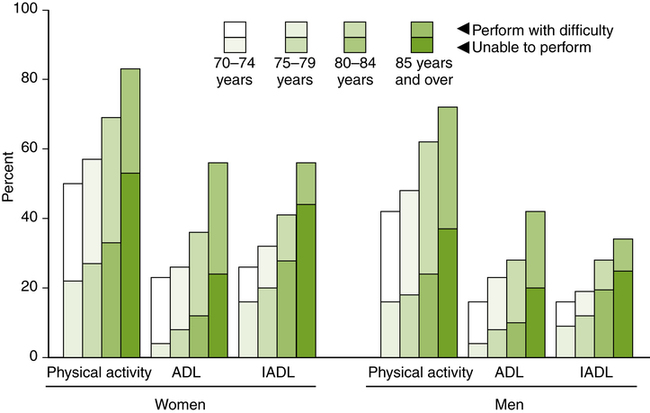
Jennifer E. Collins and Teresa A. Hoppenrath After reading this chapter, the reader will be able to: PTs have provided services to individuals with conditions common to people over the age of 65 for many decades. However, only in the past two decades have PTs and PTAs worked with older persons in such large (and growing!) numbers. Current trends in health care and life expectancy have rapidly increased the numbers of older adults requiring some type of physical therapy services, whether rehabilitative or preventative. For example, according to U.S. census data, in 2009 there were 39 million people over the age of 65 in the United States, or 12.8% of the population.1 It is expected that this will more than double between now and 2050 to 89 million, whereas the remainder of the population is expected to increase by only 49%. Globally, the world’s 65-and-older population is expected to triple by 2050.2 For an individual born in 2004, the life expectancy is 78 years, the longest life expectancy ever experienced in the United States.3 Figure 13-1 presents data on ADLs and IADLs of persons 70 years of age and older who are not institutionalized.4 The data indicate that nearly 47% of these individuals have difficulty in performing one or more of the activities. The percentage increases with age and is higher for women in all categories. This information confirms that PTs have an important role in improving functional performance. Although individual differences exist, the aging process includes changes that are common in older persons. Sometimes, professionals find it useful to differentiate between well elderly and frail elderly because people in each group have needs quite distinct from those of people in the other group. Well elderly refers to people 65 years of age and older who are not experiencing physical limitations or who have age-related changes that are not significant enough to affect function. The 86-year-old woman in Figure 13-2 is a good example of a person described as one of the well elderly. Although she has minor medical problems, these do not significantly affect her daily activities. The primary goal related to physical therapy for someone like her is to achieve good physical function and prevent conditions that might limit her ability to continue at this level. In contrast, the term frail elderly is used to describe people over age 65 with conditions that significantly impair daily function or who require frequent medical intervention. For these people, PTs offer strategies to regain mobility skills or to modify the environment to maximize the individual’s function. It is easy to envision the PT as a clinician who provides hands-on services (direct intervention) to older adults. However, in each of the settings described earlier, PTs are also educators. With valuable knowledge of the physiologic aging process, PTs are the ideal professionals to educate patients, family members, and other professionals to prevent and minimize impairments, functional limitations, and disability. Armed with facts, older people will be better able to exercise appropriately and maintain or regain skills. For example, the woman in Figure 13-3 is being taught how to use her arms to more easily get up from a reclined position. The PT is in an excellent position to teach the older person that strength and endurance can be increased with properly designed programs. The physical changes observed in older adults that affect the musculoskeletal system (bones, muscles, and joints) often result in poor posture, changes in gait pattern, and decreased strength and flexibility. Decreased strength is often related to hypokinesis (decreased activity or movement) and the decreased muscle mass (sarcopenia) typically seen in older people. Muscle mass is reduced because of a decrease in the number of muscle fibers.5 The reduction in fibers is related to loss of motor neurons (nerves innervating muscles) and active motor units (a single motor neuron and all the muscle fibers it innervates).6 Bone also undergoes changes with age. In studies of vertebral bodies, bone mass was shown to decrease by 35% to 40% between the ages of 20 and 80 years.7 This finding suggests that bone is weaker in older people. This change may eventually advance to osteoporosis. Weight-bearing joints such as hips or knees degenerate over time. Excessive wear and tear destroys articular cartilage (which covers the ends of bones) causing impairments such as pain, inflammation, and deformities. Obesity is a risk factor that causes additional stress to these joints, facilitating rapid deterioration8 (see the discussion of arthritis in the section on common conditions). The central nervous system shows a reduction in conduction velocity associated with age.5 The reduction affects the ability of the nerve to transmit impulses. This change tends to make movement responses slower in older persons and may explain the reduced ability to respond rapidly to loss of balance or the slowed gait pattern often seen in later life. Several of the sensory systems display changes that significantly affect mobility, specifically in the ability to move safely in the environment. The visual system is important in providing accurate information regarding the environment. In the older person the lens becomes less elastic, and the muscles around the lens decrease in their ability to accommodate rapidly from seeing far to near distance.9 Visual acuity is also reduced. These changes make lighting and contrasting colors important in offering the older person cues about objects or surfaces that might interfere with safe mobility. When the lens becomes cloudy it creates a condition known as cataracts, which also affects acuity. Macular degeneration is a condition that affects the retina, resulting in a central loss of vision. Visual changes can cause an increase in falls in the older population.10 Older people display a group of characteristics called presbycusis (“old people’s hearing”). This term refers to the decreased ability to perceive higher pitches and to distinguish between similar sounds.11 Auditory acuity is also reduced. These changes must be considered and strategies need to be adopted (such as lowering of the voice, talking more slowly, or looking directly at the patient at all times) when instructions are given in a physical therapy session. Age-related changes in the cardiovascular system are complicated by the characteristic cardiovascular diseases of aging. For example, 67% of people over the age of 60 have hypertension (high blood pressure).12 Non-Hispanic blacks (men and women) are more likely to be hypertensive than people of any other racial or ethnic group.13 It appears, however, that overall cardiac performance at rest is not altered by age in healthy people, although cardiac response to stress does differ. This is demonstrated by a decrease in maximum cardiopulmonary function and work capacity.14 Increased stiffness in the chest wall affects the respiratory system, which further reduces the effectiveness of cardiopulmonary function. These changes should be considered carefully in the design of exercise programs for individuals over 65 years of age. Balance is a skill essential for safe and independent daily function. Limitation in balance and an increase in the risk of falling are common problems in older adults. Falls have been reported to occur in more than 35% of people over the age of 75.15 Static balance and dynamic balance are the result of a complex interaction of multiple systems subject to age-related changes mentioned previously. If any of these systems undergoes change, balance may be affected as well. A fall resulting from a loss of balance could expose the elder to a multitude of subsequent impairments, such as fracture or other trauma, pneumonia, decubitus ulcers, and loss of strength or range of motion. The psychosocial impact on the individual can also be disabling. Fear of falling and loss of confidence may cause the individual to become isolated or more sedentary. If the fall is serious enough to cause injury, the elder could lose the ability to safely live independently. For many years one of the most common myths of aging was that cognitive function always significantly decreases with advanced age. In fact, people seemed to assume that dementia was inevitable. It is now known that deterioration of cognitive function characterized as dementia is related to Alzheimer’s disease or some other pathologic condition, not to aging itself. Reports indicate that 10% of the general population over 65 years of age, and 20% of people over age 85, display dementia.16 Health professionals serving older people are aware of how to recognize dementia and how to interact with people with dementia; however, the characteristics of dementia are not displayed universally by people over age 65 or even those over age 85. Significant cognitive changes that do fall in the category of normal aging are in memory and conceptualization (tasks requiring abstract thinking).17 Specifically, the manner in which new information is stored (encoded) in the memory is altered. This leads to difficulty in retrieving newer information. Studies show that training in memory techniques, such as list organization, can improve recall in older persons.18 Psychosocial changes may affect people in older population groups. These vary widely based on the individual, family, environment, and presence of other changes or actual disease. What is important for the PT and PTA to remember is that understanding psychosocial issues is crucial to the success of any rehabilitation program. Social considerations such as adjustment to retirement, loss of lifetime roles (e.g., worker, parent, homeowner, athlete), living environment, and presence or absence of health insurance have a tremendous impact on the elder’s life. Older persons may be required to adjust to the loss of spouses, friends, and siblings. Psychiatric disorders such as depression, dysthymia (disorder of mood), and anxiety are more common among homebound older people than those who are able to be out in the community.19 The PT or PTA has a responsibility to bring signs of psychological problems to the attention of other members of the health care team. Many impairments that are more prevalent in older people can benefit from physical therapy intervention. Individuals with the following common conditions are frequently seen by PTs and PTAs. Problems for older adults that are neurologic in nature, such as Parkinson disease and cerebrovascular accident (CVA), are discussed in Chapter 9. Therapists should be aware of the impact of medical conditions on the older person’s ability to recover from functional limitations. A retrospective analysis of a group of more than 1000 people older than age 65 showed that an older person who has two or more medical conditions is less likely to recover function in such tasks as dressing or carrying 10 lbs. Diabetes mellitus, stroke, depression, and hip fracture had the greatest effect on recovery.20 By far the most common problem for older people is one of the joint diseases described as arthritis. In 1995, 43 million people in the United States were affected by arthritis.21 African Americans have a higher rate of osteoarthritis (OA) than whites or Hispanics. OA most commonly affects the hands, spine, knees, and hips and occurs when the cartilage deteriorates owing to advancing age and/or obesity. Patients often complain of morning stiffness and pain on movement. This may alter a gait pattern or make simple tasks such as buttoning a blouse very difficult. It is important for the person with OA to maintain at least a moderate activity level while protecting the joints. PTs and PTAs can teach appropriate exercise routines (such as aquatic exercises) to maintain flexibility without excessively stressing the joints. For people who are excessively overweight, programs that address weight loss as well as exercise and joint protection are beneficial to reduce the stress on the joints. There are some facilities and therapists that specialize in treating such individuals. Their services may be referred to as bariatric programs.8 With an aging population and the escalation of obesity, the economic burden of arthritis is likely to continue to escalate. In contrast to OA, rheumatoid arthritis (RA) is a disease of the immune system that causes chronic inflammation of the joints. It is more common in women than in men, and the peak incidence occurs at 40 to 60 years of age.22 It is characterized by enlarged joints that are often reddened and warm to the touch. The affected joints are stiff and painful, usually more so in the morning or after extended periods of inactivity. This disease process leads to limited range of motion, joint deformity, and, eventually, progressive joint destruction. Typical physical therapy goals for the person with arthritis are pain relief, increased joint movement, assistive devices to facilitate independent function, and rehabilitation when joint surgery is required.
Physical Therapy for the Older Adult
 Identify three specific reasons that a physical therapist would modify an intervention for an older person
Identify three specific reasons that a physical therapist would modify an intervention for an older person
 Differentiate between static and dynamic balance
Differentiate between static and dynamic balance
 Describe the primary role for the physical therapist or the physical therapist assistant in each of the common conditions discussed in this chapter
Describe the primary role for the physical therapist or the physical therapist assistant in each of the common conditions discussed in this chapter
 Explain why an interdisciplinary approach is important when developing a plan of care for an older person
Explain why an interdisciplinary approach is important when developing a plan of care for an older person
General Description
Demographics
Roles for Physical Therapists with Older Adults
Aging-Related Changes
Common Conditions
Osteoarthritis
Rheumatoid Arthritis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine