Perioperative Medical Management of Hip Surgery Patients
A. Scott Keller and Deanne T. Kashiwagi
Key Points
Introduction
Orthopedic hip surgeries are becoming more common as our population ages. Approximately 200,000 total hip replacements, 100,000 partial hip replacements (90% of which were performed for fractures of the neck of the femur), and 36,000 revision hip replacements were performed in the United States in 2003, with in-hospital mortality rates of 0.33%, 3.04%, and 0.84%, respectively.1 In 2006 alone, 330,000 hip fractures were reported.2 Although surgical techniques have continually been refined and improved and modern anesthesia is extremely safe, with an estimated mortality of 1 in 250,000,3 patients still may suffer from medical complications. Most of these complications occur after surgery because of the significant surgical stress response, which may lead to an acute exacerbation of underlying chronic disease, especially in older patients who have diminished organ reserve capacity and comorbid medical conditions.
This chapter explains the surgical stress response, reviews the components of the preoperative evaluation, discusses techniques to help medically optimize patients, and provides a symptom-based approach to diagnosis and treatment of postoperative medical complications.
Basic Science
The Surgical Stress Response
The human body responds to the stress of an injury through a remarkable physiologic process that activates the sympathetic nervous and endocrine systems and promotes an increased inflammatory response with decreased immune function (despite initially increased production of reparative leukocytes).4–7 The magnitude and duration of these effects are directly proportional to the degree of injury,6,8 with overall goals of maintaining intravascular volume for cardiovascular homeostasis and increasing catabolism to provide energy sources.4 Although the stress response is appropriate and can prolong survival following accidental injury, it can be counterproductive following the “controlled injury” of surgery.
Many of the initial surgical stress response effects are attenuated by anesthesia and opioids but may manifest postoperatively. As a result, most postoperative complications are due to subsequent increased demands on organ function6,9,10 in the setting of preexisting comorbid conditions,6,11,12 rather than to anesthetic13 or surgical effects. The overall stress response may persist for up to 7 days,7 and knowledge of the duration of individual organ or system changes can be helpful in distinguishing expected physiologic changes from pathologic complications. For example, Dorman and associates14 showed that interleukin-6, which contributes to postoperative fever,15 peaks at 24 hours but still is slightly elevated at 72 hours. So, although a postoperative fever of 38° C may be expected within the first 48 hours, prolonged fevers warrant further workup. Awareness of the surgical stress response can be helpful in diagnosing complications based on when they are most likely to occur. For example, catecholamines are increased for 24 to 48 hours following surgery and are associated with an increased incidence of myocardial infarction.16
A multimodal approach may help decrease complications related to the stress response through the use of techniques such as minimally invasive surgery, neural blocks with local anesthetics, intraoperative body heat conservation, early enteral nutrition and ambulation, and minimal use of surgical drains and nasogastric tubes.6 Adequate postoperative pain control may help attenuate the effects of the stress response.6 The authors use a simple regimen of scheduled acetaminophen and as-needed oxycodone to help control pain with few adverse effects. More severe pain can be treated with patient-controlled analgesia.
The Preoperative Evaluation
The preoperative evaluation, an important aspect of any surgical procedure, should assess the patient’s current medical status and provide risk identification, as well as recommendations to reduce risk. This evaluation also provides an opportunity to ensure that acute conditions/exacerbations are treated and chronic medical conditions optimized. The preoperative evaluation is not done to simply declare the patient “clear for surgery,” but is a multidisciplinary effort that includes input from the surgeon, the anesthesiologist, and possibly a medical consultant. The evaluation should be performed before the day of surgery for patients with very severe disease and for patients with less severe disease undergoing highly invasive surgical procedures.17
The history and physical examination serve as the cornerstone of the preoperative evaluation. Information should focus on pertinent past medical history, current review of systems/symptoms, physical examination findings (including airway evaluation), and current medications and drug allergies. The most important aspect of the history and physical is the cardiac assessment, which includes functional status. Patients with no acute illness or exacerbation who have good functional capacity with no cardiopulmonary symptoms can proceed directly with hip surgery.18 Patients with poor functional capacity require further evaluation and, depending on cardiac risk factors, may need preoperative cardiac stress testing if it will change management. Patients with no cardiac risk factors, even if they have poor or unknown functional status, can proceed directly with hip surgery.18
The preoperative evaluation should also include any recommendations for testing before surgery; preoperative tests should not be ordered routinely, but rather should be obtained for purposes of guiding or optimizing perioperative management.17 As emphasized in the American College of Cardiology/American Heart Association (ACC/AHA) 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery, “intervention is rarely necessary to simply lower the risk of surgery unless such intervention is indicated irrespective of the preoperative context.”18 The benefits of any testing or medical treatment must be weighed against the risks of delays in surgical treatment, especially for hip fracture patients requiring urgent surgery. Recent study results have been conflicting,19–25 but operative repair of hip fracture likely should be performed within 48 hours.
It is unclear which type of anesthesia—general or neuraxial (spinal or epidural)—leads to better outcomes following hip surgery. This topic remains controversial, and decisions about the specific type of anesthesia to be used should be made by the anesthesiologist.
History
Past Medical History and Review of Systems.
Review the patient’s known medical problems and assess each for optimization/stability, including new and chronic symptoms. A mnemonic (“The ABCs,” Box 26-1), adapted from guidelines taught at Mayo Clinic,26 can serve as a reminder of the most important questions to ask each patient.
Patients who need emergency surgery should proceed directly to the operating room with testing only as allowed by their clinical condition, such as vital signs and possible baseline laboratory tests (see later). On the other hand, patients who are undergoing elective hip surgery and who have an active cardiac condition should undergo evaluation and treatment before surgery is performed.18 Active cardiac conditions include unstable coronary syndromes, decompensated heart failure, significant arrhythmias (including high-grade atrioventricular block, symptomatic ventricular arrhythmias, supraventricular arrhythmias with ventricular tachycardia, and symptomatic bradycardia), and severe valvular disease such as severe aortic stenosis. Likewise, any symptoms suggestive of acute infection or disease exacerbation (e.g., asthma) also require further evaluation and treatment before elective surgery is undertaken.
Special attention should be given to the patient’s airway and to any previous anesthesia complications or adverse reactions. For patients with a history of penicillin allergy, consider referral for formal allergy consultation and penicillin skin testing if beta-lactam therapy is being considered. Always review the patient’s alcohol history, and be alert for alcohol withdrawal postoperatively. For patients who use tobacco products, smoking cessation 4 to 8 weeks before surgery is important to decrease the risk of postoperative complications.27–29 Of note, severe obesity (body mass index [BMI] ≥ 40 kg/m2) is not associated with increased mortality but is associated with increased length of hospital stay and greater likelihood of renal failure and prolonged assisted ventilation.30 Also, these patients have been found to require longer operating times for total hip arthroplasty.31
Physical Examination
A focused review of systems and a preoperative physical examination should be performed on all patients. Important findings that may require further evaluation are listed in the following sections.
Vital Signs.
Measure and document current vital signs, including temperature, blood pressure, heart rate and rhythm, respiratory rate and pattern, oxygen saturation, and height and weight.
Airway.
Patients with a small mouth, micrognathia, limited neck range of motion, or a poorly visualized posterior oropharynx (Mallampati class III or IV; as shown in Fig. 26-1) may be more difficult to intubate and establish an airway, so the anesthesiologist should be alerted to a potential “difficult airway.” Patients who are edentulous or who have a full beard may be difficult to oxygenate with a face mask, so these conditions should be noted as well.
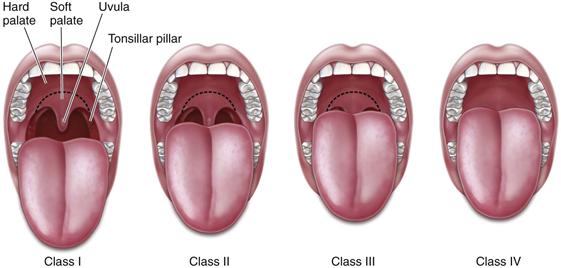
Figure 26-1 Mallampati Classification.
Class I: Full visibility of tonsils, uvula, and soft palate. Class II: Visibility of hard and soft palate, upper portion of tonsils, and uvula. Class III: Soft and hard palate and base of the uvula are visible. Class IV: Only hard palate visible.
Cardiac.
Ask patients if they have any chest pain/pressure or dyspnea at rest or with activity, palpitations, orthopnea, or syncope. Assess the heart rate and rhythm, paying particular attention to bradycardia or tachycardia and any irregularity that could indicate atrial fibrillation or a conduction block. Listen for significant cardiac murmurs. Aortic stenosis, which typically causes a harsh systolic murmur (occurring between the first and second heart sounds), poses the highest risk for noncardiac surgery; evaluation is required before surgery is undertaken. This murmur characteristically radiates to one or both carotid arteries. Note that the physical examination often underestimates cardiac dysfunction in severely obese patients (BMI ≥40 kg/m2).30
Respiratory.
Ask patients if they have dyspnea, cough with sputum, or wheezing, and whether these symptoms are baseline, worse than baseline, or new. Listen for inspiratory crackles (rales), which could indicate pulmonary edema or infection, and wheezes, which can be found in asthma, chronic obstructive pulmonary disease (COPD), and pulmonary edema. Patients with COPD commonly have decreased breath sounds and a prolonged expiratory phase of respiration.
Gastrointestinal.
Ask patients if they have nausea, vomiting, abdominal pain, constipation, or diarrhea. The abdomen should be soft, nontender, and nondistended with normal bowel sounds. Special note should be made of findings suggestive of liver disease, including ascites.
Vascular.
Look for evidence of elevated jugular venous pressure and lower extremity edema, which could indicate increased intravascular volume related to right heart failure. Diminished peripheral pulses may be due to peripheral vascular disease that could impair wound healing.
Neurologic/Psychiatric.
Any preexisting neurologic deficit should be documented, along with conditions such as a seizure disorder, dementia, or a history of delirium.
Skin.
Any skin ulcers should be documented and may need treatment before the time of surgery, particularly if evidence of infection is noted.
Functional Status
Patients who are highly functional and asymptomatic are at low risk for perioperative cardiac complications.18 Functional status is quantified in terms of metabolic equivalents (METs), as shown in Table 26-1.
Table 26-1
Metabolic Equivalents (METs) for Various Physical Activities
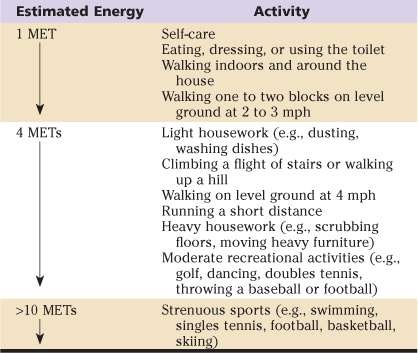
MET, Metabolic equivalent; mph, miles per hour.
Adapted from Fleisher LA, Beckman JA, Brown KA, et al: ACC/AHA guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 116:e425, 2007.
Patients who can achieve at least 4 METs without cardiopulmonary symptoms have adequate functional capacity and may proceed directly to hip surgery without preoperative cardiac testing, assuming no acute symptoms.
However, it is often difficult to estimate functional capacity in orthopedic patients, who may have joint pain that limits ambulation. In this case, ask about other activities as listed in Table 26-1,18 such as the ability to perform housework. Patients who cannot achieve 4 METs should be further assessed in terms of clinical cardiac risk factors derived from the Revised Cardiac Risk Index (diabetes mellitus treated with insulin, chronic kidney disease with creatinine greater than 2, ischemic heart disease, cerebrovascular disease, or heart failure).
Patients with no cardiac risk factors may proceed directly to hip surgery without preoperative cardiac testing, assuming no acute symptoms.
Consideration can be given for preoperative cardiac testing in patients with at least one risk factor if it will change management, or if the patient would need testing independent of hip surgery.18 Always ask whether a patient has had a recent cardiac stress test, especially if he or she is nonambulatory or is minimally active. Certain patients may benefit from starting a beta blocker, as discussed in the section, “Current Controversies and Future Directions.”
Current Medications
Obtain an accurate list of all medications, dosing, and schedules, including over-the-counter and herbal medications. In general, most prescription medications should be continued perioperatively, especially drugs with known withdrawal syndromes (such as beta blockers, clonidine, or benzodiazepines), and should be taken with sips of water on the morning of surgery. However, certain drugs should be held the morning of surgery, and herbal medications should be held for at least 1 week because of possible drug-drug interactions with anesthetic agents and concerns for increased bleeding risk (among others, bleeding can be potentiated by the “G” herbal medications: garlic, ginger, ginkgo biloba, and ginseng).32 Aspirin and clopidogrel each can increase the risk of surgical bleeding, but they provide essential treatment for patients with a recent coronary stent (especially drug-eluting stents) and may be given for other indications, including stroke. In cases in which aspirin and clopidogrel must be stopped because of high risk of surgical bleeding, aspirin should be held for 7 to 10 days and clopidogrel for 5 to 10 days before surgery. However, because of the high mortality associated with in-stent coronary thrombosis, the surgical team should consult with a cardiologist for patients with recent coronary stent placement (within 1 year for drug-eluting stents) before these medications are stopped. If clopidogrel must be stopped, aspirin should be continued if at all possible.
Table 26-2 provides suggestions regarding which medications should be taken and which should be held the morning of surgery.32,33 Some of these recommendations are based on expert opinion at the authors’ institution, and practitioners should be aware of local preferences and recommendations.
Table 26-2
Recommendations for Medication Dosing the Morning of Orthopedic Surgery
| Drug Class | Take | Hold |
| Cardiac | Beta blockers | Diuretics |
| α2-Agonists (e.g., clonidine) | ACE inhibitor1 | |
| Calcium channel blockers | ARB1 | |
| Digoxin | Fibrates (hold the night before) | |
| Isosorbide mononitrate and dinitrate | Niacin (hold the night before) | |
| Statins | ||
| Pulmonary | Nebulizer/MDI | |
| Leukotriene inhibitors | ||
| GI | Proton pump inhibitors | |
| H2-blockers | ||
| Stool softeners | ||
| GU | α1-Antagonists (e.g., tamsulosin) | Tolterodine |
| Oxybutynin | ||
| Endocrine | Levothyroxine | Sulfonylureas |
| Corticosteroid2 | Metformin3 | |
| Insulin4 | ||
| Thiazolidinediones | ||
| Hormone replacement therapy (hold 4 weeks preop) | ||
| Psychiatric | SSRI unless high bleeding risk | MAOI (hold 2 weeks preop5) |
| Benzodiazepines | ||
| Tricyclic antidepressants | ||
| Antipsychotics | ||
| Lithium | ||
| Neurologic | Antiepileptic drugs | |
| Carbidopa/levodopa5 | ||
| Rheumatologic | Methotrexate6 | Leflunomide (hold 2 weeks preop) |
| Hydroxychloroquine | ||
| Azathioprine | ||
| Sulfasalazine | ||
| NSAIDs | (hold 3 days preop) | |
| Pain | Opioids | |
| NSAIDs | ||
| Tylenol |
ACE, Angiotensin-converting enzyme; ARB, angiotensin receptor blocker; GI, gastrointestinal; GU, genitourinary; MAOI, monoamine oxidase inhibitor; MDI, metered dose inhaler; NSAID, nonsteroidal anti-inflammatory drug; SSRI, selective serotonin reuptake inhibitor.
1Hold if the indication is hypertension and current blood pressure is <140/90, or if the indication is heart failure.
2Patients taking long-term steroids may benefit from perioperative stress-dose steroids.
3Metformin should be held starting 1 day before surgery and resumed on postop day 2 to 3, assuming adequate kidney function and no heart failure exacerbation.
4Insulin dose should be adjusted the morning of surgery, depending on time of day and duration of surgery; typically one-half the usual morning dose is given for patients taking NPH insulin, and the usual dose of glargine is given the night before surgery.
5Discuss with the anesthesiologist; it may be safe to continue.
6Methotrexate should be held for 2 weeks preoperatively in patients with chronic kidney disease, but otherwise should be continued.
Preoperative Testing
Preoperative testing should be limited to those tests that may change the risk of surgery, especially if the underlying disease can be treated, or that provide a baseline that will be used to monitor a clinical condition or treatment perioperatively. Because of the risk of false-positive results or minor abnormalities that will not influence surgical outcome, tests should be ordered selectively rather than routinely. Indications for tests should be documented, and any abnormal test result must be addressed. Laboratory tests obtained within the previous 4 months should safely provide adequate information unless there is an interim change in clinical status34 or in medications that could affect electrolytes has occurred.
Laboratory Tests.
A complete blood count (CBC) with hemoglobin, white cell count, and platelet count should be obtained in patients with a history or symptoms of anemia or infection or a history of bleeding diathesis, or if the surgical procedure may lead to blood loss requiring a transfusion. A baseline platelet count may be helpful for patients who will be on heparin perioperatively. Kidney function (creatinine) should be checked in all persons undergoing hip surgery. Electrolytes should be checked in patients with chronic kidney disease or heart failure, and in those taking digoxin or medications that affect electrolytes, such as diuretics, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs). An international normalized ratio (INR) can be obtained in persons on warfarin therapy and in those with a history of bleeding diathesis, liver disease, or malnutrition. Low albumin is predictive of 30-day mortality35; therefore, albumin should be measured if it is likely to be low, such as in patients with liver disease or malnutrition, given that oral protein and calorie supplementation may be of benefit in hip fracture patients.36 Fasting glucose should be checked in diabetic individuals and in persons at high risk for diabetes. A pregnancy test should be considered for all female patients of childbearing age. Urinalysis and culture should be checked in patients with symptoms of a urinary tract infection who will have a prosthetic hip implant.
Electrocardiogram.
Obtain a preoperative electrocardiogram (ECG) in patients with a history of coronary artery disease (CAD), peripheral arterial disease, or cerebrovascular disease undergoing intermediate-risk procedures such as hip surgery.18 It is also reasonable to obtain an ECG for severely obese patients.30 Consideration can be given to an ECG for persons with risk factors for coronary disease or for asymptomatic men over 40 years old and women over 50 years old.
Chest X-rays and Spirometry.
These tests should not be used routinely for predicting risk for postoperative pulmonary complications, but they may be appropriate in patients with a previous diagnosis of COPD or asthma,37 and they may be helpful in assessing the status of known lung disease, especially when the history and physical examination do not lead to a firm conclusion.38 It is also reasonable to obtain a chest x-ray for severely obese patients.30
Cervical Spine X-rays.
Patients with long-standing rheumatoid arthritis have a high prevalence of cervical spine subluxation.39 These patients, as well as those with ankylosing spondylitis or Down syndrome, should have preoperative flexion and extension x-rays of the cervical spine to look for evidence of subluxation or other instability.
Risk Reduction and Medical Optimization
Identification of risk factors for postoperative complications can help guide preoperative evaluation and risk reduction strategies. Likewise, it is important to assess each patient’s history and symptoms before surgery to help determine whether a new, acute process or an exacerbation of a chronic illness is under way. Patients undergoing surgery should be at their best baseline regarding comorbid medical conditions, functional status, and nutritional status. This does not mean that each chronic condition must be “cured,” but if an acute process or exacerbation is present, elective procedures may need to be deferred. On the other hand, for urgent procedures such as repair of hip fracture, the important question is whether surgery should be delayed (and for how long) to allow medical optimization.
Memtsoudis and associates found that advanced age is the single most important risk factor for postoperative complications following hip and knee arthroplasty,40 along with comorbid medical conditions. Bhattacharyya and colleagues identified five preoperative medical risk factors for inpatient mortality after any orthopedic surgery: chronic renal failure, congestive heart failure, COPD, hip fracture, and patient older than 70 years.41 Maxwell and colleagues42 noted a number of independent predictors of 30-day mortality for hip fracture patients: age older than 65 years, male sex, at least two comorbidities, low mini-mental test score, admission hemoglobin concentration less than 10 g/dL, living in an institution, and the presence of malignant disease.
Cardiac
Postoperative cardiac complications include myocardial ischemia/infarction, congestive heart failure, hemodynamic instability, and arrhythmias. The key points are to distinguish acute or unstable conditions from those that are chronic and stable, and to estimate a patient’s risk of severe cardiac disease.
Risk Factors
Approximately 30% of adults undergoing surgery each year in the United States have CAD or risk factors such as advanced age, male gender, hypertension, hypercholesterolemia, diabetes mellitus, cigarette smoking, obesity, sedentary lifestyle, family history of premature CAD (men younger than 55 and women younger than 65 years old), and psychosocial stress.43
Recommendations
• Consider the use of continuous epidural analgesia, which is associated with a lower incidence of adverse cardiac events in at-risk elderly patients with hip fracture.44
• Be vigilant for withdrawal syndromes that may lead to increased cardiac stress.
• Any unstable patient should be hospitalized preoperatively for evaluation and treatment.
Pulmonary
Postoperative pulmonary complications include atelectasis, hypoxemic or hypercarbic respiratory failure, pneumonia, COPD exacerbation, aspiration, and prolonged mechanical ventilation.
Risk Factors
Patient-related risk factors include COPD, age older than 60 years, American Society of Anesthesiologists (ASA) class II or greater, functional dependence, congestive heart failure, and a low serum albumin level (<35 g/L).37 Use of cigarettes is associated with a modest increase in risk, but obesity and mild to moderate asthma are not associated with increased pulmonary risk.37 Although most orthopedic procedures are not as high risk for postoperative pulmonary complications as aortic, thoracic, or upper abdominal surgery, factors such as prolonged surgery (>3 hours) do increase risk.45 Risk factors for aspiration, which occurs in up to 0.01% to 0.06% of anesthetized patients at the time of anesthesia induction and intubation, include advanced age, gastroesophageal reflux disease (GERD)/hiatal hernia, obesity, pregnancy, and conditions such as diabetes that may predispose to delayed gastric emptying.46 Of note, aspiration related to anesthesia induction or intubation may lead to pulmonary complications, but complications are unlikely if no signs or symptoms are seen within 2 hours of the aspiration event.47
Obstructive sleep apnea (OSA) is another risk factor that may lead to hypoxemia, hypercarbia, and cardiovascular dysfunction. Patients with OSA may have difficulty with airway management, including intubation. A presumptive diagnosis of OSA can be made in patients with obesity (BMI ≥35 kg/m2), large neck circumference (>17 inches [43 cm] in men or 16 inches [40.6 cm] in women), snoring, congenital airway abnormalities, daytime hypersomnolence, inability to visualize the soft palate, and tonsillar hypertrophy.48
Recommendations
• Patients who smoke should quit at least 4 to 8 weeks before surgery.27–29
• Patients with acute respiratory symptoms such as chest tightness or wheezing should be given aggressive bronchodilator therapy with the option of preoperative systemic corticosteroid therapy. A short course of steroids is unlikely to increase perioperative infection risk or to hinder wound healing.49
• Patients with evidence of a pulmonary infection may need treatment with antibiotics.
• Postoperative epidural pain control has been shown to reduce the risk of pulmonary complications.50
• Patients with suspected OSA ideally should undergo evaluation long enough before scheduled surgery for the clinician to develop a perioperative management plan, including possible formal polysomnography. Preoperative initiation of continuous positive airway pressure (CPAP) should be considered for these patients, although the literature is insufficient to evaluate its impact.48
• Patients with suspected OSA should have continuous pulse oximetry while in bed for as long as they remain at increased risk. These patients should be given supplemental oxygen until they are able to maintain their baseline oxygen saturation while breathing room air.48
Gastrointestinal
Gastrointestinal complications following hip surgery include postoperative nausea and vomiting (PONV), postoperative ileus (POI), and acute colonic pseudo-obstruction (Ogilvie’s syndrome).
Risk Factors
Risk factors for PONV include female sex, prior history of PONV or motion sickness, nonsmoking status, prolonged surgery, volatile anesthetics or nitrous oxide, and intraoperative or postoperative opioid use.51 Pain, anxiety, and dehydration may also increase the incidence of PONV.52 Risk factors for POI include the surgical stress response (sympathetic hyperactivity, systemic endocrine response, and production of endogenous opioids and inflammatory cytokines), increased surgical blood loss (possibly contributing to a heightened inflammatory response), and factors related to perioperative care, such as general anesthesia and the use of opioid medications.53 Preexisting gastrointestinal disease such as Crohn’s and decreased perioperative physical activity can contribute to POI, which can cause abdominal symptoms and increased hospital length of stay.54 Significant risk factors for acute colonic pseudo-obstruction include advanced age, male sex, and medications that affect bowel motility (including opioids, phenothiazines, tricyclic antidepressants, calcium channel blockers, H2-receptor blockers, and anticholinergics).55 Slow postoperative mobility and revision hip arthroplasty were also found to be significant risk factors in a study by Petrisor and associates.56 Other risk factors may include prior abdominal surgery, hypothyroidism, diabetes mellitus, and preexisting gastrointestinal disease.55
Patients with known liver disease deserve special mention given their increased risk of perioperative complications and mortality. Acute hepatitis (viral or drug-induced) may present with symptoms of nausea, vomiting, anorexia, jaundice, and dark urine. Elective surgery should be deferred until patients demonstrate symptomatic and biochemical improvement. Patients should be advised to avoid strenuous activity, alcohol, and acetaminophen. Chronic liver disease is often diagnosed before surgery is performed, but it may present undiagnosed with fatigue, malaise, abdominal pain, and abnormal liver tests, especially in advanced disease and cirrhosis.57 Patients are at high risk for early complications58 and limited prosthesis longevity.59 Surgery should be delayed in patients with decompensated cirrhosis, which may manifest with encephalopathy and/or ascites.
Recommendations
• Give patients at high risk for PONV one or more antiemetics, such as droperidol, metoclopramide, ondansetron, cyclizine, or dexamethasone, before or during anesthesia.60 A single preoperative dose of dexamethasone 40 mg intravenous (IV) was shown to decrease PONV in a small study of total hip arthroplasty patients without causing adverse outcomes, including wound complications, deep infection, or osteonecrosis in the contralateral hip.61 However, even with multiple drug treatment, more than 30% of high-risk patients had postoperative emetic symptoms in a large prospective observational study.62
• Apply P6 acupoint stimulation in patients at risk for PONV. (The P6 acupoint is located between the tendons of the palmaris longus and flexor carpi radialis muscles, 4 cm proximal to the wrist crease.63)
• Although it has been reported that “little can be done preoperatively to reduce the risk for POI,”54 the medical team should strive to minimize both the surgical stress response and opioid medications as tolerated.
• Medical conditions associated with acute colonic pseudo-obstruction should be optimized.
• Patients with advanced liver disease may require perioperative evaluation by a gastroenterologist.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








