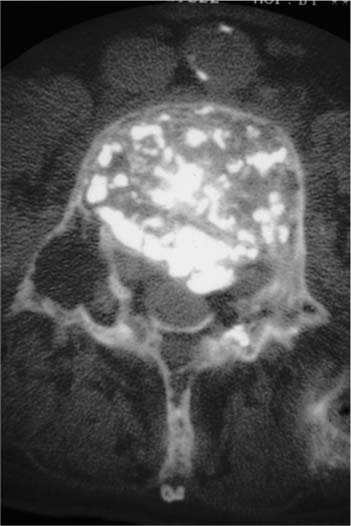
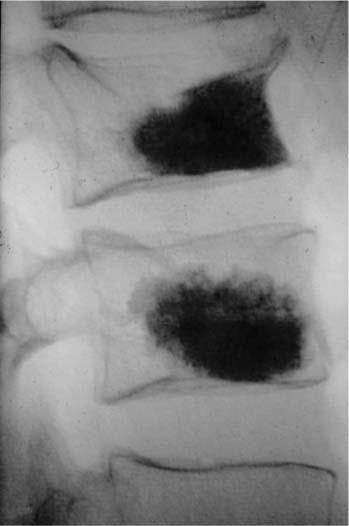
Chapter 32 Percutaneous vertebroplasty (PVP) using polymethylmethacrylate cement (PMMA) consists of injecting PMMA into the vertebral body by a percutaneous route to provide strength and support.1 The bone cement is injected into the vertebrae under Xray guidance using a hollow needle, and the PMMA hardens within 15 minutes. First described in 1987 by Pierre Galibert and coworkers,2 this technique has found increasing recognition and is now used worldwide in several diseases involving the spine, including vertebral metastatic diseases,3–5 nondegenerated hemangiomas,6–8 and vertebral osteoporotic fractures.9–11 PMMA is well known among orthopaedic surgeons who have used this acrylic cement for joint prosthesis fixation since the work of Charnley 40 years ago.12 More recently PMMA has been used in spine stabilization for metastatic diseases13–15 and for the treatment of hemangiomas16 and giant cell tumors.17 The use of PMMA by a percutaneous route for the treatment of hemangiomas was pioneered by Galibert and colleagues in 1984. They added tantalum powder to the PMMA powder to obtain a good radiopacity of the cement when using fluoroscopic guidance. The first description of this technique was published in 1987,2 then several French teams made use of it in the next few years especially in Lyon,3,18,19 Lille,4,7,8,11 and Paris,5 with the Lyon group using some minor modifications such as injection under computed tomography (CT) scan, rather than under fluoroscopic guidance. Initially the aim of PVP was to strengthen the vertebral body weakened by an aggressive hemangioma. Thereafter the method was extended to other weakening lesions such as vertebral myeloma, osteoporotic crushed fractures, or metastatic lesions. Today the technique is used worldwide, several thousand PVP procedures have been performed, and many hospitals are giving information about PVP on their web sites. Radiography and CT must be performed in the days preceding vertebroplasty to assess the extent of vertebral collapse, the location and extent of the lytic process, the visibility and degree of involvement of the pedicles, the presence of cortical destruction or fracture, especially of the posterior wall, and the presence of epidural or foraminal stenosis caused by tumor extension or bone fragment retropulsion. These assessments may influence the way the procedure is performed, but none is an absolute contraindication for vertebroplasty. The presence of cortical destruction or epidural or foraminal stenosis should lead to the exercise of extreme caution during cement injection to prevent new or further neurologic compression. Vertebroplasty is usually performed under antero-posterior and lateral fluoroscopic guidance, although some authors have emphasized the use of CT for needle positioning or injection assessment.20,21 General anesthesia or neuroleptanalgesia is needed because pain may intensify during cement injection. Ten- or fifteen-gauge needles are frequently used for cement injection, with the diameter and length of the needles chosen depending on the spinal level involved. However, the use of thinner needles has been reported. The choice of needle route depends on the experience of the radiologist. For the cervical spine, although some radiologists prefer transpedicular injections,20 anterolateral access is frequently performed. The fingers are placed in such a way as to push the large vessels laterally, and the needle is advanced between the vessels and the pharyngolarynx. Either transpedicular or posterolateral route is used for the thoracic and lumbar spine. The transpedicular route avoids spinal segmental nerve injury and decreases the risk of leakage of PMMA into the paravertebral tissue. However, this access is not possible when osteolysis involves the pedicles and does not allow their adequate visualization under fluoroscopic guidance. The posterolateral route is easy to perform for the lumbar spine but is more difficult for the thoracic spine due to the risk of pneumothorax. When the needle is in the desired location, methylmethacrylate polymer (20 mL powder, 5 to 7 mL solvent) is mixed with tungsten powder (2 g) or barium powder20 to increase its radiopacity. The viscosity of the mixture progressively increases due to polymerization of the methylmethacrylate. The main difficulty at this point is choosing the appropriate viscosity of the cement to be injected. A paste consistency is preferred to a liquid consistency as the latter may result in leakage of methylmethacrylate into adjacent structures. The methylmethacrylate is then injected until resistance is met or until cement reaches the posterior wall. However, injection is stopped immediately if epidural, foraminal, or venous leakage is detected at fluoroscopic guidance. This initial access usually allows an injection of 2 to 9 mL of cement. Depending on the distribution of cement in the vertebral body, one or more injections may be performed. The distribution of methylmethacrylate is frequently homogeneous in hemangiomatous or osteoporotic vertebral bodies, and a single injection may be sufficient. The degree of lesion filling is much more varied in cases of metastatic and myelomatous lesions, probably because of the different texture of these lesions. The procedure usually lasts from 1 to 2 hours unless cement is injected into two or more vertebral bodies. CT, which allows assessment of vertebral body filling and depicts leakage of methylmethacrylate, must be performed in the hours following cement injection. Osteolytic metastases and myelomas (Fig. 32–1) constitute the main indications for vertebroplasty, as patients usually experience severe pain that is frequently resistant to drug treatment. Vertebrectomy followed by strut grafting or intraoperative use of methylmethacrylate is rarely undertaken because of the multifocal nature of the disease. Radiation therapy affords partial or complete pain relief in more than 90% of the patients after a delay of 10 to 20 days, but results in minimal, delayed (2 to 4 months after the start of irradiation) bone strengthening, which is usually more effective in patients with myeloma than in those with metastases. However, this delay in bone reconstruction increases the risk of vertebral collapse and consequently of neural compression. FIGURE 32–1 Patient with multiple myelomas. Anteroposterior control radiograph shows satisfactory filling of L2 vertebral body. Some studies have reported the effect of vertebroplasty in patients with osteolytic metastases and myeloma. In studies of 101,22 37,4 and 335 patients, complete or marked pain relief was obtained in 80, 68, and 73% of the patients, respectively. Pain relief occurred within hours or days (mean 24 hours) after the procedure. Only 2.5 to 6% of the patients demonstrated no improvement in pain. It also may be hypothesized that vertebroplasty provides bone strengthening, preventing new or further collapse of the vertebral body, as cement hardens as polymerization occurs. This has to be confirmed, however. Vertebral hemangiomas (Fig. 32–2) are common benign lesions of the spine that are often asymptomatic and discovered incidentally during radiologic evaluation. Rarely, they may be painful, and there must be a close correlation between clinical findings and radiologic features to ensure that the patient’s pain is due to the vertebral hemangioma. In such cases, vertebroplasty is performed to provide pain relief. In 38 painful hemangiomas, Deramond et al22 reported a disappearance of the pain in more than 90% of the cases. FIGURE 32–2 Patient with vertebral hemangioma of L4. Computed tomography (CT) scan shows a leak of methylmethacrylate into the epidural space. FIGURE 32–3 Patient with osteoporotic vertebral collapses. Two vertebral bodies were treated during the same procedure. Exceptionally, vertebral hemangiomas are aggressive and result in spinal cord or nerve root compression. Decompressive surgery such as laminectomy or excision of epidural hemangioma (when present) is usually required, generally preceded by vertebroplasty, which may obviate more aggressive surgery. Methylmethacrylate is then injected for pain relief, bone strengthening, and direct embolization of the hemangiomatous body. This combination approach may be preceded by embolization of arteries feeding the vertebral hemangioma or used in conjunction with other percutaneous injections.6–8,22,23 Osteoporotic vertebral compression fractures (Fig. 32–3) are common, occurring in 16% of post-menopausal women (i.e., with a frequency comparable with the two other main osteoporotic fractures, wrist and hip fractures). Vertebral fractures are usually responsible for back pain, disability, and decreased height.24 Conservative therapy including bed rest, analgesics, calcitonin therapy, and sometimes external bracing are usually sufficient for control of pain. However, in some cases, despite these treatments, vertebral fractures are responsible for persistent and debilitating pain. Due to the high benefit/risk ratio of percutaneous vertebroplasty with PMMA in both vertebral hemangiomas and metastatic neoplasms, this procedure has been proposed in osteoporosis. The results of vertebroplasty in osteoporosis are summarized in Table 32–1. To our knowledge the first authors reporting the interest of vertebroplasty in osteoporosis were Lapras et al.19
PERCUTANEOUS VERTEBROPLASTY
USING BONE CEMENT FOR
COMPROMISED VERTEBRAL BODIES
CHRONOLOGICAL ACCOUNT OF VERTEBROPLASTY
PERCUTANEOUS VERTEBROPLASTY TECHNIQUE
RADIOLOGIC ASSESSMENT
PROCEDURE
INDICATIONS
OSTEOLYTIC METASTASES AND MYELOMAS
VERTEBRAL HEMANGIOMAS
VERTEBRAL COMPRESSION FRACTURES DUE TO OSTEOPOROSIS
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree