described as the knee giving way into hyperextension.
Physical Examination
The knee should be examined for edema, induration, ecchymosis, and tenderness. Also, gait pattern and limb alignment should be observed. Patients may walk with a slightly flexed knee to avoid hyperextension. They may also present with a varus alignment and an abnormal varus thrust during gait. There are several specific exams that have been developed to help in diagnosing injuries to the PLC (Table 22-1).
Imaging Studies
Both plain radiographs and magnetic resonance imaging (MRI) are helpful in the assessment of a patient suspected of having PLRI. In the acute setting, x-rays may show abnormal widening of the lateral joint line, a proximal fibula avulsion fracture, a Gerdy’s tubercle avulsion fracture, or a Segond fracture.1, 16 In cases of chronic instability, evidence of patellofemoral or tibiafemoral arthritis may be observed. The lateral compartment is more commonly involved. Full-length weight-bearing radiographs of both lower extremities help determine overall limb alignment and aid in any planned osteotomy.
When grade III injuries to the PLC can be diagnosed acutely, direct anatomic repair of all injured structures within 3 weeks offers the most optimal results.1–3, 17 However, in some cases, it can be difficult to perform an optimal physical exam on the acutely injured, painful knee. Because of this, MRI is an excellent diagnostic tool when evaluating injuries to the PLC. LaPrade and associates19 showed that, in cases of acute and chronic grade III injuries to the PLC, MRI can accurately define the most frequently injured posterolateral structures. MRI will also frequently reveal a contusion to the anteromedial femoral condyle.20 Lastly, MRI is useful in identifying injuries to the cruciate ligaments and other soft tissue structures of the knee. For these reasons, MRI is also an excellent preoperative tool that aids in planning the approach and sequence of reconstructing the injured structures.
| Exam | Maneuver | Interpretation |
| Anteroposterior translation | The patient is supine. At 30 and 90 degrees of flexion, posterior translation of the tibia on the femur is tested. | Increase at only 30 degrees: isolated PLC Increase at both 30 and 90 degrees: combined PLC and PCL |
| Varus-valgus stress | The patient is supine. Varus testing is performed at both 0 and 30 degrees. | Positive finding: increased varus laxity Isolated LCL: increase only at 30 degrees Combined LCL and PLC: increase at 0 and 30 degrees |
| External rotation recurvatum | The patient is supine. The great toes of both feet are grasped and lifted off the examining table. | Positive findings: knee hyperextension, tibial external rotation, and increased varus compared with contralateral knee |
| Posterolateral drawer | The patient is supine. The hip is flexed 45 degrees, the knee flexed 80 degrees, and the tibia externally rotated 15 degrees. The foot is fixed, and a posteriorly directed force is applied to the proximal tibia. | Positive findings: lateral tibial external rotation and posterior translation relative to the lateral femoral condyle |
| Tibial external rotation | The patient is either prone or supine. At both 30 and 90 degrees of flexion, the degree of external rotation of the foot relative to the axis of the femur is observed | Positive findings: a side-to-side difference in external rotation of more than 10 degrees Isolated PLC: increased external rotation observed only at 30 degrees Combined PLC and PCL: increased external rotation at both 30 and 90 degrees |
| Posterolateral external rotation | This combines the posterolateral drawer test and the tibial external rotation test. | Isolated PLC: subluxation only at 30 degrees |
| At both 30 and 90 degrees, both posterior translation and external rotation of the tibia are performed. | Combined PLC and PCL: subluxation at both 30 and 90 degrees | |
| Reverse pivot shift | The patient is supine. A valgus force is applied to the tibia while bringing the knee from 90 to 0 degrees with the foot in external rotation. | Positive findings: a palpable shift is observed as the posteriorly subluxated lateral tibial plateau reduces from flexion to extension |
LCL, lateral collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner.
Surgical Techniques
There have been many techniques describing reconstructions of the PLC. However, in this chapter, an allograft semitendinosus, figure-eight reconstruction will be described. A semitendinosus autograft may also be used if not being used for other reconstructive purposes.
Graft Preparation
- The allograft semitendinosus tendon is opened and inspected.
- The graft should be long enough to cut at about 20 cm.
- A No. 2 Ethibond suture is then placed in each free end of the graft in a Krackow-type stitch.
- The looped graft is then passed through a sizing tube to assess the size of the needed femoral socket.
- To prevent desiccation, the graft is then kept moist by utilizing a saline-soaked gauze.
Operative Setup
- Prior to positioning the patient on the operating table, an examination with the patient under anesthesia is performed on both lower extremities to further objectify the degree of laxity and to compare with an exam performed after reconstruction.
- In cases of isolated PLRI, the operative leg is positioned with the heels of both lower extremities at the end of the operating table. The patient is supine. This same position is used in the case of a combined anterior cruciate ligament injury.
- A tourniquet is applied to the proximal thigh.
- A lateral thigh post is positioned at midthigh to aid in diagnostic arthroscopy and is then removed.
- In cases of combined posterior cruciate ligament and PLC injuries, the operative knee is positioned at the table break to allow knee flexion, and the proximal thigh is placed in a leg holder. The nonoperative leg is positioned in a well-leg holder with the hip flexed, abducted, and externally rotated to allow more room about the operative knee. Care is taken to appropriately pad all down points.
- Anesthetic options include general and regional blocks.
Tip: A femoral nerve block is helpful for postoperative pain control.
Incisions
- We prefer not to inflate the tourniquet unless it is needed. However, if the surgeon prefers, the tourniquet is inflated after the extremity is exsanguinated and the knee is flexed.
- Incision 1 is a 3 to 4 cm oblique incision made from the tip of the fibular head proximally. The peroneal nerve can be palpated posterior to the biceps femoris tendon as it dives beneath the fibular head. The course of the nerve should be marked on the skin with a surgical pen. The incision should parallel this course, just proximal to it.
- Careful dissection should then be performed to clearly identify the peroneal nerve. A vessel loop should be placed around the nerve for easy identification throughout the case.
- The anterior and posterior aspects of the fibular head are then cleared.
- A guide pin is placed about 1.5 to 2.0 cm below the tip of the fibular head at its greatest anteroposterior (AP) diameter so as to prevent a fracture. It is then overdrilled with a 6 mm drill.
Tip: Drilling toward a fingertip placed between the posterior aspect of the fibular head and the peroneal nerve allows for palpation of the medial-lateral dimension of the fibular head for better guide pin placement and protects the peroneal nerve.
- A Hewson suture passer is used to pull a No. 5 Tevdek suture through the drill hole so that the looped end is out anteriorly.
- Incision 2, a 3 to 4 cm incision, is then made centered over the lateral femoral epicondyle and in line with the ITB.
- The ITB is then incised in line with the skin incision just above the epicondyle.
Tip: Be careful to split only the ITB and not the joint capsule underneath. This will help if further arthroscopy is to be performed.
- Next, a plane is developed beneath the ITB and biceps femoris tendon, from proximal to distal, along the course of the LCL to exit in incision 1.
Graft Passage
- One end of the semitendinosus graft is passed through the fibular head tunnel from anterior to posterior using the previously placed suture loop. At this point, there is a free end of the graft exiting the anterior and posterior aspect of the fibular head.
- A right-angle clamp, placed from the lateral epicondyle to the fibular head in the plane developed in step 9 in the previous list, is used to pass both free ends of the semitendinosus graft proximally (Fig. 22-3).
- A Beath pin is then placed at the anterior edge of the epicondyle and drilled medially so as to exit the medial femoral condyle.
Tip: The pin should be angled slightly anterior and proximal to avoid the intercondylar notch and any femoral tunnels used for cruciate ligament reconstruction (Fig. 22-4).
- The free ends of the graft are then wrapped around the guide pin, and the knee is moved through a range of motion to check the isometry of the graft. If necessary, changes to the guide pin can be made at this time.

Figure 22-3 The graft being passed with a right-angle clamp beneath the iliotibial band (ITB). The two free ends of the graft are exiting the anterior and posterior aspects of the fibular head. The peroneal nerve is observed with the vessel loop.

Figure 22-4 The guide pin being placed anterior and superior to avoid any tunnels used for cruciate ligament reconstruction. In this case, a double-bundle posterior cruciate ligament (PCL) procedure was also performed, and the sutures used to tension the femoral part of the PCL graft are shown just posterior and inferior to the guide pin.
- Once isometry had been established, a femoral socket is reamed over the Beath pin to a depth of about 30 mm. The diameter of the socket was determined earlier in graft preparation.
- The sutures attached to the free ends of the graft are then placed in the eyelet of the Beath pin and pulled out medially.
- The free ends of the graft are then pulled into the femoral socket. The graft should penetrate the socket at least 20 mm. Care is taken here to place the end exiting the posterior aspect of the fibular head more anterior in the socket and the end exiting the anterior aspect of the fibular head posterior in the socket.
Tip: At this point, if the graft cannot be adequately tensioned within the socket, either the socket needs to be slightly deepened or the graft can be shortened.
- Next, internal tibial rotation and valgus stress are applied to the knee while it is flexed 30 degrees.
- In this position, the graft is tensioned by pulling on the sutures exiting medially. While holding this tension, a bioabsorbable interference screw 1 mm larger than the socket diameter is used to fixate the graft to the lateral epicondyle (Fig. 22-5).
- The knee is then examined to establish that the varus laxity and abnormal external tibial rotation have been corrected.
- Once isometry had been established, a femoral socket is reamed over the Beath pin to a depth of about 30 mm. The diameter of the socket was determined earlier in graft preparation.
Closure
- The ITB is closed with interrupted 0 Vicryl suture. The skin is closed with interrupted 2–0 Vicryl suture followed by a running 4–0 Monocryl suture.
- After dressing the incisions, the tourniquet is released and a thigh-high compressive stocking is placed over the dressing.
- Finally, the knee is placed in either a knee immobilizer or a hinged knee brace locked in extension.
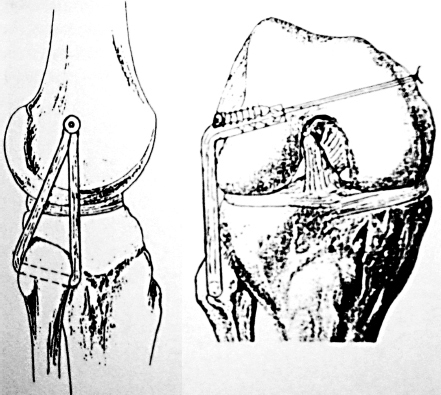
Figure 22-5 A lateral and anteroposterior diagram depicting the graft in place after being secured on the femur with an interference screw. (From Larson RV. Isometry of the lateral collateral and popliteofibular ligaments and techniques for reconstruction using a free semitendinosus tendon graft. Oper Tech Sports Med 2001;9(2);88, with permission.)
Potential Pitfalls
Potential complications associated with the operative treatment of PLC injuries include peroneal nerve injury during both the surgical approach and reconstruction, loss of motion postoperatively, failure of the reconstruction, infection, and painful hardware. Most of these complications can be avoided by vigilant protection of the peroneal nerve throughout the procedure, careful attention to the isometry of the reconstruction, safe and efficient operative and tourniquet time, and clear communication with the patient regarding the postoperative rehabilitation. Preoperative antibiotics should be used in all cases.
Conclusion
The graft described here provides a near isometric reconstruction of the LCL and PFL that will resist posterolateral and varus rotation. This reconstruction can be used to augment the primary repair of acutely injured posterolateral structures or as an isolated procedure. Because injuries to the PLC are relatively uncommon, evaluation of the different surgical techniques to reconstruct this area is difficult. The need continues for randomized, prospective outcome studies concerning these techniques.
References
1 DeLee JC, Riley MB, Rockwood CA, Jr. Acute posterolateral rotatory instability of the knee. Am J Sports Med 1983;11:199–207
2 Hughston JC, Jacobson KE. Chronic posterolateral instability of the knee. J Bone Joint Surg Am 1985;67:351–359
3 Krukhaug Y, Molster A, Rodt A, Strand T. Lateral ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc 1998;6:21–25
4 Harner CD, Vogrin TM, Hoher J, Ma CB, Woo SL. Biomechanical analysis of a posterior cruciate ligament reconstruction. Deficiency of the posterolateral structures as as cause of graft failure. Am J Sports Med 2000;28:32–39
5 Noyes FR, Barber-Westin SD, Roberts CS. Use of allografts after failed treatment of rupture of the anterior cruciate ligament. J Bone Joint Surg Am 1994;76:1019–1031
6 O’Brien SJ, Warren RF, Pavlov H, Panariello R, Wickiewicz TL. Reconstruction of the chronically insufficient anterior cruciate ligament with the central third of the patellar ligament. J Bone Joint Surg Am 1991;73:278–286
7 Andrews JR, Baker CL, Curl WW, Gidumal R. Surgical repair of acute and chronic lesions of the lateral capsular ligamentous complex of the knee. In: Feagin JA, Jr. The Crucial Ligaments: Diagnosis and Treatment of Ligamentous Injuries About the Knee. New York: Churchill Livingstone; 1988;425–438
8 Seebacher JR, Inglis AE, Marshall JL, Warren RF. The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am 1982;64:536–541
9 Wroble RR, Grood ES, Cummings JS, Henderson JM, Noyes FR. The role of the lateral extraarticular restraints in the anterior cruciate ligament-deficient knee. Am J Sports Med 1993;21:257–263
10 Maynard MJ, Deng X, Wickiewicz T, Warren RF. The popliteofibular ligament. Rediscovery of a key element in posterolateral stability. Am J Sports Med 1996;24:311–316
11 Martin IL, Racanelli JA, Drez D. The popliteofibular ligament and its role in posterolateral stability of the knee. Presented at 20th Annual Meeting, American Orthopaedic Society for Sports Medicine, Palm Desert, CA, June 26-29, 1994
12 Staubli HU, Birrer S. The popliteus tendon and its fascicles at the popliteal hiatus: gross anatomy and functional arthroscopic evaluation with and without anterior cruciate ligament deficiency. Arthroscopy 1990;6:209–220
13 Veltri DM, Deng XH, Torzilli PA, Warren RF, Maynard MJ. The role of cruciate and posterolateral ligaments in stability of the knee: a biomechanical study. Am J Sports Med 1995;23:436–443
14 Sidles JA, Larson RV, Garbini JL, Downey DJ, Matsen FA, III. Ligament length relationships in the moving knee. J Orthop Res 1988;6:593–610
15 Larson RV. Isometry of the lateral collateral and popliteofibular ligaments and techniques for reconstruction using a free semitendinosus tendon graft. Oper Tech Sports Med 2001;9:84–90
16 Jakob RP, Warner JP. Lateral and posterolateral rotatory instability of the knee. In: Delee JC, Drez D, Jr, eds. Orthopaedic Sports Medicine: Principles and Practice. Philadelphia: WB Saunders; 1974;1275–1312
17 Baker CL, Jr, Norwood LA, Hughston JC. Acute posterolateral rotatory instability of the knee. J Bone Joint Surg Am 1983;65:614–618
18 LaPrade RF, Terry GC. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med 1997;25:433–438
19 LaPrade RF, Gilbert TJ, Bollom TS, Wentorf F, Chaljub G. The magnetic resonance imaging appearance of individual structures of the posterolateral knee. A prospective study of normal knees and knees with surgically verified grade III injuries. Am J Sports Med 2000;28:191–199
20 Ross G, Chapman AW, Newberg AR, Scheller AD, Jr. Magnetic resonance imaging for the evaluation of acute posterolateral complex injuries of the knee. Am J Sports Med 1997;25:444–448
< div class='tao-gold-member'>









