Phalangeal fractures and dislocations
Treatment considerations for elderly patients
INTRODUCTION
Phalanx fractures and dislocations are some of the most common musculoskeletal injuries. The goal of treatment is to optimize hand function and minimize adverse outcomes. Elderly patients are, in general, more accepting of deformity, have lower functional demands and adapt less well to cumbersome treatments. This chapter addresses the management of phalanx fractures in the elderly.
EPIDEMIOLOGY
In 1998, approximately 0.84% of all patients visiting an emergency room in the United States had a hand fracture, most often a phalanx fracture.1,2 Finger fractures are most common in childhood. The incidence of finger fracture is 16/100,000 patients in a year among people aged 55–64 years and 35/100,000 in people aged 65–74 years, which is much less than the 185/100,000 in children aged 5–14 years.1 Phalanx fractures are more common after falls in elderly women and during sports among boys and young men.3,4
ANATOMY
Final hand function after phalanx fracture is influenced by the condition of the skin, tendons and nerves. There are three phalanges in each finger that are connected by the proximal interphalangeal (PIP) joint and the distal interphalangeal (DIP) joint (Figure 29.1). The thumb has two phalanges and only one interphalangeal (IP) joint.
The distal phalanx is the smallest of the phalanges. The tip of the distal phalanx is horseshoe shaped and referred to as the tuft. The central, thinner part of the distal phalanx is called the shaft and has a smooth surface. The proximal portion of the distal phalanx is called the base and along with the distal portion of the middle phalanx constitutes the DIP joint. The middle phalanges and proximal phalanges have similar shape, although the proximal phalanges are larger in size. Each of them has a base, shaft, neck and head from proximal to distal. The heads of these phalanges enlarge as two condyles separated by a shallow groove.
The DIP joint can hyperextend. The capsule is reinforced by the collateral ligaments and volar plate. Movement and stability are enhanced by the terminal extensor tendon and flexor digitorum profundus (FDP) tendon.
The head of the proximal phalanx and base of the middle phalanx constitute the bony structures of the PIP joint. The PIP joint is a hinge joint that has flexion and extension motions. The collateral ligaments originate from the proximal phalangeal head and insert on the base of the middle phalanx. The length of the collateral ligaments changes little as the proximal phalanx is flexed and extended.5 Accessory collateral ligaments (ACLs) originate slightly proximal and volar to the collateral ligaments and insert on the volar plate and flexor sheath. These ligaments provide lateral stability as the joint moves. The volar plate is a fibrocartilaginous structure that is attached proximally to the neck of the proximal phalanx and distally to the base of the middle phalanx. The volar plate limits hyperextension of the joint.
The metacarpophalangeal (MCP) joint is a condylar joint that can move along two axes including flexion/extension and radial/ulnar deviation.6 The soft tissue boundaries of the joint are also made up of the articular capsule, the collateral ligaments and volar plate. The volar plate is more flexible and mobile than the PIP volar plate. Unlike the PIP joint, there is a pear-shaped metacarpal head in the MCP joint. The collateral ligaments are longest in flexion and shortest in extension because of the ‘cam effect’ produced by the larger radius of curvature on the volar part of the head as well as the pear shape in the coronal plane. To limit the chances that the collateral ligaments will contract at the shorter position in extension, the MCP joint is typically immobilized in 70–90 degrees of flexion (Figure 29.2).
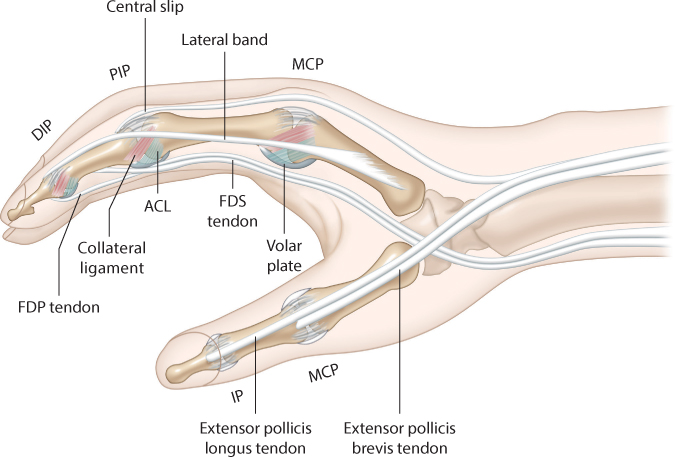
Figure 29.1 A simplified diagram illustrating the phalanges and joints of the digits.
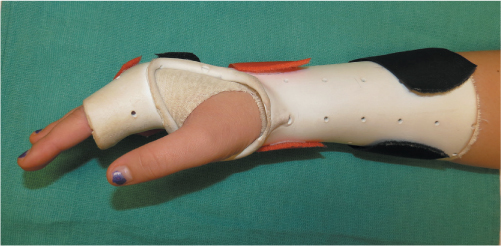
Figure 29.2 Safe position of the hand. The wrist is in 30 degrees of extension, the metacarpophalangeal joint is in 70–90 degrees of flexion and the proximal interphalangeal joint is in full extension.
The dorsal extensor apparatus, FDP tendon, flexor digitorum superficialis (FDS) tendon and the flexor sheath are close-knit to the phalanges and joints. One-half of the dorsal distal phalanx is covered by nail bed and nail (Figure 29.3).
TREATMENT CONSIDERATIONS FOR ELDERLY PATIENTS
Some chronic hand diseases such as rheumatoid disease, osteoarthritis and Dupuytren disease are common in elderly patients. Three radiographic views are usually sufficient to define the location, orientation, displacement and fragmentation of the fracture as well as pre-existing arthritis (Figure 29.4). The goals of treatment are adequate alignment and motion and a durable articulation.
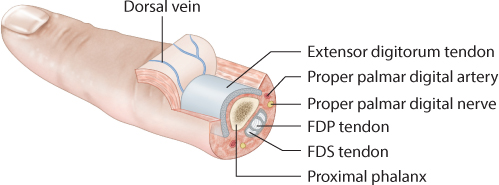
Figure 29.3 Cross-sectional anatomy of the proximal phalanx of the finger.
Most closed non-displaced fractures as well as some displaced fractures after closed reduction are stable. They can be managed with a splint or buddy taping to adjacent fingers (Figure 29.5). Irreducible fractures and fractures that lose alignment after reduction are considered for operative treatment.
Rotation and angulation of a phalanx fracture can cause the finger to overlap or diverge. Angulation of the fracture apex volar or dorsal will result in a bone–tendon length discrepancy leading to an extension lag. It is difficult to judge rotational alignment on radiographs.7 Measurements of the angle of the nail plate relative to the horizontal plane are not accurate for malrotation because there is substantial variation from person to person and finger to finger.8 Soft tissue swelling and pain can affect accuracy, but observation of the fingers during passive or active flexion is the most reliable test of malrotation. The overlapping or divergence of the finger indicates rotation or angulation deformities of the fractures (Figure 29.6). It is also used to address whether the deformities are corrected after fracture reduction.

Figure 29.4 Radiographs of a volar base fracture of the ring finger middle phalanx. (a,b) Anteroposterior and oblique views show a narrow joint space and incongruent surface of the proximal interphalangeal (PIP) joint, but the intra-articular fracture with dislocation of the PIP joint is not apparent. (c) The lateral view demonstrates the intra-articular fracture and dorsal dislocation of the joint.
Immobilization of fingers for more than 4 weeks has been shown to increase joint stiffness as a result of extensor tendon and joint capsular scarring.9 Rigid internal fixation allows early mobilization to prevent finger stiffness. However, open reduction and internal fixation (ORIF) causes additional soft tissue injury, which may result in more adhesions that may limit motion and cause complications. The surgeon should strive to balance bony stability and tissue injury, using an individualized approach based on fracture type and injury configuration.
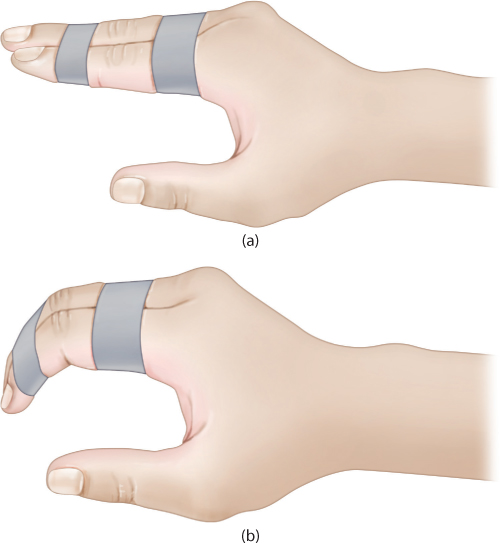
Figure 29.5 (a,b) Buddy taping allows the injured finger to move with the adjacent finger that provides support.
PHALANGEAL FRACTURES
Distal phalangeal fractures
The distal phalanx is most the commonly fractured phalanx.10 The long finger distal phalanx is the most common because its length makes it more vulnerable.11 Distal phalanx fractures can be divided into tuft fractures, shaft fractures and base fractures.
Typically, tuft fractures are caused by crush injuries to the fingertips. These fractures can be longitudinal or transverse, but most of them are comminuted fractures with associated nail bed injuries. Closed tuft fractures are usually stable owing to the volar soft tissues and dorsal nail plate. Symptomatic treatment, sometimes including protective splinting of the DIP, is sufficient for closed tuft fractures.12 Even with displacement, open reduction is not helpful if the fracture fragments are too small for fixation. Non-union of the comminuted tuft fractures is often asymptomatic owing to fibrous union. The roles of subungual haematoma decompression for pain relief and nail bed repair for improved aesthetics are both debated and are unnecessary in older patients. For open fractures with nail bed injury, small devitalized fracture fragments can be removed during debridement followed by nail bed and soft tissue repair. Substantial displacement on radiographs often indicates severe soft tissue injury. Adequate reduction of the fracture often restores vascularity to an initially dysvascular tip that is widely displaced.
Non-displaced shaft and base fractures of the distal phalanx can be immobilized by splinting the DIP for 3 weeks for comfort or allowed protected active mobilization. Most displaced fractures of the shaft of the distal phalanx are open fractures with a transverse laceration of the nail matrix. If the fracture does not stay aligned after reduction, suture of the skin and nail bed, and replacement of the nail plate with a piece of suture pack foil, the fracture can be fixed with one or two Kirschner wires (K-wires) (Figure 29.7). Fractures that realign well can be splinted with the DIP joint extension for 4–6 weeks with regularly scheduled radiographs to confirm fracture reduction.
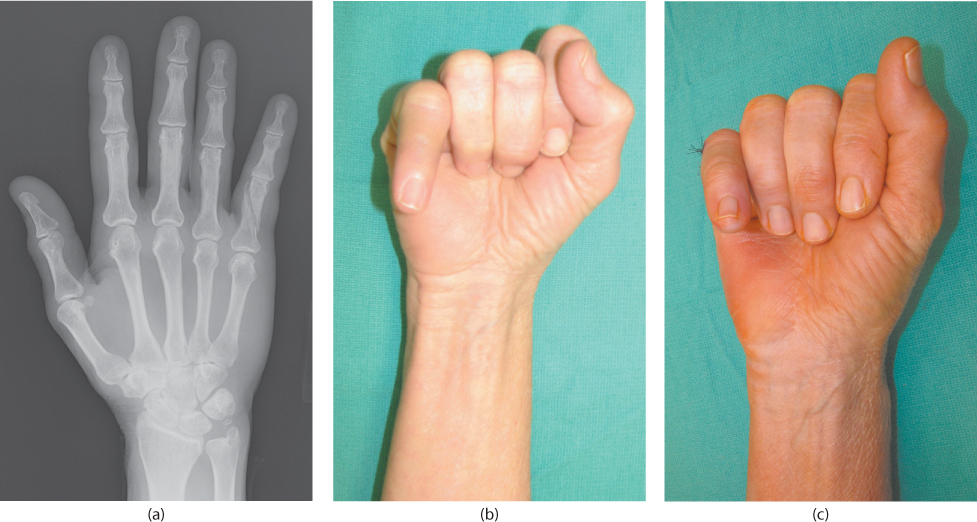
Figure 29.6 (a) Radiograph demonstrating a spiral fracture of the small finger of a 63-year-old woman. (b) Rotation of the fracture results in divergence of the small finger while making a fist. (c) Correction of the divergence of the small finger after open reduction of the fracture.
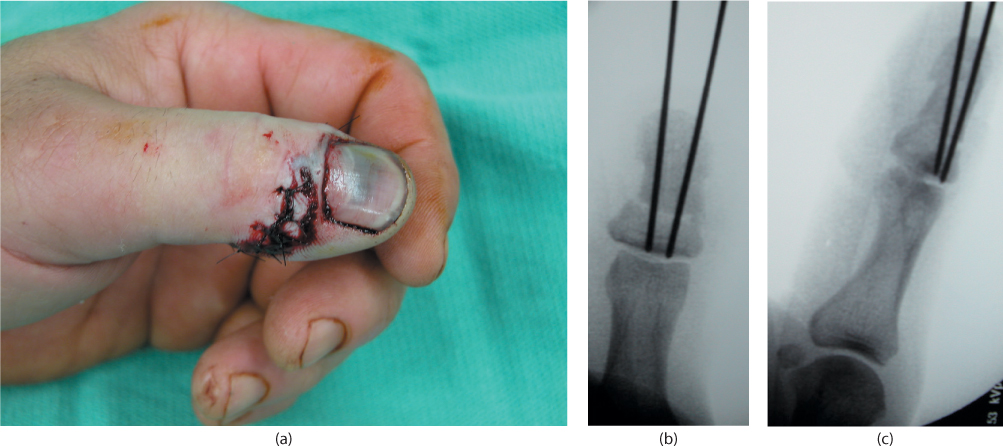
Figure 29.7 (a) A 68-year-old man sustained a crush injury to his left thumb. (b,c) Intraoperative fluoroscopies show the distal phalanx fracture of the thumb is fixed by two K-wires after closed reduction.
Intra-articular fractures at the dorsal base of the distal phalanx are called mallet fractures. The finger presents with a flexion deformity with inability to extend the DIP joint (Figure 29.8). Although mallet fractures are displaced intra-articular fractures, the role of ORIF is debated. Some authors suggest that less than one-third of the articular surface of the DIP joint can be treated with a splint.13 Other authors state that non-operative treatment yields good results even when the displaced fragment of the fracture is greater than one-third of the articular surface of the distal phalanx unless there is volar subluxation of the remaining intact joint.14 The DIP joint of the affected digit is immobilized in extension or slight hyperextension for 4–6 weeks. A variety of splints are available that can be applied along the dorsal or volar aspect of the DIP joint or both. In the study of Wehbe and Schneider, 21 patients aged 5–56 years old were followed for a mean of 3 years.15 Six were treated surgically and the others were splinted. All but one regained a near normal range of painless motion of the DIP joint. Wehbe concluded that ORIF offered no advantage over non-operative treatment and surgical treatment had more problems. Kalainov et al. retrospectively reviewed 22 closed mallet fractures in 21 patients (20–69 years old) who were treated by a DIP joint extension splint.16 The sizes of all fractures were greater than one-third of the articular surface, and 13 of them presented with volar subluxation of the DIP joint. At 2-year follow-up evaluation, all patients reported minimal difficulties with activities of daily living and work, and the patients expressed relatively high satisfaction with finger function. Considering that surgical treatment of mallet fractures is difficult and unreliable, we recommend non-operative treatment for elderly patients.
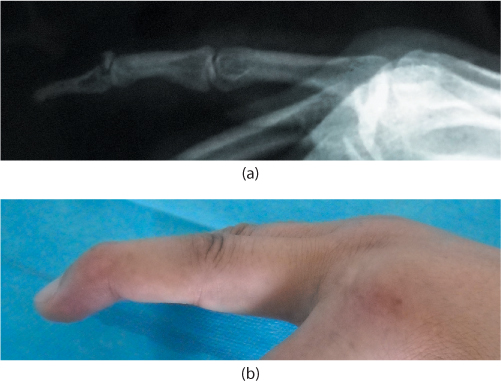
Figure 29.8 Mallet fracture. (a) Lateral radiograph demonstrates a dorsal articular avulsion fracture of the extensor tendon insertion of the middle finger. (b) The patient presented with a flexion deformity of the distal interphalangeal joint.
Intra-articular fractures at the volar base of the distal phalanx are often caused by avulsion of the terminal FDP tendon. They occur most commonly in sports activities and are uncommon in the elderly. If operative treatment is favored, fixation depends on the size of the fragment: pull-out suture technique, K-wire, screw or suture anchors are options.
Lateral fractures of bases are due to lateral ligament avulsion, and the fragments are usually small. Splinting the DIP joint in extension for 3–4 weeks is sufficient treatment.
Middle and proximal phalangeal fractures
NON-ARTICULAR FRACTURES
Stable and minimally displaced extra-articular fractures of the middle and proximal phalanges can be immobilized in a splint for 3–4 weeks, or mobilized immediately by strapping the injured finger to an adjacent finger (buddy strapping).
Displaced transverse fractures of one finger with little or no soft tissue injury are treated with closed reduction under local anesthesia. Most displaced transverse fractures displace with an apex angulation configuration, because the fragments are pulled by the interosseous muscles, lumbricals and extensor tendons. For reduction of the fractures, longitudinal traction is applied in the distal direction, and then the distal fragment is flexed to correct the angulation deformity. Both radiographic and clinical alignment should be checked after reduction, rotation in particular. For stable fractures, a short arm cast is used to immobilize the hand in safe position. If a fracture is stable only when the IP joints are in flexion, then the fracture is considered to be unstable. The unstable transverse fractures after reduction will be pinned to keep alignment. The cast or pin is maintained for approximately 3 weeks; buddy taping is continued for an additional 2 weeks after that.
Displaced oblique, spiral and comminuted fractures are often considered unstable fractures. In these cases, percutaneous or internal fixation will be performed. A wide variety of fixation methods is available, and selection of the technique is largely based on surgeon experience and preference.
K-wires
K-wires are commonly used for fixation usually after closed reduction but sometimes after open reduction. For short oblique and transverse fractures, the finger is distracted and reduced under fluoroscopy guidance. One 0.045-inch (1.1 mm) K-wire is inserted through the flexed MCP joint and down the medullary canal of the proximal phalanx to stabilize the fracture. Another crossed 0.045 K-wire can then be placed near the mid-lateral line of the finger to limit rotation (Figure 29.9). For open reduction, the K-wires can be inserted antegrade and then passed retrograde through the fracture site after reduction.
For long oblique fractures, K-wires are inserted perpendicular to the fracture line. A pointed reduction forceps is helpful to maintain reduction of the spiral oblique fracture while K-wires are inserted.17 The PIP joint is not usually immobilized, but crossing the DIP joint can limit the potential for extensor lag in the treatment of middle phalanx fractures. The patient is placed in a splint and gentle limited active PIP motion exercises are initiated 1 week postoperatively. The wires are removed in the office 3–4 weeks after insertion.
The major advantage of pin fixation is minimal soft tissue damage. Favourable outcomes are reported in some studies.17,18 Green and Anderson achieved full range of motion in 18 of 22 patients with long oblique fractures of the proximal phalanx treated by closed reduction and two or three percutaneous pins.18 Belsky and colleagues used transverse K-wire fixation for 100 patients with long oblique phalangeal fractures.17 Good and excellent results were reported in 90% of fractures, and a total active movement of 215 degrees or more was achieved in 61% of fractures. Other studies have less optimal results. Faruqui et al. reviewed 338 patients with the base of the proximal phalanx fractures treated by closed reduction and percutaneous pinning.19 Nearly half of the patients had flexion loss averaging 20 degrees and a third of patients had fixed flexion contracture greater than 15 degrees at the PIP joint.
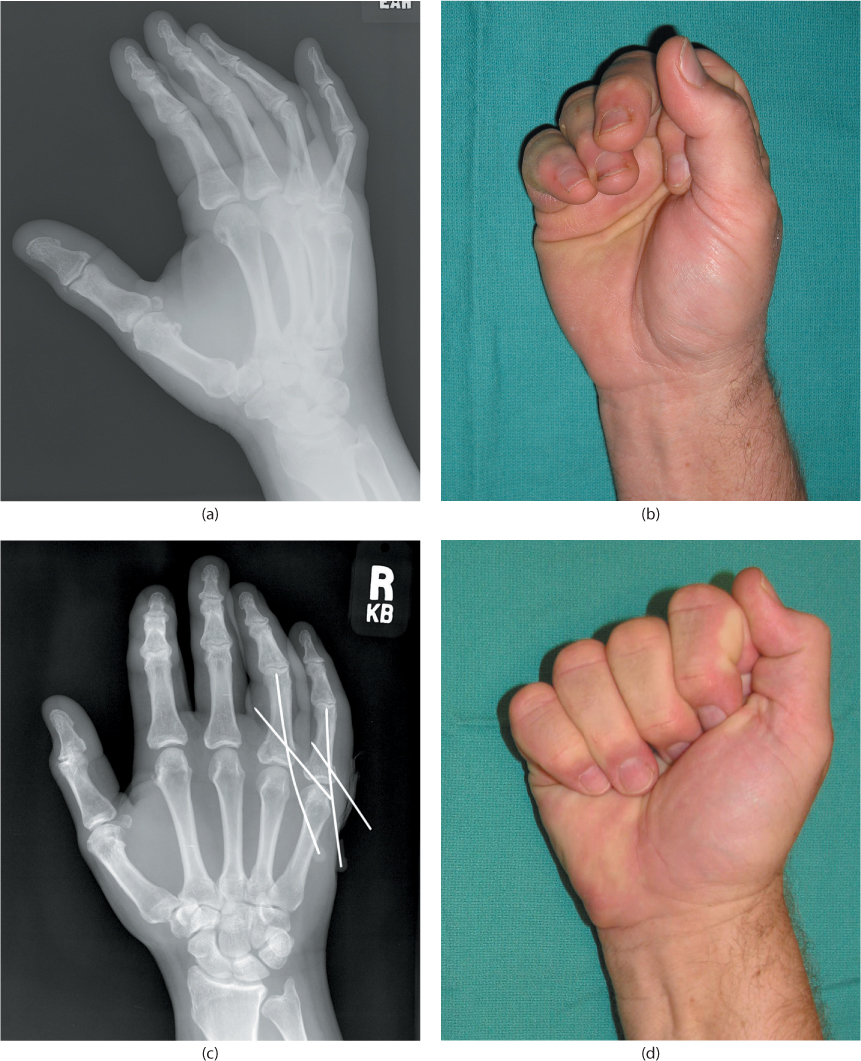
Figure 29.9 Percutaneous K-wire fixation of proximal phalangeal fractures. (a) The fractures at the base of the proximal phalanges of the ring and little fingers of a 65-year-old man are shown on the radiograph. (b) The flexion function of the hand preoperatively. (c) Radiograph shows two cross K-wires were used to fix the fractures after closed reduction, and the proximal interphalangeal (PIP) joints are not pinned. (d) The final flexion function of the hand after the K-wires were removed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








