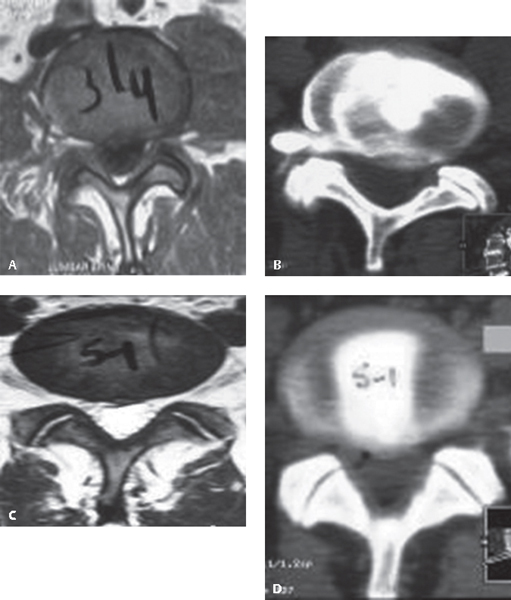
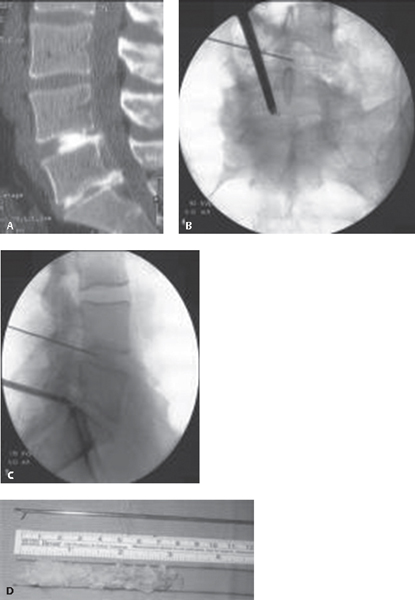
61 Low back pain is one of the most commonly encountered problems in a medical practice. Discogenic low back pain, or pain arising from the intervertebral disks, has been called the most common cause of chronic low back pain. Historically, surgical solutions were initially open, traumatic approaches that were associated with significant morbidity. Driven in part by the desire of patients and physicians to reduce the morbidity of spinal procedures, less-invasive approaches have grown significantly in popularity in recent years.1 There is a growing need for clearer language that can differentiate between the various “minimally invasive” procedures. A purported advantage of percutaneous procedures is that they have low approach-related trauma, although certain techniques have yet to be proven effective. Although no universally accepted classification system has been suggested for percutaneous techniques for discogenic pain, the following definitions are helpful. Discogenic pain is produced by complex chemical and mechanical interactions. Internal disk derangement of the nucleus pulposus (dehydration and collagen disorganization) and associated annular disruption allow nuclear material and inflammatory cytokines, such as cyclooxygenase, interleukins, and prostaglandins, to come in contact with the perineural tissue surrounding the outer layers of the disk. Axial pain is believed to be produced by a combination of outer annular chemical sensitization, whereas radicular pain is produced by a direct mass effect and chemical inflammation of the nerve roots.2 Disk herniations can be further subdivided into contained (within disk boundaries) and uncontained (outside of the disk boundaries and into the spinal canal; i.e., extruded and sequestered). A spectrum of herniations is seen based on location, size, and consistency. Intradiskal procedures (both visualized and nonvisualized) are used to treat contained herniation and internal disk derangement and can be further subdivided into (a) intranuclear and (b) annular. Extradiskal procedures (visualized) are used to treat uncontained herniations. The workup for percutaneous procedures is similar to the workup of disk problems in general. A focused history and physical examination are performed, followed by radiologic studies. The most useful screening test is magnetic resonance imaging (MRI) to visualize the disk pathology directly. It is recommended that percutaneous procedures be preceded by diskography with postdiskography computed tomography (CT) scanning. The CT scan includes focal cuts through the affected levels.2–5 Postdiskography CT helps determine the size and location of the herniation and the presence of fissures, usually with greater accuracy than the MRI alone. This radiological study provides a route map for the guide-wire passage and defines the safe entrance zones to the disk to avoid vital structures, such as bowel or kidney, which could potentially be in the track of the guide-wire passage. Diskography may also help predict the outcome of the treatment (success rates based on positive diskograms are higher than in cases with negative results).3–6 In some cases, diskography shows dramatic pathology not seen on MRI (Fig. 61.1A–D). Although these procedures utilize different physical methods, the basic principle is to reduce the disk volume by removal of 10–15% of the nuclear material and thus reduce intradiskal pressure, allowing room for the herniated area to remodel gradually inward. Remodeling may or may not occur. If it does, it would be expected to occur over many months.2 In general, these procedures have the highest success rates in patients with contained, wide-neck herniations with intact posterior annulus and no migration or sequestration. Nonvisualized intranuclear procedures include chemonucleolysis, percutaneous automated nucleotomy, percutaneous laser disk decompression (PLDD), nucleoplasty, and the Dekompressor system (Stryker Interventional Spine, Allendale, NJ). Nonvisualized annular procedures include intradiskal electrothermal therapy (IDET), annuloplasty, and bipolar biacuplasty. Fig. 61.1 (A) L3–L4 axial MRI with a very equivocal left far lateral herniation. (B) Postdiskography CT scan of the same patient, clearly showing an extruded left far lateral fragment. (C) Axial MRI at L5–S1 showing a “high-intensity zone” accompanied by central disk bulge (internal disk structure is not clearly demonstrated). (D) Postdiskography CT scan of the same patient showing a wide, full-thickness annular tear. In 1963, Smith administered the enzyme chymopapain to the first chemonucleolysis patient. By 1984, 75,000 patients had been treated with this method. However, in 1999, this procedure was widely discontinued in the United States after several cases of transverse myelitis and anaphylactic deaths were reported.7,8 In 1975 Hijikata introduced the percutaneous manual nucleotomy, which was expanded by Onik, a radiologist, who developed an automated device (Nucleotome, Clarus Medical, Minneapolis, MN). This consists of a small probe that is positioned into the nuclear chamber via a standard posterolateral approach. The probe contains a distal window with an internal cutter and a suction mechanism. The nuclear material is cut and suctioned to an outside reservoir. The reported success rates of this procedure by itself vary from 29% to 75%.9,10 Success rates vary depending on the pathology, specifically, whether the herniation has a wide neck. It is a relatively simple and safe technique, and major complications are very rare.2,9–12 The Dekompressor probe has been recently introduced but received a very weak recommendation due to poor scientific support for its efficacy.2,13 Since its introduction by Ascher and Choy in 1986, the utilization of laser energy to reduce the nucleus pulposus volume has gained increasing popularity because of its small size, technical simplicity, and low incidence of complications. The effectiveness of PLDD varies from 56% to 87%, with an average relief of 72% at 1-year follow-up. The incidence of complications is around 1% and includes infectious diskitis, cauda equina syndrome, bowel perforation, and nerve root damage.2,14,15 In 2002 the U.S. Food and Drug Administration (FDA) approved the use of controlled ablation technology for percutaneous disk decompression. Disc Nucleoplasty (ArthroCare, Stockholm, Sweden) uses a 1-mm instrument that creates radiofrequency energy, which dissolves disk nucleus and removes such tissue at low temperatures, therefore preserving the integrity of the healthy tissue. Evidence for the success of this approach is anecdotal at the current time. The Centers for Medicare and Medicaid Services (CMS) have disallowed this procedure.1 Even though complications are rare, Cohen reported new onset of “neurologic” symptoms attributed to provocation of posterolateral disk nerve fibers.2,16,17 Intradiskal Electothermal Therapy (IDET) The Intradiskal Electrothermal (Smith & Nephew, Memphis, TN) treatment (IDET) was introduced by physiatrists Jeffrey and Joel Saal. The mechanism of action of this procedure is a subject of controversy and is not well described in the literature. Complications are rare. Thomas et al. reported a case in which the tip of the catheter broke off into the spinal canal and migrated into the dural sac, to be removed later by a wide laminectomy.18 Long-term data collection found that the results were less promising than previously expected. Pauza et al. (2003) reported that even though 40% of their patients achieved greater than 50% relief of their pain, ~ 50% of the patients experience no appreciable benefit.19 According to Assietti et al., the global clinical success rate was 78%, with a strong success correlation in highly concordant diskography findings, high-intensity zone (HIZ), and higher percentage of annulus covered by the catheter.2,20–22 The CMS disallowed this procedure.1 Newer thermal annular procedures include unipolar radiofrequency annuloplasty and bipolar biacuplasty, with only anecdotal studies reported in the literature.23–25 Disk removal is performed through a small working channel scope, passed through a cannula. Visualization is done on a monitor. Depending on the location of the disk fragments, minimal or no tissue removal may be required to remove the herniated fragment. For extradiskal, free fragments, the contents of the spinal canal can be well seen and fragments removed with a grasper. Access into the spinal canal can be obtained by either a transforaminal approach (Fig. 61.2A–D) or paramedian approach (Fig. 61.3A–D).26 The success rate (excellent and good) for this type of paramedian approach fragmentectomy at L5–S1 (Fig. 61.3A–D) has been reported as 93% in a series of 111 patients.27 In contrast to other procedures presented above, these procedures, removing free fragments in the spinal canal, are fundamentally different; they provide compelling visual, radiologic, and physical evidence of clear pathology, and that pathology is effectively dealt with and removed as a specimen. Scientifically controlled outcome studies have not been performed for most of the techniques discussed at the time of this writing. Potential risks of all procedures include infection, neurologic injury, retained pathology, continued pain, and injury to vital structures. Fig. 61.2 (A) Sagittal postdiskography CT scan. (B) Intraoperative fluoroscopic AP films showing the grasper in the epidural space at L5–S1. (C) Intraoperative fluoroscopic lateral films showing the grasper in the epidural space at L5–S1. (D) Free disk fragments that have been removed from the spinal canal.
Percutaneous Discogenic Pain Treatment
![]() Classification
Classification
![]() Workup
Workup
History and Physical Examination
Spinal Imaging
![]() Treatment
Treatment
Nonvisualized Nuclear Procedures
Chemonucleolysis
Percutaneous Automated Nucleotomy
Percutaneous Laser Disk Decompression (PLDD)
Nucleoplasty
Annular Procedures
Visualized Intradiskal and Extradiskal Procedures
Percutaneous Access Discectomy
![]() Outcome
Outcome
![]() Complications
Complications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






