20
Posterior Cruciate Ligament Reconstruction Using the Tibial Inlay Technique
Posterior cruciate ligament (PCL) injuries and reconstruction have received increased attention over the past two decades and have become the focus of much ongoing research. For many years, the challenge of repairing the PCL has baffled orthopaedic surgeons. Although the PCL is an important stabilizer to posterior translation of the knee, the lack of success with reconstruction has made it a less popular procedure than repair of the anterior cruciate ligament (ACL) and other knee structures. Currently, many of the surgical techniques for reconstruction of the PCL do not consistently yield reproducibly good results. Techniques that have shown the most promise are those that focus on re-creating the normal anatomy of the PCL and may yield the best long-term results.
The PCL is the primary restraint to posterior tibial translation.1, 2 Along with the ACL, it is responsible for the “screw home” mechanism of the knee (tibial external rotation during the final 15 degrees of knee extension).3 Hughston et al4 found the PCL to be extremely important, noting that it is the “fundamental stabilizer of the knee.” This chapter focuses on the evaluation and treatment of the PCL and on reconstruction using the tibial inlay technique.
Surgical Indications and Other Treatment Options
Anatomically, the PCL lies within the capsule of the knee joint and can be viewed arthroscopically, but technically it is extraarticular, as it lies within its own synovial sheath. The PCL originates at the posterolateral aspect of the medial femoral condyle and inserts centrally on the posterior aspect of the tibia in a depression 1 cm distal to the tibial plateau. It has an average length of 38 mm and width of 13 mm5 and fans out at its origin and insertion. The ligament consists of several portions. The anterolateral portion, which is tight in flexion, is the thickest, longest,6 and strongest.7 The posteromedial portion is thinner and shorter, and is tight in extension.5 The anterior and posterior meniscofemoral ligaments of Humphry and Wrisberg, respectively, are variable in their presences. They arise from the posterior horn of the lateral meniscus and insert on the medial femoral condyle with the PCL. The vascular supply to the PCL is the middle genicular artery, a branch of the popliteal artery.8 The nerve supply to the PCL is from the popliteal plexus, which provides pain sensation, pressure, and even proprioception.9
Biomechanically, the PCL is said to have twice the strength of the ACL,10 an assertion that was used to explain why the ACL is more commonly injured. Tensile testing of the PCL has actually revealed the load failure to be only marginally greater than the ACL.11 Butler et al1 showed that the PCL is the primary restraint to posterior tibial translation in more than 30 degrees of knee flexion. The amount of strain in the PCL varies throughout its course but appears to be greatest in the anterior portion. Covey and Sapega12 showed that PCL tension appears to be altered by quadriceps force and rotation. Contact pressure studies have shown that increased pressure (ultimately leading to chondrosis) occurs within the medial femoral condyle and patellofemoral compartment of the PCL-deficient knee.13, 14 As a result of the anatomic and biomechanical complexity of the PCL, re-creation of this ligament via surgical reconstruction has proven to be quite a difficult task.
Preoperatively, the diagnosis of PCL tears depends on a combination of a high index of suspicion, good history taking, and a careful physical examination. The common mechanisms of injury include high-energy posterior impact to the anterior tibia of a flexed knee (e.g., dashboard injury from a motor vehicle accident) and forceful hyperextension or hyperflexion of the knee (e.g., during athletic activity15). On the physical exam, the “gold standard” test for diagnosis of a PCL tear is the posterior drawer test (which is 90% sensitive and 99% specific),16 and should be performed with the patient in neutral rotation with the knee in 90 degrees of flexion.17 Other useful tests for determining PCL pathology include the posterior sag test, the quadriceps active test, the prone drawer test, the dynamic posterior shift test, and the posteromedial pivot shift test for posteromedial instability. Tests for posterolateral corner injuries commonly associated with PCL tears include asymmetric tibial external rotation, reversed pivot shift, and the posterolateral drawer tests for posterolateral instability.
Radiographically, plain films should be obtained to rule out avulsion or medial tibial plateau fractures, as well as the presence or absence of arthrosis in the patellofemoral and tibiofemoral joints in cases of chronic PCL deficiency. Stress views may also be helpful for diagnosis and may allow objective measurement of surgical results.18, 19 Magnetic resonance imaging (MRI) is also extremely helpful and is nearly 100% sensitive and specific in identifying PCL tears,20 but should be used as an adjunct to clinical assessment rather than independently to diagnose PCL tears.
Direct arthroscopic examination and visualization of the PCL (after examination under anesthesia) can provide the confirmation for the diagnosis of PCL tears. Additional evidence of PCL pathology includes the presence of bony avulsions, hemorrhage, ACL pseudolaxity (as the tibia is subluxed posteriorly) (Fig. 20-1), degenerative changes in the articular surfaces of the medial compartment and patellofemoral joint, and alteration of the contact points between the normal articular surfaces of the tibia and femur.21
Choosing a treatment option for PCL injuries continues to be controversial.29 Historically, nonoperative management has been preferred over operative treatment, but recent studies have shown that patients with this treatment have a high risk of developing late arthrosis.22 Conservative management usually consists of early postinjury splinting with the knee in full extension, followed by early motion and quadriceps strengthening exercises (avoiding hamstring strengthening), and protecting the knee from posterior tibial translation. Currently, nonoperative treatment is indicated in cases of isolated, asymptomatic PCL tears in patients with mild to moderate laxity. Operative treatment is preferred in cases of severe posterior laxity, combined ligament injury, and bony avulsion fractures, and in patients with chronic, symptomatic posterior laxity. The site of injury to the PCL is important in selecting the optimal treatment option. For complete midsubstance tears, we recommend the tibial inlay technique for reconstruction. Primary repair of the ligament is indicated for avulsion fractures from either of the insertion sites. Primary repair of midsubstance injuries has resulted in poor outcomes and is not recommended. Tibial avulsions are more common and require a posterior approach to the knee for reduction and fixation.23, 24 For larger avulsion fragments, anatomic reduction and primary repair can be performed with lag screws, whereas smaller fragments may be repaired with suture fixation through drill holes. We prefer the tibial inlay technique to arthroscopic “transtibial” techniques because of less laxity with cyclic loading, lower graft forces,25 and less vascular risk.
Surgical Techniques
The goal of surgical reconstruction of the PCL is the accurate restoration of normal anatomy. Reconstructing only the anterolateral portion of the PCL is both practical and acceptable as this is the most important anatomic and biomechanic component. Choosing which type of graft to use is also an important concern. Autografts using bone-patellar tendon-bone or quadriceps tendon, or allografts using Achilles’ tendon or bone-patellar tendon-bone may be used depending on the circumstances of each specific case. Consideration should be given to the necessary length of the graft, bony fixation at the ends of the graft, and other issues. For tibial inlay PCL reconstruction, patellar tendon grafts are used most often because it has both adequate length and allows bony fixation on both ends of the graft. In the past, arthroscopic anterior techniques have been used to reconstruct the PCL, but due to the limited exposure of the PCL fossa, this technique can lead to sharp graft angles as it exits the tibial tunnel. This has been referred to as the killer turn and may be associated with late graft failure.26
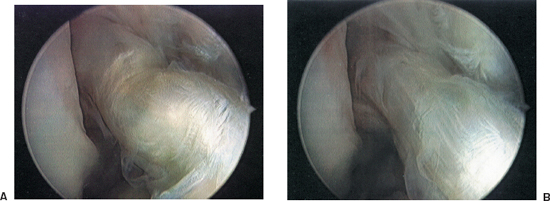
Figure 20-1 Anterior cruciate ligament (ACL) pseudolaxity. (A) Arthroscopic view of the posterior cruciate ligament. (B) Normal appearance of the ACL after an anterior drawer is performed.
Tibial Inlay Technique
Recently, the tibial inlay technique has been developed, which has resulted in decreased graft bending angles and led to improved patient outcome following PCL reconstruction.27, 28 This technique, originally described by Berg,28 involves a posterior approach to the knee and has been adapted from methods used to perform primary fixation of PCL tibial avulsion fractures.24
The patient should be positioned on the operating room table in the lateral decubitus position, with the operative leg up (Fig. 20-2). From this position, a posterior approach can be made directly, and the hip can be abducted, flexed to 90 degrees, and externally rotated, with the foot on the table to perform arthroscopy, graft harvest, femoral tunnel placement, and graft passage. A commercially available leg holder, commonly used for total knee arthroplasty, can be helpful. The patient is examined under anesthesia prior to positioning. A tourniquet is placed on the proximal thigh (although rarely used), and the leg is prepped and draped in the standard sterile fashion.
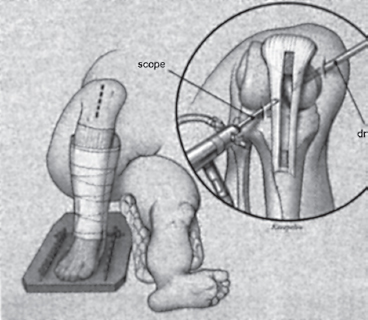
Figure 20-2 Positioning of the patient. After examina tion under anesthesia, the patient is placed in the lateral decubitus position with the affected leg up. The opposite leg remains extended, and care is taken to ensure it is adequately padded. A commercially available leg holder is used, and the leg is abducted and externally rotated for arthroscopy, graft harvesting, and femoral tunnel place ment. After femoral tunnel placement, the leg is extended and placed in neutral rotation on a padded Mayo stand for the posterior approach.
A central anterior knee incision is then made, about 6 to 8 cm long, sufficient to harvest a patellar tendon autograft. An 11 mm bone-patellar tendon-bone graft is harvested from the central third of the patellar tendon, being careful to harvest a rectangular or trapezoidal bone plug from the tibial side. The tibial portion of the graft is fashioned with a flattened surface and prepared to accept a 4.5 mm bicortical screw by drilling and tapping. The patellar portion of the graft should be contoured in a cylindrical fashion and the tip sculpted in a “bullet” shape to facilitate graft passage. Perpendicular sutures are placed in this end to avoid suture cutout during graft fixation.
Standard arthroscopy should then be performed to verify PCL deficiency (it may be done prior to graft harvesting if there is any question), as well as any other intraarticular pathology, and to identify landmarks for reconstruction. The PCL stump is debrided, and preparations for the femoral tunnel are finalized. A commercially available femoral drill guide is then placed into the anterior portion of PCL footprint at its femoral insertion. The starting point is centered on the medial cortex of the medial femoral condyle. The entry point is more proximal to preserve subchondral bone and reduce the risk of avascular necrosis of the medial femoral condyle. The guide tip should be placed 8 mm from the medial femoral condyle articular surface at the 11 or 1 o’clock position and subsequently overdrilled with a cannulated drill bit sized appropriately for the graft. The posterior aspect of the femoral tunnel is rasped to prevent graft abrasion. An 18-gauge guidewire or commercially available graft passer is then introduced into the femoral tunnel and the posterior aspect of the knee joint to facilitate graft passage.
The patient is then repositioned with the operative knee extended and the lower leg placed on a padded Mayo stand (Fig. 20-3A). We prefer the posterior approach similar to that described by Burks and Schaffer.24 A horizontal incision is made in the crease of the popliteal fossa (Fig. 20-3B). The interval between the medial head of the gastrocnemius and the semimembranosus is developed. Lateral retraction of the gastrocnemius provides access to the posterior capsule of the knee and simultaneously protects the neurovascular structures of the popliteal fossa. The fascial incision is then extended distally and medially. If necessary, the medial head of the gastrocnemius can be partially released to provide additional exposure, but this is rarely, if ever, necessary. The surgeon can then palpate both the posterior tibial sulcus and the prepositioned wire loop. A vertical capsular incision is then made to expose the posterior knee joint and retrieve the wire loop.
Muscle fibers of the popliteus are split, and the posterior cortex of the tibia is exposed. It is helpful to palpate the PCL sulcus, which lies between two ridges, before exposing the back of the tibia completely. With the use of an osteotome, burr, and tamp, a unicortical trough is made at the site of tibial insertion of the PCL to match the tibial side of the graft prepared earlier. The graft is inlaid into the trough, and the trough or bone plug is adjusted to allow the plug to fit snugly into the window, flush with the back of the tibia. The graft is then provisionally fixed to the back of the tibia with a staple that is left prominent for easy removal, if adjustment becomes necessary.
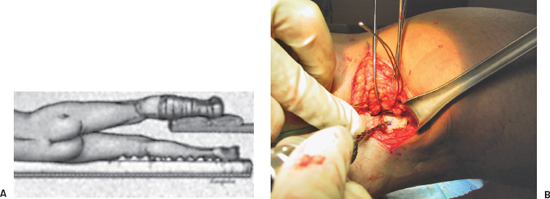
Figure 20-3 Posterior incision. (A) A horizontal incision is made in the crease of the popliteal fossa. After dissection of the fascia overlying the gastrocnemius muscle, the interval between the medial head of the gastrocnemius and semimembranosus is identified. (B) Retraction of the medial head of the gastrocnemius laterally with Steinmann pins exposes the popliteus muscle belly. The neurovascular structures are then protected. The graft is inlayed into a trough made in the posterior aspect of the tibia.
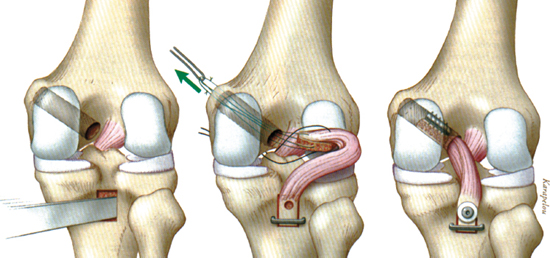
Figure 20-4 Graft passage. The inlay graft is provisionally fixed with a staple, and the proximal end is pulled into the joint by using an 18-gauge wire. A suture is passed out the front of the knee and is used to “toggle” the graft to assist in guiding the graft through the femoral tunnel. The graft is then secured with a bicortical screw from posterior to anterior. Next, the graft is tensioned, an anterior drawer force is applied, and the femoral side is fixed with a 9 mm interference screw. Double fixation may be performed by supplementing the graft with a suture over post technique.
The prepositioned 18-gauge wire or graft passer is then used to pass the patellar end of the graft through the notch and into the femoral tunnel (Figs. 20-3B and 20-4). This maneuver sometimes requires two steps. In the first step, the graft is passed into the notch by passing the sutures from the bony end of the graft out the anteromedial portal. A second loop is passed from the femoral tunnel out the same portal and is used to pull the bone plug up into the tunnel as a second step. It is helpful to place multiple sutures in the patellar bone block, with sutures placed near the tapered end of the block passed into the femoral tunnel and sutures near the opposite end of the bock passed through an anteromedial portal. In this manner, the graft can be manipulated into the femoral tunnel with one set of sutures and “toggled” to line up with the tunnel with the sutures retrieved through the anteromedial portal.
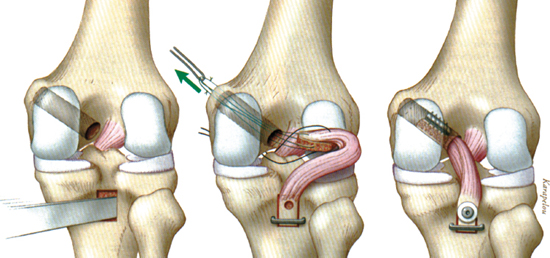
Figure 20-5 Anteroposterior (A) and lateral (B) radiograph demonstrating graft and hardware placement.
The knee is then passively taken through a full range of motion, any kinks in the graft are eliminated, and the stability of the graft is assessed. The location of the bone plug-tendon junction is then carefully evaluated. It is our goal to have this junction right at the intraarticular margin of the femoral tunnel. The graft is tensioned, and the tension is assessed. If the bone plug goes too far into the femoral tunnel, the tibial trough/inlaid bone block is moved distally.
The tibial bone block is then secured using a bicortical 4.5 mm cortical screw and flat washer placed through the predrilled hole in the graft and lagged to the anterior cortex of the tibia. We frequently supplement this with a staple, usually placed distal to the screw. After ensuring that the graft is fully in the femoral tunnel, this side of the graft is fixed with a 9 20 mm interference screw. The knee is flexed 70 to 80 degrees, anterior drawer force is applied to the tibia to reproduce the stepoff, and tension is placed on the sutures exiting the femoral tunnel. A posterior drawer test confirms that PCL stability has been restored. Additional fixation may be used with a screw and post technique.
Bone graft, which is saved during graft preparation and during femoral tunnel drilling, is packed into the patella and, if enough remains, into the tibial tubercle. Wounds are closed in the standard fashion, and a sterile dressing is applied. Intraoperative radiographs are obtained before the patient leaves the operating room to ensure that graft and hardware placement is appropriate (Fig. 20-5).
Postoperatively, the operative knee is braced in extension with support to the posterior tibia provided to prevent posterior translation. Weight bearing as tolerated with crutch walking is initiated as early as the first day postoperatively. Passive range of motion in the prone position usually with the assistance of another person is stressed early during rehabilitation. Quadriceps strengthening is emphasized only, whereas hamstring rehabilitation is delayed. The patient should be allowed to return to full activities 9 to 12 months following surgery provided the knee is stable, full range of motion is returned, and quadriceps strength is symmetric to the contralateral leg.
Tips, Tricks, and Pitfalls
Preoperative planning is a critical aspect to successful reconstruction of the PCL. If there is other associated ligamentous damage, especially to the posterolateral corner, reconstruction should be considered simultaneously with PCL reconstruction. If allograft is utilized, care should be taken to ensure that the donor patella tendon graft is approximately the same size as the recipient’s patella tendon. Steinmann pins are used to assist in retraction of the medial head of the gastrocnemius. Graft passage can sometimes be very challenging, so a generous arthrotomy should be made to assist in the graft passage. The patellar bone block should be fashioned in a smooth, small (18 to 20 mm), and bullet shape. An extra suture may be passed out of the anterior portal to help “toggle” the graft. After securing the tibial side of the graft and prior to proximal fixation, the knee should be cycled in flexion and extension to tension the graft. Prior to wound closure, intraoperative anteroposterior and lateral radiographs should be taken to ensure proper placement of the hardware.
The most serious complication of the surgery is injury to the neurovascular structures during tibial tunnel drilling and graft passage. Other potential complications are infection, loss of motion, medial femoral condyle osteonecrosis, anterior knee pain, and painful hardware. The most common complication to surgery is residual laxity, which we believe occurs more commonly following arthroscopic-assisted PCL reconstruction than following tibial inlay reconstruction.25
Conclusion
Although uncommon, PCL injuries result in an unstable knee and must be diagnosed early to achieve optimal results and avoid the possible sequela of chronic PCL deficiency, including the development of osteoarthrosis. Once diagnosed, repair or reconstruction appears to be the most appropriate treatment of complete PCL tears. Primary repair yields the best results for avulsion injuries. In chronic PCL laxity, reconstruction via the tibial inlay procedure appears to be the best treatment option in our hands. This technique has yielded acceptable results although not as good as those seen with ACL reconstruction. Through further research into PCL anatomy and reconstruction techniques, we hope improvements in grafts, technique, diagnosis, and preoperative and postoperative care will ultimately provide more improved results.
References
1 Butler DL, Noyes FR, Grood ES. Ligamentous restraints to antero-posterior drawer in the human knee: a biomechanical study. J Bone Joint Surg Am 1980;62:259–270
2 Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee: a biomechanical study. J Bone Joint Surg Am 1987;69:233–242
3 Kannus P, Bergfeld J, Jarvinen M, et al. Injuries to the posterior cruciate ligament of the knee. Sports Med 1991;12:110–131
4 Hughston JC, Bowden JA, Andrews JA, et al. Acute tears of the posterior cruciate ligament: results of operative treatment. J Bone Joint Surg Am 1980;62:438–450
5 Girgis FG, Marshall JL, Al Monarem ARS. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res 1975;106:216–231
6 Harner CD, Xerogeanes JW, Livesay GA, et al. The human posterior cruciate ligament complex: an interdisciplinary study. Ligament morphology and biomechanical evaluation. Am J Sports Med 1995;23:736–745
7 Race A, Amis AA. The mechanical properties of the two bundles of the human posterior cruciate ligament. J Biomech 1994;27:13–24
8 Scapinelli R. Studies on the vasculature of the human knee joint. Acta Anat (Basel) 1968;70:305–331
9 Kennedy JC, Alexander IJ, Hayes KC. Nerve supply of the human knee and its functional importance. Am J Sports Med 1982;10:329–333
10 Kennedy JC, Hawkins RJ, Willis RB, et al. Tension studies of human knee ligaments: yield point, ultimate failure, and disruption of the cruciate and tibial collateral ligaments. J Bone Joint Surg Am 1976; 58:350–355
11 Prietto MP, Bain JR, Stonebrook SN, et al. Tensile strength of the human posterior cruciate ligament (PCL). Trans Orthop Res Soc 1988;13:195
12 Covey DC, Sapega AA. Injuries of the posterior cruciate ligament. Current concepts review. J Bone Joint Surg Am 1993;7SA:1376–1386
13 Skyhar MJ, Warren RF, Ortiz GJ, et al. The effects of sectioning of the posterior cruciate ligament and the posterolateral complex on the articular contact pressures within the knee. J Bone Joint Surg Am 1993;7A:694–699
14 MacDonald PB, Miniaci A, Fowler PJ, et al. Biomechanical analysis of joint contact forces in the posterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc 1996;3:252–255
15 Fowler PJ, Messieh SS. Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med 1987;15:553–557
16 Miller MD, Johnson DL, Harner CD, et al. Posterior cruciate ligament injuries. Orthop Rev 1993;22:1201–1210
17 Bergfeld JA, McAllister DR, Parker RD, Valdevit AD, Kambic H. The effects of tibial rotation on posterior translation in knees in which the posterior cruciate ligament has been cut. J Bone Joint Surg Am 2001;83-A:1339–1343
18 Puddu G. Radiographic view for PCL injuries. Instructional Course Lecture, Western Pacific Orthopaedic Association Meeting, Taipei, Taiwan, November 1997
19 Hewett TE, Noyes FR, Lee MD. Diagnosis of complete and partial posterior cruciate ligament ruptures. Stress radiography compared with KT-1000 arthrometer and posterior drawer testing. Am J Sports Med 1997;25:648–655
20 Gross ML, Grover JS, Bassett LW, et al. Magnetic resonance imaging of the posterior cruciate ligament: clinical use to improve diagnostic accuracy. Am J Sports Med 1992;20:732–737
21 Fanelli GC, Giannotti BF, Edson CJ. The posterior cruciate ligament arthroscopic evaluation and treatment. Current concepts review. Arthroscopy 1994; 10:673–688
22 Dejour H, Walch G, Peyrot J, et al. The natural history of rupture of the posterior cruciate ligament. Fr J Orthop Surg. 1988;2:112–120
23 Meyers MH. Isolated avulsion of the tibial attachment of the posterior cruciate ligament of the knee. J Bone Joint Surg Am 1975;57:669–672
24 Burks RT, Schaffer JJ. A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop Relat Res 1990;254:216–219
25 Bergfeld JA, McAllister DR, Parker RD, Valdevit AD, Kambic HE. A biomechanical comparison of posterior cruciate ligament reconstruction techniques. Am J Sports Med 2001;29:129–136
26 Miller MD, Bergfield JA, Fowler PJ, et al. The posterior cruciate ligament injured knee. Principles of evaluation and treatment. Instr Course Lect 1999;48:199–207
27 Miller MD, Harner CD, Koshiwaguchi S. Acute posterior cruciate ligament injuries. In: Fu FH, Harner CD, Vince KG, eds. Knee Surgery. Baltimore: Williams & Wilkins; 1994:749–767
28 Berg EE. Posterior cruciate ligament tibial inlay reconstruction. Arthroscopy 1995;11:69–76
29 Miller MD, Olszewski AD. Posterior cruciate ligament injuries. New treatment options. Am J Knee Surg 1995;8:145–154
< div class='tao-gold-member'>









