Plantar Heel
Jeffrey S. Boberg
Damien M. Dauphinée
D. Scot Malay
William Harris IV
Calcaneodynia is a disorder that is usually amenable to conservative care measures, but in some patients it can be both frustrating and difficult to treat. Patients often present with episodic pain, often poststatic, with increasing intensity and duration over months to years. The diagnosis is based upon the history and physical exam, which yields areas of palpatory tenderness to the plantar and medial heel as well as proximal arch. No other consistently reliable objective diagnostic tests are available. Response to different treatment modalities can vary greatly from patient to patient or in the same patient from one visit to the next. The condition is often referred to as plantar fasciitis, but this as an etiology is now being questioned and the exact cause is unclear. This can make treatment of the nearly 2 million patients who present to physician offices with heel pain every year a challenging task, especially given the diversity in treatment protocols from one doctor to another. The conceptual approach to conservative and surgical care for this condition is still evolving.
FUNCTIONAL ANATOMY
Weight-bearing and ambulation force the soft tissues in the heel to react to compressive and tractional forces at the same time. Understanding the anatomic relationship of structures in this tightly packed area of the foot can help the practitioner to understand the possible causes of heel pain. Compression of the heel pad occurs at the beginning of each weight-bearing period, followed by traction on both the plantar and posterior calcaneus during the middle to late stance periods. Depending on body structure and activity, those forces may exceed tissue tolerances and may create painful and disabling symptoms.
At the anterior aspect of the calcaneal tuberosity are the attachments of the plantar fascia, or plantar aponeurosis, and the intrinsic musculature of the foot. These structures extend the length of the longitudinal arch and envelop the metatarsophalangeal joints inserting on the phalanges (1). The plantar structures are tightened whenever the metatarsophalangeal joints are dorsiflexed, thus raising the longitudinal arch of the foot. The secondary effect is traction on the calcaneal origins of the plantar intrinsic musculature (1).
The plantar fascia is a broad, dense band of longitudinally arranged collagen fibers that begins as a thick mass attached to the anterior aspect of the calcaneal tuberosity (2). The central band spreads into a broad sheet as it extends distally and divides into five digital bands at the metatarsophalangeal joints (2). Each digital band divides to pass on either side of the flexor tendons and inserts dorsally into the periosteum at the base of the proximal phalanges. Fibers of the plantar fascia blend with the dermis, transverse metatarsal ligament, flexor tendon sheaths, and other adjacent ligamentous structures (1,2). The central portion of the plantar fascia is continuous with the medial and lateral portions. At these junctions are two strong intermuscular septa that are broader distally than proximally (2).
The lateral portion of the plantar fascia is found superficial to the abductor digiti minimi muscle (2,3). This portion of the fascia is thicker proximally and forms a strong band between the lateral process of the tuberosity of the calcaneus and the base of the fifth metatarsal bone. The lateral band of the plantar fascia is continuous with the central portion medially and with the fascia on the dorsum of the foot laterally (2) (Fig. 39.1).
The medial portion of the plantar fascia lies superficial to the abductor hallucis muscle and is thin. It is continuous with the central portion of the plantar fascia laterally and with the fascia on the dorsum of the foot medially. This medial portion is also attached to the flexor retinaculum (2).
The plantar fascia itself is largely inelastic. This inelasticity means that tension experienced on one end is immediately transmitted to the other. As the foot moves through midstance to toe-off, the metatarsophalangeal joints are dorsiflexed, thus creating tension on both intrinsic muscle and the plantar fascial origins at the calcaneal tuberosity. Simultaneously, additional tension is created by the soleus as it pulls the heel posteriorly, stabilizing the ankle for forefoot stance (4).
No natural bursae exist beneath the plantar surface of the heel. Adventitial bursae may exist, but they are uncommon. Barrett et al (5), in a dissection of 200 cadaver legs, were able to identify only a single inferior calcaneal bursa.
MUSCLES
The abductor hallucis lies along the medial border of the foot along the instep and takes its origin at the inferior and medial aspects of the posteromedial calcaneal tuberosity; it inserts into the medial aspect of the base of the proximal phalanx of the great toe. Its origin is also invested in the deep surface of the plantar fascia, the posterior end of the medial intermuscular septum, and the flexor retinaculum, or laciniate ligament, which invests the muscle (6).
The flexor digitorum brevis lies in the middle of the plantar aspect of the foot, immediately deep to the central portion of the plantar fascia. Many of its fibrous attachments originate from the deep side of the plantar fascia (2). The flexor digitorum brevis muscle originates from the medial process of the tuberosity of the calcaneus, as well as from the central portion of the plantar fascia and from the intermuscular septa between it and the adjacent muscles (2).
The abductor digiti minimi lies along the lateral border of the foot, with its medial margin next to the lateral plantar vessels and nerves. It originates from a broad area that begins at the lateral process, includes the posterolateral calcaneal tuberosity, and extends to the distal aspect of the posteromedial tuberosity of the calcaneus slightly anterior to the origin of the flexor digitorum brevis. It also has attachments to the deep side of the plantar fascia and to the intermuscular septum between it and the flexor digitorum brevis muscle. It inserts with the flexor digiti minimi brevis into the lateral part of the base of the fifth toe (2).
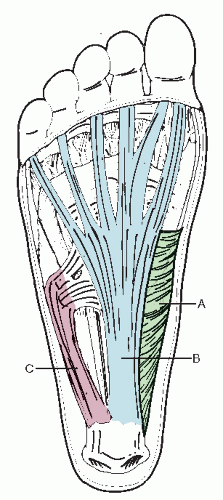 Figure 39.1 The anatomy of the plantar fascia. The thin medial band (A) overlies the abductor muscle belly. The thick central (B) and lateral (C) bands are easily identified. |
The only muscle in the second layer of intrinsics that originates from the calcaneus is the quadratus plantae. It arises from two heads separated by the long plantar ligament. The larger muscular medial head arises from the concave surface of the plantar calcaneus. The lateral head is flat and tendinous, and it arises from the lateral border of the calcaneus, distal to the lateral process of the tuberosity as well as from the long plantar ligament. The quadratus plantae muscle helps to straighten the pull of the flexor digitorum longus tendon by inserting deep to and along the lateral margin of the tendon of the flexor digitorum longus muscle (2).
TIBIAL NERVE AND ITS BRANCHES IN THE FOOT
The tibial nerve is the larger of the two terminal divisions of the sciatic nerve and is composed of fibers from the ventral portions of L4, L5, and S1, S2, and S3. At the heel, the medial calcaneal branches perforate the laciniate ligament and innervate the skin of the heel and medial side of the sole of the foot (2). The tibial nerve then divides into the larger medial plantar nerve and the lateral plantar nerve. The medial plantar nerve follows the medial plantar artery and passes deep to the abductor hallucis and medial to the flexor digitorum brevis muscle, to enter the plantar vault through the porta pedis (2).
The lateral plantar nerve also enters the plantar vault through the porta pedis. However, before this, it gives off the “first branch,” discovered in 1963 by Tanz (6), who noticed a deep calcaneal branch at the time of a heel spur resection. He further detailed a cadaveric dissection of this nerve as it passes beneath the tuber calcanei and under the plantar fascia, where it bends laterally. In 1981, Przylucki and Jones (7) dissected a similar nerve and found it to be a motor branch to the abductor digiti quinti muscle. They described this nerve as a branch of the lateral plantar nerve that passed medially to laterally beneath the heel.
The lateral plantar nerve then courses distally with the lateral plantar artery to the lateral side of the foot, to lie between the flexor digitorum brevis muscle and the quadratus plantae (2). The nerve may also course proximally enough that it is at risk during plantar fasciotomy surgery.
HEEL SPUR
Over the years, many authors have described the classic heel spur (8,9,10 and 11). The heel spur or calcaneal spur is an osteophytic outgrowth anterior to the medial calcaneal tuberosity that usually extends its entire width or about 2.0 to 2.5 cm (11). This condition most often exists without producing symptoms, although in some selected patients it may become a source of symptoms.
Although some surgeons believe that the apex of the spur lies in the origin of the plantar fascia, McCarthy and Gorecki (8) countered that the spur lies in the origin of the flexor digitorum brevis muscle, superior to the plantar fascia. Furthermore, they asserted that the origin of the flexor digitorum brevis muscle, the quadratus plantae, the long plantar ligament, the abductor hallucis muscle, and the abductor digiti minimi muscle are all sites of potential spur formation.
Foreman and Green studied cadaveric specimens and found that the plantar fascia “slings underneath the calcaneus and remains plantar to the spur at the calcaneal tuberosities. The flexor digitorum brevis lies above the aponeurosis and attaches into the apex of the spur at the medial tuberosity” (9). They also believed that the abductor hallucis origin attaches at the apex of the spur and contributes to its formation. From their cadaveric specimen studies, these investigators found that the abductor digiti minimi and quadratus plantae origins were lateral to and superior to the spur, respectively.
Graham stated that the plantar fascia and the flexor brevis muscle attach to the calcaneal tubercle proximal to where technetium-99m scans show increased uptake His belief was that the intrinsics pull on the tubercle and eventually collapse the anterior lip of the tubercle. Graham’s contention is that the “spurs” seen on radiographs are a “manifestation of the healing effort and reflect a layering out of the calcification on top of the flexor muscle and not a traction spur as commonly believed” (12).
Many authors believe that the constant pulling of the plantar fascia causes an inflammatory process. The constant strain results in periostitis followed by osteogenesis (13,14 and 15). Histologic studies have demonstrated that the periosteum displays “low-grade chronic inflammation as evidenced by thickening and edema, proliferation of fibroblasts, and round cell infiltration.” In addition, investigators noted that the bone spur itself showed “fibrosis of marrow tissues, small areas of necrosis, hyaline or gelatinous degeneration, and at places, proliferation of fibroblasts and sclerosis of cortical bone” (16).
ETIOLOGY
Investigators have stated that of all adult foot complaints, 15% result from heel pain (8). Over the years, many causes of heel
pain have been proposed. In the 1930s, gonorrhea, syphilis, tuberculosis, and streptococcal infections were commonly believed to be major causes (16). Later, many of the theories on gonorrhea were discredited (17,18). Hauser (14) surmised that the heel spur acts like a truss, pointing down into the muscle belly and causing pain. Some investigators postulated that the subcalcaneal fat pad loses its compressibility secondary to thinning and loss of structural integrity of the septa. Graham considered the pain to be related to cortical fatigue fractures of the medial tubercle of the calcaneus (12). Smith et al (19) suggested “microtrabecular stress fractures (“fatigue perturbation”) of the calcaneus which occur with secondary soft tissue involvement such as enthesopathy, periostitis, myositis, bursitis, and finally the formation of a buttress callus (bone spur) to stabilize a microcortical crack.”
pain have been proposed. In the 1930s, gonorrhea, syphilis, tuberculosis, and streptococcal infections were commonly believed to be major causes (16). Later, many of the theories on gonorrhea were discredited (17,18). Hauser (14) surmised that the heel spur acts like a truss, pointing down into the muscle belly and causing pain. Some investigators postulated that the subcalcaneal fat pad loses its compressibility secondary to thinning and loss of structural integrity of the septa. Graham considered the pain to be related to cortical fatigue fractures of the medial tubercle of the calcaneus (12). Smith et al (19) suggested “microtrabecular stress fractures (“fatigue perturbation”) of the calcaneus which occur with secondary soft tissue involvement such as enthesopathy, periostitis, myositis, bursitis, and finally the formation of a buttress callus (bone spur) to stabilize a microcortical crack.”
Hauser and Hicks had similar ideas regarding the traction forces acting at the insertion of the plantar fascia and intrinsic musculature (15,20). These tension forces are increased during the later part of stance, when the windlass mechanism is a major contributor to the tension. Many authors have shown that not all heel spurs are typically in and of themselves painful (11,21).
Lemont et al (22) histologically examined 50 heel spur resection samples performed for refractory plantar heel pain and found that there was no evidence of inflammation present in any of the specimens. Based on these observations, they recommended that the disorder of recurrent heel pain that is unresponsive to any type of conservative treatment be classified as plantar fasciosis instead of plantar fasciitis.
It is important to note that Lamont’s study only involved submission of heel spurs for microscopic examination, not segments of plantar fascia. Ten specimens were normal, sixteen demonstrated fiber fragmentation with myxoid degeneration of the attached fascia and the remaining samples “were submitted in sections, preventing adequate pathologic analysis.” Myxoid degeneration can be nonpathologic and is often an age-related observation. Lamont’s findings were not stratified by age, sex, or length of symptoms. Based upon this study alone, the characterization of heel pain as the result of “fasciosis” and its therapeutic options should be approached with caution.
In 1981, Przylucki and Jones (7) described a more accurate course of the first branch of the lateral plantar nerve. They noted that the nerve actually passes in proximity to the calcaneal tuber. Thus, it was believed that, in patients with recalcitrant heel pain, this nerve could be the sole or concomitant cause of the painful condition, and these investigators obtained relief in three patients by nerve excision. Sections of the nerve from cadavers, as well as from surgical patients, demonstrated histologic evidence of perineural hypertrophy. This work provided the clinical confirmation for the anatomic studies performed by other investigators (23,24,25 and 26).
Rondhuis and Huson (26) concluded that the site of entrapment was between the deep taut fascia of the abductor hallucis muscle and the medial or caudal head of the quadratus muscle. They presented strong evidence that nerve is a mixed type, providing sensory fibers to the calcaneal periosteum, including over the medial tuberosity, and the long plantar ligament, as well as motor fibers to the quadratus plantae, flexor digitorum brevis, and abductor digiti quinti muscles. This evidence may help to explain the more neuralgic symptoms that are characteristic of this cause of heel pain.
Baxter and Pfeffer (27) referred to the heel spur as an unlikely cause of direct mechanical heel pain. However, they believed that inflammation in the area of the spur is a theoretic source of compression of the first branch of the lateral plantar nerve as it passes superior to the spur. Patients exhibiting maximal tenderness over the area between the abductor hallucis and quadratus plantae muscles were proposed to suffer from nerve entrapment, and this test could be considered the “hallmark of this compression neuropathy.” In their study of 69 heels in 53 patients undergoing operative decompression of the inferior calcaneal nerve, 89% of these patients’ heels experienced good to excellent results, with 83% achieving complete resolution of pain after an average of 49 months.
Chronic exertional compartment syndrome has become recognized as a potential source of pain and disability in the lower extremity (28,29,30,31 and 32). Some research has focused on the possibility of compartment syndromes in the foot. Mollica described chronic exertional compartment syndrome as a transient, symptomatic pressure increase within a myofascial compartment that is precipitated by exercise and subsiding with cessation of athletic activity (50). The medial compartment appears most susceptible to chronic exertional compartment syndrome in the foot (33). This compartment contains the following: the abductor hallucis and flexor hallucis brevis muscles; the tendons of the flexor hallucis longus, peroneus longus, and tibialis posterior; and the medial planter nerve. In addition, this medial compartment does not communicate with any other compartment of the foot or ankle. Patients may report “cramp-like” pain and tightness in the arch (33). Pain may be preceded or followed by tingling or numbness. These symptoms may mimic classic plantar fasciitis pain when the medial compartment of the foot is involved. Palpation of the abductor hallucis muscle belly, medial to the plantar fascia, elicits a painful response.
Most of the current literature points to abnormal foot mechanics as a major influence in producing the heel pain syndrome. Excessive traction of the plantar fascia and intrinsic musculature are responsible for the majority of cases of heel pain. Bone scintography and MRI typically demonstrate inflammation of bone and soft tissue in the area of the calcaneal tuberosity.
Bergmann (34) concluded that “any force that causes an excessive pull at the origin of the plantar fascia or muscle can cause heel spur syndrome.” He referred to the various biomechanical abnormalities causing abnormal or excessive pronation (tibial varum, short Achilles tendon, compensated rearfoot varus, forefoot varus, flexible and partially flexible forefoot valgus, or a combination) as potential causes of heel spur syndrome.
DIAGNOSIS
Heel pain has many potential diagnoses. However, there is little mistaking the signs and symptoms of classic heel spur syndrome, more accurately referred to as plantar fasciitis. Subjectively, the patient usually presents with pain in the heel on arising in the morning or after periods of rest (referred to as poststatic dyskinesia). Although the pain abates after several steps, it may slowly worsen as the day progresses. In severe cases, the pain is constant and may awaken the patient from sleep. Patients may describe the pain as a deep tenderness, the classic “stone bruise,” or as a sharp, sticking sensation as if a needle were in the heel. Pain radiates into the arch in many patients, but a few complain of numbness or tingling in the sole of the foot. The symptoms are episodic at first and so delay the patient’s initial presentation to the office.
Examination reveals two distinct groupings of patients. The first subgroup has plantar central palpatory tenderness at the insertion of the central band of the plantar fascia into
the calcaneal tuberosity. Patients have little to no tenderness medial to this area. Palpation along the course of the plantar fascia is unremarkable. The calcaneal tuber is often prominent, and adventitious bursae are occasionally present.
the calcaneal tuberosity. Patients have little to no tenderness medial to this area. Palpation along the course of the plantar fascia is unremarkable. The calcaneal tuber is often prominent, and adventitious bursae are occasionally present.
The larger group of patients, however, has increased palpatory tenderness along the plantar medial and inferior medial wall of the calcaneus. This feature differentiates fasciitis from the lateral wall pain of a stress fracture. Although the nature of the subcutaneous tissues does not allow for much swelling, the bottom of the heel often feels tense. Patients with stress fractures and systemic arthritides usually present with edema along the medial and lateral calcaneal walls. In plantar fasciitis, pain may also be elicited by active or passive extension of the foot and digits. Palpatory tenderness extends along the fascial band into the medial arch. As the patient begins to compensate for chronic pain, symptoms often develop along the posterior and lateral rim of the heel pad.
Little comprehensive data exist regarding the foot type and biomechanics of the patient with plantar heel pain. Scherer noted that whereas fewer than 25% of his patients had an everted heel, 86% demonstrated supination of the longitudinal midtarsal joint axis in stance (35). Amis noted that 75% of his patients had less than 5 degrees of ankle joint dorsiflexion. Biomechanical information gleaned from radiographs has demonstrated that 81% of patients with symptoms had evidence of pronation (21). In another group, the mean calcaneal pitch in normal control subjects was 20.5 degrees and in those with heel pain it was 15.9 degrees. Powell et al (36) classified only 19% of their patients as pronated, whereas 75% had normal findings.
The prevalence of plantar calcaneal spurs in the general population ranges from 8% to 18% (21,37,38 and 39). The presence of spurs increases with age (56). A random survey of 1,228 black Africans revealed that approximately 50% of patients who were more than 50 years of age had spurs. In the group of patients less than 30 years of age, the incidence dropped to 20%, but the overall average incidence of spurring was 15% (with females predominating over males) (39). Radiographs also help to rule out osseous causes of heel pain such as bone tumors, stress fractures, and even fractures of the spur itself.
Clearly, most plantar spurs are asymptomatic. In a review of 1,000 radiographs, Shama et al (21) noted a 13.2% incidence of heel spurs, but only 31% of these patients were symptomatic. Prichasuk and Subhadrabandhu (40) studied the asymptomatic contralateral foot of patients with heel pain and found spurs in nearly two-thirds of these feet. However, approximately three-fourths of patients with symptomatic heels possess spurs (21,38,39,41,42 and 43). A definite correlation exists between heel pain and spurring, but the significance of this relationship has yet to be defined.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








