Periacetabular Osteotomy for the Treatment of Symptomatic Acetabular Dysplasia
Robert T. Trousdale
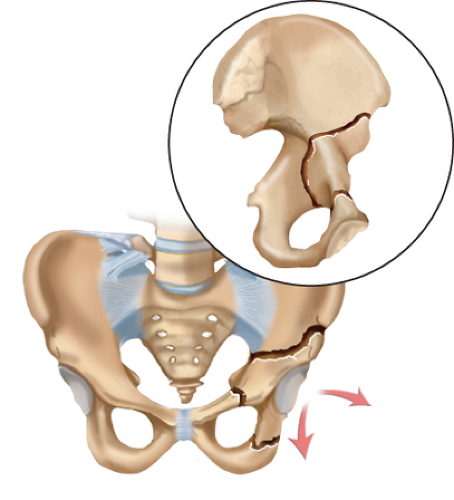
The Bernese periacetabular osteotomy (PAO) has become the procedure of choice in many centers for the treatment of young patients with symptomatic hip dysplasia in the absence of severe secondary arthritis. Patients with classic developmental hip dysplasia typically have varying degrees of anatomic abnormalities. On the acetabular side, the joint socket is usually shallow, anteverted, lateralized, and femoral head coverage is deficient anteriorly and superiorly. The version status of the acetabulum occasionally is retrotorted in up to 25% of the acetabula. On the femoral side, the head can be small, the neck–shaft angle is typically increased, and the femoral canal is narrow. These structural abnormalities lead to decreased contact between the femoral head and the acetabulum and increased body weight lever arm from excessive lateralization of the hip center of rotation. Relatively high forces are transmitted through this decreased surface area, which can lead to secondary degenerative joint disease over time. Retroversion of the acetabulum has become increasingly recognized for the past 10 years as a potential source of hip discomfort. It is defined as a posteriorly oriented acetabular opening referenced to the sagittal plane and can be seen as an isolated entity or associated with classic hip dysplasia, as mentioned. It also is seen after injury to the triradiate cartilage in a child or in association with bladder exstrophy or Legg–Calvé–Perthes disease. Those patients with retrotorsion in the presence of posterior wall deficiency are good candidates for anteversion PAO. Younger patients with hip dysplasia without marked degenerative joint disease should still rely on nonarthroplasty options to help control pain and hopefully retard the progress of arthritic changes. Multiple different types of osteotomies have been developed to improve symptoms and joint mechanics in young patients with symptomatic hip dysplasia. In 1992, we began using the Bernese PAO because of its balance between minimal exposure, acceptable complication rate, and the ability to provide optimal correction of the dysplastic hip (Fig. 32.1). Its advantages are multiple and have been well described. It can be performed through one incision without major violation of the abductors; the pelvic ring and outlet are not disrupted which allows for early mobilization. There is no need for postoperative immobilization, and it allows for future vaginal delivery without complication in women. Furthermore, it allows optimal correction both medially, laterally, and version changes as needed. One can also perform a capsulotomy to check for impingement and the status of the labrum without markedly compromising acetabular blood supply.
In our mind, the ideal patient for a reconstructive pelvic osteotomy is one who is relatively young, has minimal secondary arthritic changes, and has a poorly covered femoral head. The socket and femoral head should be relatively round with the ability to obtain a congruent hip after correction.
Surgery
The majority of our patients have this procedure done under regional epidural anesthesia. We have abandoned the use of preoperative autologous blood donation as intraoperative cell saver appears very helpful in minimizing the need for allogeneic blood. Presently our allograft transfusion rate is less than one in five patients.
The patient is placed on an image table. A Foley catheter is inserted. We use intraoperative EMG monitoring of the sciatic nerve and femoral nerve to minimize the chance of permanent neurologic injury (Fig. 32.2). In 1992, we began performing the procedure using an anterior incision with exposure of both the inner and outer tables of the pelvis. In 1996, we began utilizing the same skin incision performing the osteotomy only through the inner aspect of the pelvis leaving the abductors intact on the outer aspect of the ilium. We feel this has dramatically improved the rate of healing, the time allowable to weight bearing, and the resolution of the postoperative limp. The incision typically begins along the border of the iliac crest and proceeds along the anterior superior iliac spine and continues distally ending approximately 3 cm distal and anterior to the greater trochanter. The plane between the tensor fascia lata and sartorius is developed, incising the deep fascia over the tensor fascia lata, avoiding direct injury to the lateral femoral cutaneous nerve. The sartorius origin is reflected from the anterior superior iliac spine, the hip is flexed, adducted, and the inner table of the pelvis is exposed to the sciatic notch. The pubis is then exposed by retracting the iliopsoas tendon medially and a Hohmann retractor is placed in the pubic bone. The direct head of the rectus is reflected distally from the anterior inferior iliac spine exposing the anterior hip capsule. Using blunt dissection, one proceeds distally and medially, and under image intensifier a scissors is used to palpate the ischium and obturator foramen.
Performing the osteotomies has become relatively routine with the aid of an image intensifier. We use image intensifier at four critical points during the performance of the osteotomies. We perform the ischial osteotomy initially, and an anteroposterior image is used to assure the osteotomy is distal and medial enough and oriented in the proper direction (Fig. 32.3). The ischial osteotome is left in place as a guide when performing the last osteotomy (the posterior iliac osteotomy). Often one can palpate this osteotome medially and distally over the quadrilateral surface. We then expose the pubic bone using Hohmann retractor, check with image intensifier to make sure we are medial enough which will prevent entry of the osteotomy into the joint. The pubic osteotomy is performed in an oblique fashion, proximal medial to distal lateral, which facilitates mobilization of the fragment. The iliac cut is typically performed just at the level just distal to the anterior superior iliac spine, but an AP image is obtained to make sure one is high enough above the joint to allow satisfactory fixation of the distal fragment. It is often helpful to orientate the iliac cut slightly distal to make sure that when the iliac cut is turned to connect with the ischial cut one is distal to the top of the sciatic notch. The image intensifier really becomes helpful with the last osteotomy (Fig. 32.4). We get a 45-degree oblique x-ray showing the posterior column of the acetabulum, and one can make sure the posterior osteotomy is extra-articular as well as not to violate the posterior column of the pelvis. Once the cuts are made the fragment is mobilized. Occasionally the “corners” of the cuts can impinge or catch, limiting mobilization. One has to be careful not to hinge the fragment with correction. This error is easily detected both by palpation as well as radiographically. The acetabular teardrop should flip radiographically, proving that the fragment is not hinging. If one is hinging posteriorly and inferiorly, this corner of the fragment can be trimmed with an osteotome or rongeur, and will facilitate mobility of the fragment. When all three osteotomies are completed in the proper location, the posterior column should be left intact, and the acetabular fragment should be free and mobile.
 Figure 32.2. Intraoperative photograph showing EMG monitor and fluoroscopy in place. This patient’s left hip is the operated side. |
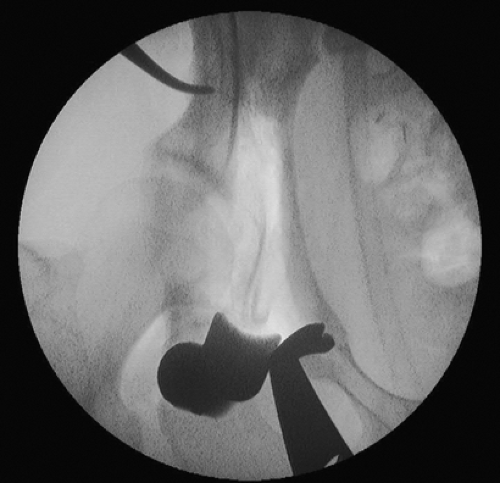 Figure 32.3. Intraoperative fluoroscopy showing placement of ischial osteotome. A Hohmann retractor is in the lateral aspect of the pubic bone. |
The most difficult part of the operation is obtaining proper correction. We presently think of the proper correction in four different steps: Proper medialization of the hip




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree