Periprosthetic Tibial Fractures
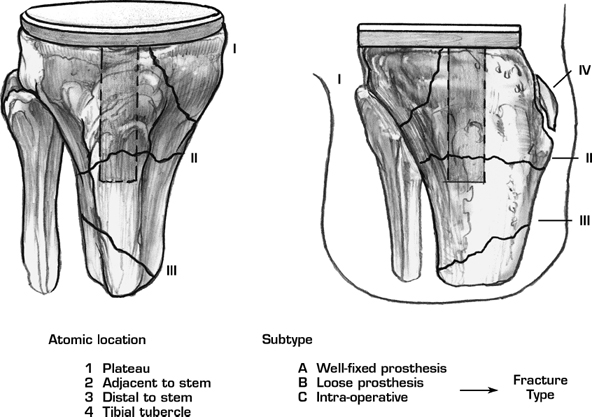
Periprosthetic tibial fractures are quite uncommon.1 Management of these fractures requires a combination of fracture management and revision arthroplasty skills. Use of a classification system facilitates decision making and helps direct one toward the proper treatment approach (Fig. 47–1).2
Indications
- Displaced fractures
- Loose prostheses with or without bone deficiencies
- Axial malalignment
- Prosthesis malposition
Contraindications
Nondisplaced fractures associated with a well-fixed prosthesis and good limb alignment are managed best with nonoperative fracture treatment principles.
Mechanism of Injury
- Postoperative fractures occur by a variety of mechanisms including a traumatic episode,3 a spontaneous event through an area of osteolysis, or as a stress phenomenon related to limb or prosthesis malalignment.4
- Intraoperative fractures occur during removal of prosthesis or cement, reduction of trial components, or insertion of a stemmed or keeled tibial component.2
Physical Examination
Assessment of soft tissue envelope, integrity of extensor mechanism, and documentation of neurovascular status.
Diagnostic Tests
Anteroposterior and lateral radiographs are required. Supplemental oblique views with spiral tomographic radiographs are often helpful. Preoperative knee aspiration to rule out deep periprosthetic infection is advised.
Preoperative Planning and Timing of Surgery
Most fractures are managed best on a semielective basis due to the possibility of requirement for revision knee instrumentation, fracture fixation instruments, and structural bone graft. External fixation techniques are not recommended for periarticular fixation due to the potential for pin site contamination and subsequent prosthetic infection.
Special Instruments
- Revision knee instrumentation incorporating constrained articular designs, stemmed components, modular wedge augments, and occasionally hinged knee implants
- Fracture fixation implants including specialized periarticular plates
Surgical Procedure
Approach
Previous arthroplasty incisions should be used whenever possible. Percutaneous incisions may be helpful for placement of lag screws.
Tips and Pearls
Use of the classification system to determine timing, anatomic location, and status of prosthesis fixation allows the creation of a treatment algorithm (Fig. 47–2).2 Once the proper treatment approach has been determined, the vagaries of reconstruction and fracture fixation possibilities are numerous. Following the principles of good limb alignment, proper prosthesis selection and positioning and rigid fracture fixation are key ingredients to a successful outcome.5
Pitfalls and Complications
The combination of revision knee arthroplasty and fracture fixation skills required for a successful outcome suggests careful assessment of resources and capabilities. Minimally invasive treatment for fractures is generally unsuccessful. Delay of surgical intervention often results in progressive joint stiffness, bone loss, and consolidation of the fracture fragments, which increases the difficulty of subsequent reconstruction efforts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








