CHAPTER 12 Posterior Instability of the Shoulder
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. government.
PREOPERATIVE CONSIDERATIONS
The diagnosis and management of posterior instability of the shoulder can be challenging. Posterior instability may be easily overlooked because the initial patient presentation can be confusing; patients present relatively infrequently, and are often referred with a diagnosis other than shoulder instability.1 As always, obtaining an accurate history and diagnosis and accounting for intraoperative pathology are prerequisites for a successful outcome in the treatment of posterior instability of the shoulder.
ANATOMY AND PATHOANATOMY
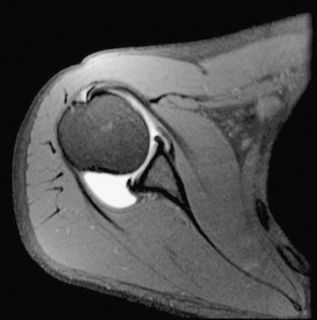
Recent improvements in understanding the anatomy and biomechanics of posterior instability have led to an improvement in clinical diagnosis and recognition of pathology. Posterior shoulder instability can be associated with bony glenoid retroversion, chondrolabral retroversion,2 and decreased posteroinferior capsular size.3 Studies have determined that the quality of the posteroinferior capsule is not as robust as that of the anterior capsule (Fig. 12-1).4
Stabilizers
Dynamic Stabilizers
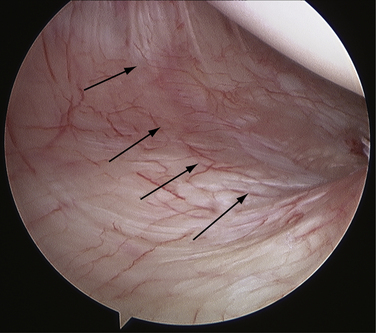
It should be noted that just as in anterior instability, the rotator cuff muscles are the most important stabilizers in posterior shoulder instability. The subscapularis has been identified as the primary dynamic stabilizer preventing posterior translation,5–7 but all the rotator cuff muscles have been shown to be important in providing concavity-compression of the shoulder joint.6–8 Dynamic inferior stability of the shoulder joint is maintained by the supraspinatus and, some believe, by the long head of the biceps.9 The infraspinatus and teres minor serve as posterior compressors.10 A critical component of the examination of a patient who presents with posterior instability is scapular rhythm and control, paying particular attention to the individual rotator cuff muscles, especially the subscapularis (Fig. 12-2).
Static Stabilizers
The primary static stabilizers of the glenohumeral joint are the bony anatomy and capsulolabral ligamentous complex.5,7,10 The most important posterior ligamentous stabilizer in the provocative posterior loading position of internal rotation and forward flexion is the posterior band of the inferior glenohumeral ligament (IGHL) complex. This positions the posterior band of the IGHL (PIGHL) in an anterior-posterior orientation, enabling resistance to posterior subluxation.6 Stretch of the capsule and PIGHL beyond the initial resting length has been implicated as a cause of posterior and multidirectional instability, and is present even without a labral tear.11
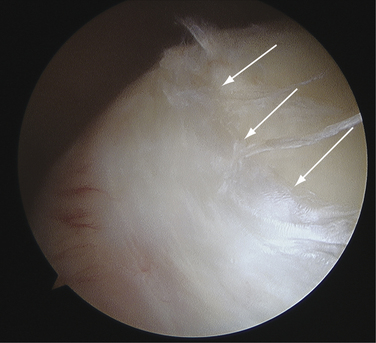
The attachment site of the IGHL is usually well visualized arthroscopically and ranges from 2 to 4 o’clock for the anterior band and 7 to 9 o’clock for the posterior band (Fig. 12-3). In normal shoulder mechanics, the anterosuperior capsule is under tension and there is an obligate simultaneous laxity in the posteroinferior capsule, and vice versa.7 This principle is known as the circle concept of glenohumeral instability. It states that to have shoulder instability, both sides of the capsular mechanism must be disrupted to some extent, although this concept has been questioned by some.12
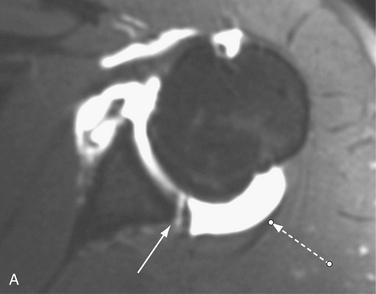
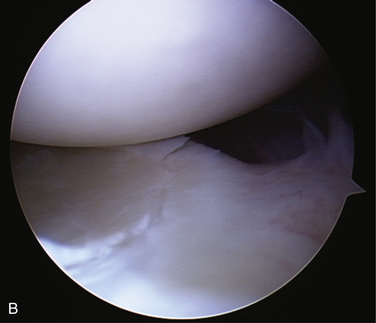
The labrum influences glenohumeral stability by increasing the concavity-compression mechanism of the humeral head in the glenoid socket.7,8,13 The posterior capsule and PIGHL are much less robust and able to sustain much less tensile force than the anterior capsular structures, which underscores the principle that posterior instability is much different from anterior instability.4 A loss of chondrolabral containment (both an increase in bony retroversion and loss of posteroinferior labral height) has been demonstrated in patients with clinically documented posterior instability.2 The principle of chondrolabral containment is important, given the shallow depth of the bony glenoid, which is augmented by the fibrous ring of the glenoid labrum (Fig. 12-4).
Excessive glenoid or humeral retroversion, glenoid hypoplasia, and loss of chondrolabral containment can all contribute to posterior instability.2,7,8,14,15 However, it has not been shown whether glenoid bony changes, such as retroversion, precede or follow the development of posterior instability. In addition, if the ability to maintain negative intra-articular pressure is compromised (effusion, hematoma, repetitive trauma, and loss of capsular constraint), the humeral head will subluxate and also assume a more inferior position with the arm at the side.16
Pathoanatomy
Three broad causative factors have been defined in posterior instability17–19: traumatic, atraumatic, and cumulative microtrauma.
The most frequent cause of posterior shoulder instability is repetitive microtrauma to the posteroinferior shoulder complex. Sporting activities that involve repetitive loading of the shoulder in front of the body, such as repetitive bench press lifting, overhead weight lifting, rowing, swimming, and blocking linemen in football, are commonly implicated. In these activities, the shoulder is placed in a flexed, adducted, internally rotated position, with a concomitant posterior load resulting in stretch and injury of the posterior band of the IGHL17,18,20,21 and the posterior labrum. The labrum and capsule are repetitively injured, often present in conjunction with a dynamic dysfunction of the shoulder (poor scapulothoracic mechanics).
Tears of the labrum, which can develop after acute trauma or repetitive microtrauma, are important to recognize, because those with labral pathology have demonstrated uniformly good results with surgical treatment.20–23 In the cumulative microtrauma model, a Kim lesion may develop. This is thought to occur with cumulative rim loading secondary to persistent shoulder subluxation or microtrauma. This pathologic process leads to a loss of chondrolabral containment, with subsequent development of posterior labral marginal cracks and undermining of the labrum or partial avulsions of the glenoid labrum (Fig. 12-5).24
HISTORY AND PHYSICAL EXAMINATION
The most frequent complaint in patients with posterior shoulder instability is shoulder pain that is often accompanied by decreased athletic performance and loss of strength.17,20,23,25 Pain is often described as generalized throughout the shoulder or at the deep posterior aspect of the shoulder. Subjective apprehension in posterior instability is uncommon.19 When questioned, patients will describe a dramatic reduction in the amount of their bench press weight, inability to do push-ups, and overall poorer athletic performance. In the relatively young patient (younger than 35 years) who presents with multiple vague complaints of shoulder pain in the absence of other diagnoses, the diagnosis of posterior instability is often present.
A unique finding in posterior instability is that patients may be able to subluxate “voluntarily” their glenohumeral joint posteriorly. There are two types of voluntary glenohumeral instability—voluntary positional and voluntary muscular.26 Voluntary positional instability is common in posterior instability and is defined by subluxation in a provocative position (flexion, adduction, and internal rotation). Voluntary muscular instability occurs with the arm in an adducted (non–position-dependent) position. Patients with voluntary positional instability who can positionally reproduce their instability should not be excluded from surgical treatment27 and should not be associated with voluntary willful instability.
A comprehensive physical examination is essential for a patient with suspected posterior instability of the shoulder. Both shoulders should be examined, observing any obvious dislocation, asymmetry, abnormal motion, muscle atrophy, swelling, and scapular winging and tracking. The asymptomatic shoulder may be examined first to gain patient confidence and relaxation. The mainstay of diagnosis remains a finding of symptomatic posterior instability in the office setting, which may be confirmed by a translation examination under anesthesia.28
Although an increase in external rotation and mild loss of internal rotation may be observed, range of motion testing in patients with posterior is usually normal and symmetrical.18 Tenderness to palpation at the posterior glenohumeral joint line is common.26
Provocative maneuvers allow a determination of the direction and degree of instability. Common posterior instability tests include the jerk test,29 posterior stress test,30 Kim test,31 and load and shift test.32 The jerk test is performed while the examiner stands next to the affected shoulder. The elbow is grasped in one hand, and the distal clavicle and scapular spine in the other. With the arm in flexion and internal rotation, the flexed elbow is pushed posteriorly while the shoulder girdle is pushed anteriorly. While these forces are applied, the shoulder is abducted. A sudden jerk associated with pain occurs as the subluxated humeral head relocates into the glenoid fossa (Fig. 12-6).
The Kim test is also helpful for diagnosing posterior instability.31 This test is performed with the patient seated and the arm in 90 degrees of abduction. As the arm is passively elevated to 45 degrees of forward flexion, the examiner applies an axial load to the elbow while a downward and posterior force is applied to the upper arm. Pain and posterior subluxation signify a positive test. Combining the Kim and jerk tests has been shown to have 97% sensitivity for posterior instability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree