A. Epidemiology—Spinal injuries are less common in children than in adults. Patients who are younger than 15 years old account for less than 10% of patients who sustain spinal cord injuries. The most common causes of spinal injury in children are motor-vehicle collisions, falls, and sporting injuries. A very young child with a spinal injury should be evaluated for nonaccidental trauma. Multilevel spinal injuries are common in children.
B. Differences between Children and Adults with Spine Trauma—Children are not just small adults. There are physiologic and anatomic differences that predispose them to different types of injuries and require different methods for management.
1. Head size—The pediatric patient’s head is disproportionately larger than that of the adult. This raises the fulcrum of motion into a more cephalic position (C2–C3 in children vs. C5–C6 in adults) which increases the incidence of upper cervical spine injuries in children. The upper cervical facets in children are also more horizontal, allowing for greater upper cervical motion. During evaluation on a back board, these properties force the cervical spine into greater flexion, which can make radiographic interpretation difficult and may manifest as pseudosubluxation. To accommodate for this a pediatric patient should be evaluated on a pediatric back board with an occipital cutout. Alternatively, a standard back board can be used with supports under the shoulders.
2. Spine anatomy—The pediatric spine may have open physes and developing ossification centers. This can make evaluation difficult for a physician unaccustomed to viewing pediatric spine radiographs. For instance, the odontoid synchondrosis may be mistaken for a fracture. Furthermore, fractures may occur through these cartilaginous regions, producing distinct pediatric spinal fracture patterns such as vertebral endplate injuries. These fractures may produce only subtle radiographic findings such as disc space widening.
3. The pediatric spinal column—The pediatric spinal column is more elastic than the spinal cord due to underdeveloped paraspinal musculature and ligaments. The spinal column can tolerate 2 inches of stretch, whereas the spinal cord can only tolerate approximately 0.25 inches of stretch. This puts the pediatric spine at risk for spinal cord injury without radiographic abnormality (SCIWORA).
4. Long-term management—Long-term management of pediatric spinal injury differs from that of adults. The pediatric patient is more likely to recover from neurologic injury due to the greater plasticity of the neural elements. In pediatric spine fractures, physeal injury may result in the development of spinal deformity. Alternatively, growth may allow for remodeling of mild deformities.
C. Imitators of Pediatric Spine Injuries
1. Pseudosubluxation (Fig. 32-1)—Pseudosubluxation is a normal physiologic variant in the pediatric cervical spine secondary to the relatively large head size and horizontal upper cervical facets.On radiographs, it manifests as anterior translation of the cephalic vertebral body relative to the caudad body and is most common at C2–C3. There may be up to 4 mm and 3 mm of pseudosubluxation at C2–C3 and C3–C4, respectively. It is most commonly seen in children younger than 8 years being evaluated with a supine lateral cervical radiograph taken on a standard back board without shoulder supports or an occipital cut out. The diagnosis is made (true subluxation is ruled out) using the posterior spinolaminar line (Swischuk’s line) on the lateral radiograph. This line connects the posterior arches of C1 and C3 and should come within 2 mm of C2.

FIGURE 32-1 Pseudosubluxation of C2 on C3. Hypermobility is common in children younger than 8 years. Specific measurement of the movement of the vertebral bodies is unreliable, whereas the relationship with the posterior elements is more consistent. In flexion, the posterior arch of C2 lies in a relatively straight line with C1 and C3. Note the relative horizontal nature of the facet joints, which allows greater mobility. (Reprinted with permission from Capen DA, Haye W. Comprehensive Management of Spine Trauma. St Louis, MO: Mosby; 1998.)
2. Ossification of the odontoid process—Different stages of ossification of the odontoid process can mimic injuries to this structure. The apical ossification center can mimic an avulsion fracture. The synchondrosis fuses by age 6, but is still visible until age 12 and this may make diagnosis difficult. Persistence of the synchondrosis at the base of the odontoid can mimic fracture. Incomplete ossification of the odontoid process can mimic atlantoaxial instability.
3. Imitators of compression fractures after minor trauma—Eosinophilic granuloma, Mucopolysaccharidoses, Gaucher’s disease, Osteogenesis imperfecta, Tuberculosis, tumor.
D. Workup for Pediatric Spine Injury
1. Clinical examination—Since spinal fractures are often the result of a significant trauma, workup should begin with assessment of the patient: Airway, Breathing, and Circulation. The patient should be transported and assessed on a pediatric back board with an occipital cut out or a standard back board with shoulder supports to accommodate for the relatively large head size. The Primary Survey should include a visual survey and palpation of the head, neck, back, and pelvis. The abdomen should be evaluated for a lap belt sign, which should increase suspicion for an injury of the spine and viscera. A complete neurologic exam should be performed.
2. Radiographic examination—Patients involved in high-energy trauma should have lateral C-spine, AP pelvis, and AP chest radiographs. Dedicated AP and lateral radiographs should be obtained of any location with tenderness, swelling, or ecchymosis. Any patient with an identified spine fracture should have AP and lateral radiographs of the entire spine as noncontiguous multilevel injuries are common. Twenty-four percent of pediatric cervical spine injuries have a second spine injury. CT scan and MRI may be used for increased bony and soft-tissue detail. MRI may be used to clear a C-spine in a noncooperative patient.
E. Radiographic Evaluation Specific to the Pediatric Spine
1. Cervical spine—Powers ratio is used to evaluate the atlanto-occipital junction and should be between 0.7 and 1.0. Normal atlantodental interval may be up to 4.5 mm. At the level of C1, one-third should be taken up by the odontoid, one-third by the spinal cord, and one-third by space available for the cord. Pseudosubluxation up to 4 mm at C2–C3 is physiologic. Subtle disc height changes may be signs of fracture through vertebral endplates.
F. Developmental Anatomy (Figs. 32-2 and 32-3)—Knowledge of the unique ossification patterns of the pediatric spine is necessary for proper evaluation of an injury.
1. Atlas (C1)
• Ossification centers—The atlas has three primary ossification centers. The right and left neural arches are ossified at birth, and the body ossifies at 1 year.
• Fusion—The atlas body and neural arch synchondroses fuses at 7 years. The spinous process (neural arch) synchondrosis fuses at 3 years.
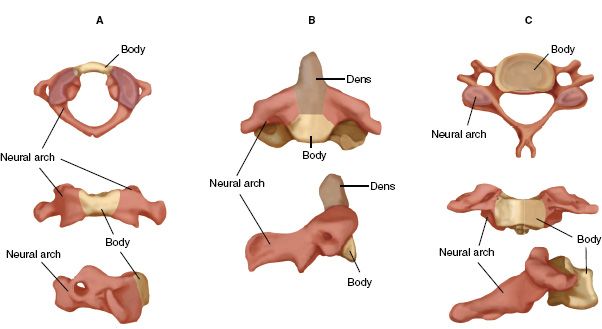
FIGURE 32-2 Ossification centers. A, C1. B, C2. C, Typical of C3-L5.
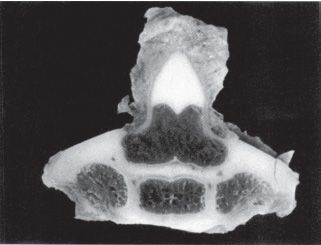
FIGURE 32-3 Morphologic development of the second cervical vertebra at 3 months. The odontoid ossification centers have coalesced. The neurocentral synchondroses separate the centrum from the posterolateral elements. (Reprinted with permission from Ogden JA. In: Ogden JA, ed. Skeletal Injury in the Child. 2nd ed. Philadelphia, PA: WB Saunders; 1990.)
• Ossification centers—The axis has four primary ossification centers at birth. The two odontoid ossification centers fuse in the midline by the seventh fetal month. The body and the two neural arches are ossified at birth. The secondary ossification center at the tip of the odontoid appears at 3 years. The inferior epiphyseal ring ossifies at puberty.
• Fusion—The synchondrosis between the body and the odontoid fuses by 6 years. The fusion line is often visible until age 12. The neural arches fuse to the body by 6 years, and the spinous processes fuse by 3 years. The secondary ossification center at the tip of the odontoid fuses by 25 years, as does the inferior epiphyseal ring ossification center.
3. C3–C7
• Ossification centers—Five ossification centers are all present at birth. These are the body, two neural arches, and two transverse processes.
• Fusion—The transverse processes fuse to the body by age 6. The body and neural arches fuse by age 6. The spinous processes fuse by age 3. Bifid spinous processes appear at puberty and fuse by age 25. The superior and inferior epiphyseal rings fuse by age 25.
4. Thoracic and lumbar spine—Adult characteristics and size are present by age 10 with a similar radiographic examination except for the open epiphyses.
• Overview—The thoracic and lumbar spine ossify and fuse in a similar manner.
• Lumbar Ossification Centers—Additional ossification centers are present in the lumbar spine for the mammary processes. They appear during puberty and fuse by age 25.
G. Immobilization Techniques—During initial evaluation, the patient should be immobilized on either a pediatric back board or a standard back board with shoulder supports. Traction should not be used.
1. Rigid immobilization collars—A rigid collar with access to the oropharynx and neck should be used. Rigid collars allow up to 17° of flexion, 19° of extension, 4° of rotation, and 6° of lateral motion. Motion can be decreased to 3° in each direction by supplementing with sandbags and tape.
2. Halo-vest immobilization—Halo-vest immobilization may be used in patients as young as 1 year of age. The thickness of the pediatric skull is variable and therefore pin penetration is a potential complication. CT scan of the skull should be considered to estimate skull thickness at potential pin sites. eight to twelve pins should be placed with torques of only 2 to 4 in-lb. Halo-vest restricts 75% of C1–C2 motion.
H. SCIWORA—SCIWORA is more common in children than in adults because of the increased elasticity of the vertebral column, shallow facet joints, poorly defined uncinate process, and more proximal fulcrum of cervical motion. The term was coined before MRI was available, and despite having no radiographic abnormality, most will have an MRI abnormality. Approximately 20% to 30% of children with spinal cord injury have SCIWORA. There are two peak incidences:
1. Age 8 to 10 years—Most commonly a proximal injury at the cervicothoracic junction. Neurologic injuries in this group are usually permanent.
2. Adolescents—Most commonly a mid-thoracic injury that may be associated with a visceral injury. Neurologic injuries in this group have a better prognosis for neurologic recovery.
SCIWORA often has delayed onset of neurologic deficit, which may take up to 4 days to manifest. Spine precautions should be maintained until instability is ruled out. Recurrence of neurologic deficit has been reported but it is unclear whether bracing prevents recurrence. Outcome is correlated with MRI findings and severity of neurologic deficit on presentation.
I. Cervical Spine Injuries—Cervical spine fractures account for approximately 1% of pediatric fractures. The incidence is estimated to be 7.41 in 100,000 per year. There is a 16% mortality rate associated with cervical spine fractures. Sixty percent of these injuries occur in boys and 27% occur during sporting activities. Other mechanisms of injury include motor-vehicle collisions, falls, and nonaccidental trauma. Children under age 8 most commonly have upper cervical injuries while older children have lower cervical injuries. Clinical findings such as facial lacerations and contusion, and palpable posterior cervical defects may be clues to cervical spinal injury.
1. Atlanto-occipital dislocation (Fig. 32-4)
• Incidence—Atlantooccipital dislocation accounted for one-third of deaths from traumatic cervical spine injuries in one series. It is frequently associated with severe spinal cord and brainstem injury causing respiratory arrest. The atlantooccipital joint is a condylar joint that in the pediatric population is almost horizontal and provides little bony stability. Injury mechanism is usually a sudden deceleration causing hyperextension of the occipitocervical junction.
• Evaluation—The Powers ratio can be measured on the lateral cervical spine radiograph. Ratio greater than 1.0 indicates anterior dislocation and a ratio less than 0.7 indicates posterior dislocation.
• Treatment—Associated injuries often include severe head, thoracic, and visceral injuries. Initial cervical stabilization should be obtained with a halo vest. Traction is contraindicated. Definitive treatment requires occiput—C2 fusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






