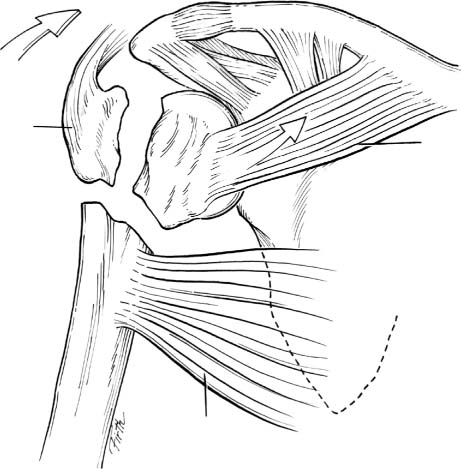
5 Percutaneous Pinning of Proximal Humeral Fractures Proximal humerus fractures are common and occur at a rate of 4 to 5% of all fractures. This rate has increased since the 1970s and is expected to continue to rise. The major risk factors are old age, female gender, and osteoporosis.1 The vast majority (85%) of these fractures are not displaced or minimally displaced and can be treated with nonoperative means. The remaining 15% present a challenge to the clinician in terms of the best treatment option. There are many surgical options including open reduction and internal fixation with locked or nonlocked plates, tension-band wiring, intramedullary nail fixation with solid or flexible nails, humeral head replacement, and percutaneous reduction and pinning. Hagg and Lundberg2 reported a doubling of the rate of avascular necrosis with open reduction. The advantages of percutaneous pinning include decreased soft tissue stripping and a decreased risk of vascular compromise to the fracture fragments. In addition, there is less adhesion formation with closed reduction, which makes any subsequent revision surgery easier secondary to decreased scarring. The major disadvantages are technical difficulty and risk to neurovascular structures around the proximal humerus. These risks can be decreased with strict attention to anatomic principles, careful dissection, and soft tissue protection during placement of hardware. It is important to perform a thorough history and physical examination when the patient first presents to the office or emergency room. Most patients are elderly and may have other comorbid conditions, which may help guide the physician to an operative or nonoperative course. The preinjury functional level of the patient is important to assess and may help guide expected outcomes. The surgeon must document a complete neurologic and vascular assessment of the extremity preoperatively. Axillary artery and nerve dysfunction is common after proximal humerus fractures and may prolong the recovery time.3 It is important to assess both the sensory as well as the motor function of the axillary nerve. Injuries to the axillary artery may not present with a dysvascular limb secondary to the vast collateral circulation around the shoulder. If a vascular injury is suspected, an angiogram should be performed. An electromyogram (EMG) should be obtained at 3 weeks postinjury if a patient has any residual neurological symptoms. Standard radiographic evaluation includes an anteroposterior (AP) and lateral (Y-view) in the plane of the scapula as well as an axillary view. This shoulder trauma series is usually sufficient to determine the fracture configuration. If the fracture pattern cannot be determined from plain films, computed tomography (CT) with reconstructions may aide in the determination of the position and displacement of the fracture fragments. Fractures are classified using the Neer system, which describes the fracture as the number of parts that are displaced 10 mm or angulated 45 degrees. Greater than 5 mm of superior displacement of the greater tuberosity has recently been felt to require reduction and fixation, especially in younger, active patients. The majority of two-part fractures have surgical neck displacement. Isolated fractures of the greater or, less commonly, the lesser tuberosity also occur. Three-part fractures have a displaced surgical neck component as well as a displaced fracture of either the greater or lesser tuberosity. In a classic four-part fracture-dislocation both tuberosities are separated from the dislocated head and the shaft. Valgus-impacted four-part fractures are a specialized subset of four-part fractures because they usually have a medial periosteal sling, which connects the head fragment to the shaft and preserves the ascending branches of the anterior and posterior circumflex arteries to the head.4 This periosteal hinge also aids in reduction of the fragments via ligamentotaxis. The head segment itself is fragmented in the “head splitting” fractures. Fracture fragment displacement varies depending on the fracture configuration. The deforming forces around the shoulder include the subscapularis, which will displace a lesser tuberosity or head fragment medially. The supraspinatus, infraspinatus, and teres minor will displace the head or greater tuberosity fragment superiorly and posteriorly. The pectoralis major will medialize the proximal aspect of the humeral shaft with respect to the head. Understanding these deforming forces will facilitate proper reduction based on fracture configuration (Fig. 5–1). Figure 5–1 Deforming forces on proximal humeral fracture fragments include the pectoralis major pulling the humeral shaft medially, the subscapularis pulling the lesser tuberosity medially, and the supraspinatus, infraspinatus, and teres minor displacing the greater tuberosity fragment superiorly and posteriorly. The majority of fractures can be treated nonoperatively with short-term immobilization followed by range of motion (ROM) exercises once the fracture begins to heal. Most displaced fractures will require reduction and operative fixation. Although closed reduction and percutaneous fixation is a good treatment for two- and three-part displaced fractures, other methods can be effective, including intramedullary rods, fixed-angle plates, and tension-band wiring. Percutaneous repair is especially well suited, however, to the treatment of impacted-valgus four-part fractures, as the reduced soft tissue stripping leads to a lower rate of avascular necrosis compared with open treatment.2 Minimally invasive repair also leads to less stiffness and reduced adhesions, making revision, if needed, easier. Classic four-part fracture-dislocations generally require humeral head replacement given the high rate of avascular necrosis due to the disruption of the blood supply to the humeral head. Fractures with severe comminution or patients with osteoporotic bone are not ideal candidates for percutaneous pinning. Head splitting fractures usually require arthroplasty given the high rate of avascular necrosis and posttraumatic arthritis. The results of revision hemiarthroplasty after failed open reduction are poorer than for primary arthroplasty for fracture.5
Patient Assessment
Treatment
Nonsurgical Treatment
Surgical Treatment
Technique for Percutaneous Pinning
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree