I. Introduction—Pediatric lower-extremity injuries occur much less frequently than upper extremity injuries. Long-bone fractures occur after high-energy trauma such as motor-vehicle accidents and sports injuries or after simple falls in younger children. Unfortunately, child abuse may be the etiology, particularly in younger children. The clinician must always consider this possibility. Sequelae of fractures, such as growth arrest, leg length discrepancy, malunion, neurovascular injury, and compartment syndrome, can profoundly affect the child’s function. Attention to detail when managing lower-extremity injuries can lessen the frequency of these undesirable outcomes.
Because lower-extremity fractures can result from high-energy trauma, the patient must have a systematic evaluation. The primary survey is performed to exclude life-threatening injuries and is followed by the secondary survey. Management of specific musculoskeletal injuries depends largely on the age of the patient and the associated injuries.
Open fractures are irrigated and meticulously debrided in the operating room before skeletal stabilization. Prophylactic antibiotics are administered in weight-appropriate doses. Tetanus prophylaxis should be given if necessary. Depending on the mechanical stability and extent of soft-tissue damage, some fractures can be managed in a cast that is windowed for wound care. External fixation, internal fixation, or traction is used for more extensive injuries. As with adult patients, surgical (skeletal) stabilization is generally preferred in cases of pediatric multiple trauma and in cases of head injury.
II. Fractures of the Hip
A. Overview—Hip fractures, defined as injuries to the portion of the femur proximal to the lesser trochanter, are rare. Such fractures represent less than 1% of all pediatric fractures. Approximately 85% of pediatric hip fractures result from high-energy trauma. The remaining 15% consist of pathologic fractures, usually through tumors. The capital femoral epiphysis appears between 4 and 6 months of age, and the physis fuses between 14 and 16 years of age. The proximal femur contributes 13% of the length of the leg, or 3 to 4 mm per year. The blood supply is tenuous and therefore susceptible to injury.
B. Evaluation—The child usually has hip pain and refuses to walk. If the fracture is displaced, the leg may appear shortened and externally rotated. Plain films are the best initial study. If plain films are negative, a bone scan or magnetic resonance imaging (MRI) can detect occult fractures.
C. Classification—The Delbet classification is most commonly used (Fig. 30-1).
1. Type I—Type I fractures (transepiphyseal fractures [transphyseal separations]) occur more often in younger children. Some 50% are associated with hip dislocations. There is a high incidence of avascular necrosis (AVN), especially with dislocations.
2. Type II—Type II fractures (transcervical) are the most common, representing 46% of pediatric hip fractures. The risk of AVN is related to the amount of initial displacement.
3. Type III—Type III fractures (cervicotrochanteric) represent 34% of hip fractures. A good outcome is likely if the fracture is not displaced. AVN is related to both fracture severity and amount of initial displacement.
4. Type IV—Type IV fractures (intertrochanteric) have the best prognosis. Complications are less common.
D. Treatment—Hip fractures, particularly displaced ones, require expeditious treatment. In general, in addition to internal fixation, all fractures require cast immobilization for at least 6 weeks if the child is younger than 10 years of age.
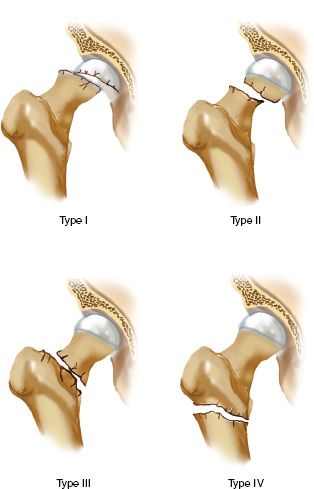
FIGURE 30-1 Delbet classification of pediatric hip fractures. Type I, transepiphyseal fracture; Type II, transcervical fracture; Type III, cervicotrochanteric fracture; Type IV, intertrochanteric fracture.
1. Type I fractures—Type I fractures should undergo a gentle closed reduction and internal fixation. Fixation is achieved with smooth pins or with cannulated screws in older children. If the child is younger than 2 years of age, reduction and spica cast immobilization without internal fixation is a reasonable treatment for stable fractures. With dislocations, a single attempt at closed reduction is warranted. If unsuccessful, open reduction should be performed from the direction of the dislocation.
2. Type II fractures—Type II fractures require anatomic reduction and stable fixation. A gentle closed reduction may be attempted. If unsuccessful, an open reduction through an anterolateral approach should be performed. Stable fixation is essential. Although the physis should be avoided, stable fixation takes precedence over protecting the physis. Casts should be applied for 6 to 12 weeks for children who require immobilization.
3. Type III fractures—Type III fractures also require an anatomic reduction and stable fixation. Achieving anatomic reduction requires that an anterolateral open reduction be performed if necessary. The benefit of decompressing the intracapsular hematoma is controversial, but the procedure is advocated by some as a possible means of decreasing the risk of AVN.
4. Type IV fractures—Type IV fractures can usually be treated by closed techniques. Reduction can be achieved under anesthesia or with traction and followed by the application of an abduction spica cast. If the fracture is irreducible or unstable in a cast, internal fixation should be used with a pediatric screw and side plate system. In patients with multiple injuries, Type IV fractures should be treated with open reduction and internal fixation.
E. Complications
1. AVN—AVN is the most common complication, occurring in 6% to 47% of cases. AVN usually occurs during the first 12 to 24 months after injury and is related to initial fracture displacement with the consequent compromise of blood supply. AVN has also been shown to be associated with increasing age, time to reduction, and quality of reduction. The treatment of AVN of the pediatric hip is controversial but includes restricted weightbearing, bed rest, soft-tissue releases, and containment. There are three types of AVN (Fig. 30-2).
• Type I involves the whole head. It has the worst prognosis.
• Type II involves part of the head. The prognosis is fair.
• Type III occurs from the fracture line to the physis. The prognosis is good.
2. Coxa vara—The incidence of coxa vara after pediatric hip fractures ranges from 14% to 30% but is consistently lower and even absent in series using internal fixation. Coxa vara results from malunion, AVN, inadequate fixation, or partial physeal closure. Observation for 2 years is acceptable because the deformity often remodels with time. If the neck-shaft angle is less than 110° or the child is over 8 years of age, a subtrochanteric valgus osteotomy may be performed.
3. Growth arrest—Growth arrest occurs when AVN is present or when fixation necessitates crossing the physis. Type II and III AVN most often lead to arrest. Leg length measurements and bone age should be followed. Epiphysiodesis or lengthening may be performed if a large leg length discrepancy is anticipated.
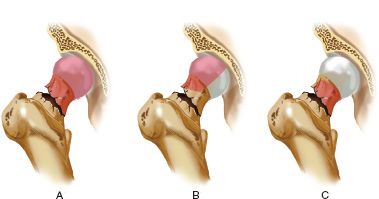
FIGURE 30-2 Patterns of AVN of the pediatric hip. A. Total involvement of the capital femoral epiphysis, physis, and metaphysis (Type I). B. Anterolateral involvement (Type II). C. Metaphyseal involvement (Type III).
4. Nonunion—Nonunion, an infrequent complication, has an incidence of 6% to 10%. An incomplete reduction is often the cause. As soon as it is recognized, nonunion should be treated operatively with subtrochanteric valgus osteotomy with or without bone graft.
F. Special Considerations
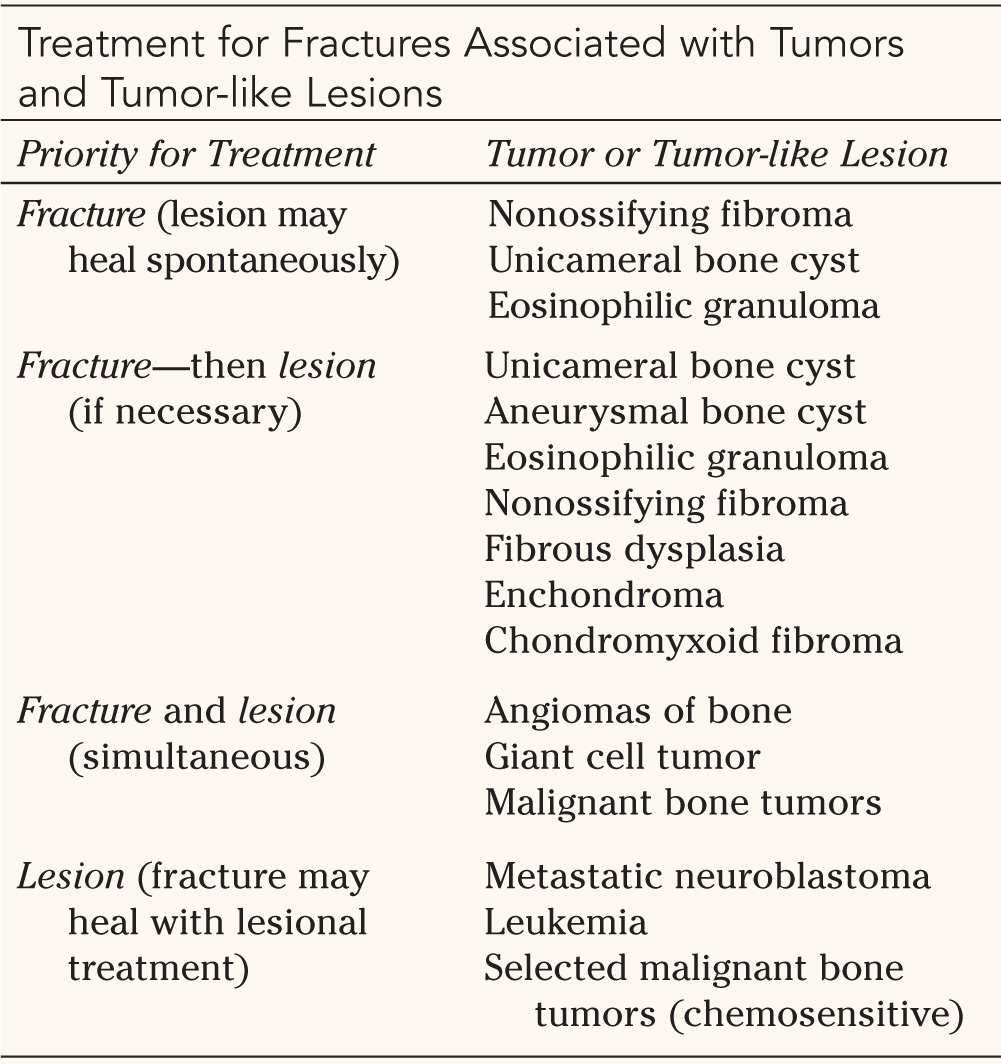
1. Pathologic fractures (Fig. 30-3)—Fractures that occur through benign or malignant tumors pose difficult problems. The objective is management of the fracture concurrent with the underlying problem if possible. In some cases, the fracture must heal before tumor management. A guide for management is outlined in Table 30-1.
2. Stress fractures—Stress fractures are rare but can occur in children engaged in activities with cyclic loading. The differential diagnosis includes a slipped capital femoral epiphysis, synovitis, Perthes’ disease, avulsion fracture, and neoplasm. Plain films may be negative for several weeks; bone scan and MRI are therefore helpful for early diagnosis. Stress fractures occur in two types: tension fractures occur on the superior femoral neck, whereas compression fractures occur on the inferior femoral neck. Tension fractures are at risk for displacement; therefore, internal fixation is recommended. Compression fractures are more stable and can be managed with either restricted weightbearing or a spica cast in a less compliant patient.
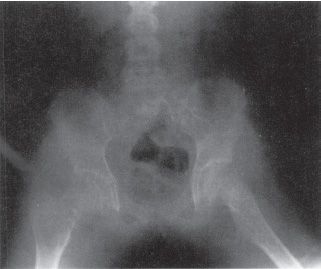
FIGURE 30-3 Anteroposterior radiograph of the pelvis of a 10-year-old girl shows a radiolucent lesion (aneurysmal bone cyst) of the right proximal femur with a pathologic femoral neck fracture.

Source: From Green NE, Swiontkowski MF, eds. Skeletal Trauma in Children. 2nd ed. Philadelphia, PA: WB Saunders; 1998, with permission.

3. Slipped capital femoral epiphysis—An unstable acute slipped capital femoral epiphysis presents similarly to a transepiphyseal fracture. Questioning may reveal a history of chronic hip pain, knee pain, or a limp. Radiographs of the hip may demonstrate remodeling of the femoral neck in slips with a chronic component. Stable slips can be stabilized with a cannulated screw inserted percutaneously. Displaced unstable slips should have a gentle reduction by traction or under anesthesia. The femoral head is then stabilized internally in the chronic slip position. Another option is surgical hip dislocation with anatomic restoration of alignment and internal fixation performed by experienced hands.
III. Fractures of the Femoral Shaft
A. Overview—Femoral shaft fractures, which occur in the region between the lesser trochanter and the supracondylar metaphysis, almost always unite. The challenge is achieving union with acceptable length, alignment, and rotation. Femoral fractures represent 1.6% of all pediatric fractures and 7.6% of all pediatric long-bone fractures. The incidence of child abuse, in children with a femur fracture, approaches 80% in infants younger than walking age, and 30% in children younger than 4 years of age. Young children may sustain femoral fractures with simple falls, whereas older children may be involved in high-energy trauma such as that from motor-vehicle accidents.
B. Evaluation—Most patients have severe pain and are unable to walk. There may be obvious deformity, swelling, tenderness, and crepitation. Isolated fractures do not cause hypotension. Children with signs of hypovolemia should be carefully evaluated for additional injuries. Plain films are the preferred initial studies and should include the knee and hip to rule out other fractures.
C. Classification—There is no formal classification system. Descriptors such as transverse, spiral, oblique, segmental, comminuted, closed, and open are used.
D. Treatment—The management of pediatric femoral shaft fractures depends on many factors, including age, the mechanism of injury, associated injuries, economic considerations, and psychosocial issues. The goal is to achieve bony union without excessive shortening or malalignment. Current trends attempt to avoid lengthy hospitalization. Fractures with neurovascular injuries, open fractures, multiple trauma, and head injury require operative stabilization. In general, isolated injuries in young children may be managed with an immediate spica cast; the injuries of children close to maturity are managed with locked intramedullary nails. For children between 6 and 12 years, there is considerable controversy. All the techniques described have advocates and support in the literature.
1. Immediate spica casting—Children younger than 6 years or weighing less than 60 pounds with isolated closed injuries can be treated with an immediate spica cast. Single leg, one and one half, and double leg spica casts have been reported. If there is more than 2 cm of shortening, some recommend a brief period of skin or skeletal traction before casting. Strict attention to detail is essential for immediate spica casting. Length must be restored, and the cast must be carefully molded to prevent late varus or recurvatum angulation. Radiographic studies are done weekly for the first 2 to 3 weeks to rule out loss of reduction and excessive shortening, which occur in approximately 20% of cases. Loss of reduction may be corrected with cast wedging or cast reapplication. Children who develop unacceptable shortening should be placed in skeletal traction until length is restored and then recasted. The cast is worn for 6 weeks.
2. Traction-delayed spica—Traction with delayed spica cast application yields uniformly good results. The child is placed in skin or skeletal traction for 2 to 3 weeks until the fracture becomes more stable. Radiographs must be checked every few days for excessive shortening or over-distraction. A spica cast is then applied. The technique can present social (and economic) difficulties because of the lengthy hospitalization.
3. Locked intramedullary nail—The injuries of adolescents close to maturity are managed like those of adults: with a rigid locked intramedullary nail. If the capital femoral physis is open, care should be taken to avoid the piriformis fossa when inserting the nail. Damage to the lateral ascending arteries in the piriformis fossa can cause AVN of the femoral head; a more anterior or trochanteric starting point is therefore advised. Recently designed pediatric nails avoid the piriformis fossa and the greater trochanteric apophysis. The nail should not violate the distal femoral physis.
4. External fixation—Unilateral external fixation allows early mobilization. The fixator is applied to the lateral side of the leg; full knee motion must be achieved while in the operating room. The family must be vigilant about pin care because there is a high rate of pin tract infection. Refracture is another complication. A total of 12 weeks may be required before adequate bridging callus is present. Dynamization is important and must be done early.
5. Flexible intramedullary nails—Flexible intramedullary nails (Enders, Nancy) allow early mobilization and therefore avoid the problems of prolonged traction and casting. The nails may be inserted in a retrograde fashion; the starting point is proximal to the distal femoral physis. The nails may also be inserted in an antegrade fashion; the starting point is distal to the greater trochanter. A second operation is necessary to remove the nails after fracture healing. With titanium nails, poor outcomes have been associated with age greater than 11 years, weight greater than 49 kg, and comminution or long oblique fracture patterns. Stainless steel nails had fewer complications than titanium nails in one series.
6. Compression plates—Compression plating is technically simple, convenient for the family, and conducive to early mobilization. It requires large incisions, extensive dissection, and protected weightbearing after insertion. Plate removal is mandatory, and protected weightbearing is continued for 6 weeks.
7. Submuscular bridge plates—Submuscular plating provides all the advantages of compression plating, with less dissection, scarring, blood loss, and more rapid healing. The technique is particularly advantageous for comminuted fractures that are not amenable to treatment with other types of fixation. Achieving an acceptable reduction is critical before applying the plate percutaneously. The plate can then be secured with regular or locking screws, the latter providing greater stability.
E. Complications
1. Leg length discrepancy—Leg length discrepancy is the most common complication. It can be secondary to fracture union in a shortened position or limb overgrowth. Overgrowth is poorly understood, but it occurs in children between 2 and 10 years of age during the first 2 years after injury. The amount of overgrowth ranges from 0.5 to 2.5 cm. Leg lengths should be followed for at least 2 years after the union of a pediatric femoral shaft fracture. Projected shortening discrepancies greater than 6 cm or those with significant deformity can be treated with lengthening and/or deformity correction. Smaller projected discrepancies without deformity are treated with epiphyseodesis (of the ipsilateral extremity in the case of overgrowth and of the contralateral extremity in the case of shortening).
2. Angular deformity—Angular deformity frequently occurs, and there are several recommendations for acceptable amounts of deformity. Femoral shaft fractures remodel considerably in younger children. Lateral view angulation of 30° is acceptable in children younger than 2 years, but the limit decreases to 10° in children 11 years and older. In the coronal plane, valgus angulation is better tolerated in general than varus angulation. Anteroposterior (AP) view angulation of 20° to 30° is acceptable in infants, 15° in children younger than 5 years, 10° up to 10 years of age, and 5° in children 11 years and older.
3. Rotational malunion—Rotational malunion occurs in up to one third of children. There is less remodeling potential than with angular deformities, but up to 30° of malrotation is usually well tolerated in children. Derotation osteotomy corrects malunions that require intervention.
4. Neurovascular injuries—Neurovascular injuries are rare, occurring in less than 2% of femoral shaft fractures. Fractures with vascular injuries should be stabilized rapidly, followed by vessel repair. Most nerve injuries associated with the fracture spontaneously recover.
5. Compartment syndrome—compartment syndrome can occur after application of a 90/90 spica cast. Application of the short leg portion of the cast first with subsequent application of traction is believed to be the etiology.
F. Special Considerations
1. Floating-knee injuries—defined by fractures of the femur and the ipsilateral tibia, are usually high-energy injuries. Most authors agree that at least one of the fractures should be managed operatively.
2. Stress fractures—stress fractures of the femoral diaphysis are rare in children. The history of an increase in activity may not be present. Radiographs may be normal, or show periosteal new bone suggestive of a neoplasm. MRI is helpful in making the diagnosis.
IV. Fractures of the Distal Femoral Metaphysis and Epiphysis
A. Overview—The distal femoral physis is the largest and fastest growing in the body. It is responsible for 70% of the femoral length and 37% of the leg length. It grows approximately 1 cm a year, fusing between 14 and 16 years of age in girls and 16 and 18 years in boys. Because the physis undulates, an accurate reduction is important for preventing physeal bar formation in displaced fractures. Fractures involving the distal femoral physis are relatively uncommon, representing only 7% of all physeal fractures. Injuries usually result from sports or motor vehicle accidents. The fracture typically occurs during periods of rapid growth such as the adolescent growth spurt. In children before walking age, there is a strong association between complete fractures and child abuse.
B. Evaluation—The child has an acute onset of pain and is usually unable to walk. The thigh may be angulated or shortened. The knee is tender, with an effusion and ecchymosis. Careful attention to the neurovascular examination is essential for ruling out an associated injury. AP and lateral plain films are the best initial studies. Oblique films may detect a fracture if the initial films are negative. Gentle-stress views or an MRI can be used for difficult cases.
C. Classification—The Salter-Harris classification, although not prognostic, is most commonly used. Salter-Harris Types I and II fractures have a more frequent incidence of growth disturbance. The most important prognostic factors are the magnitude of displacement, age, adequacy of reduction, and severity of trauma.
D. Treatment—Nondisplaced fractures should be stabilized percutaneously with smooth pins because of the high risk of displacement. Displaced Salter-Harris Types I and II fractures require reduction and percutaneous fixation. The reduction maneuver is primarily traction with gentle manipulation. Percutaneous fixation is performed with either smooth wires or screws, followed by a cast for 6 weeks with the knee in 10° of flexion. Anatomic reduction is desirable. In children near maturity, up to 5° of varus or valgus angulation is acceptable. In children younger than 10 years, 20° of posterior angulation is acceptable. Displaced Salter-Harris Types III and IV fractures necessitate anatomic reduction with internal fixation by closed or open methods. Fixation is accomplished with screws followed by a cast for 6 weeks. Pathologic fractures through benign lesions should receive standard fracture care, with management of the neoplasm secondarily after healing.
E. Complications
1. Leg length discrepancy—Leg length discrepancy is the most common complication (32%). The age at injury is important; discrepancies usually occur with high-energy injuries in younger children. The risk is greater if fracture displacement is greater than 50% of the width of the bone. Treatment options are those that are standard for leg length discrepancy.
2. Angular deformity—Angular deformity (incidence, 24%) occurs most frequently after Salter-Harris Type II fractures. It is usually due to direct physeal injury on the side of the physis opposite the metaphyseal spike. Management may include epiphysiodesis or osteotomy depending on the child’s age. The former is performed when a child is close to the end of growth.
3. Physeal bars—Physeal bars can be assessed with tomograms or computed tomograms (CT) to determine the size. Bars measuring less than 50% of the physeal area can be resected, with fat interposition. Resection is contraindicated if the patient has fewer than 2 years of growth remaining. Extensive bars in children near skeletal maturity can be treated with epiphysiodesis of the uninjured leg.
4. Neurovascular injuries—Neurovascular injuries (incidence, 2%) are rare and usually result from hyperextension injuries. The popliteal artery is injured with anterior displacement, and the peroneal nerve is injured with varus angulation. Fractures with suspected neurovascular injuries should be reduced emergently with prompt reassessment of vascular status. If the vascular supply is restored, the patient should be observed for 48 to 72 hours to rule out an intimal tear with thrombosis. If the fracture is irreducible, an open reduction is performed through a posteromedial approach, and the neurovascular structures are directly assessed.
5. Extension contracture of the knee—Extension contracture of the knee rarely follows severe supracondylar femur fractures. Cases failing rehabilitation are managed with Judet quadricepsplasty.
V. Fractures of the Intercondylar Eminence
A. Overview—The intercondylar eminence lies between the anterior horns of the menisci. Fractures of the intercondylar eminence are most common in children between 8 and 14 years of age. Injuries occur after hyperextension of the knee, a fall from a bicycle or motorbike, or a direct blow to the knee.
B. Evaluation—The child typically has pain, an effusion in the knee, and an inability to bear weight. An aggressive examination should be avoided before radiographic studies to prevent displacement of the fragment. AP and lateral plain films are the best diagnostic studies; the most useful information is obtained from the lateral view. Stress views can be added if an associated physeal or ligamentous injury is suspected.
C. Classification—The Myers and McKeever classification is standard (Fig. 30-4).
1. Type I—Type I is nondisplaced.
2. Type II—Type II is one-third to one-half displaced and is hinged.
3. Type III—Type III is completely displaced.
D. Treatment—For Types I and II fractures, first the hemarthrosis is aspirated. The knee is hyperextended to reduce the fragment, and a long leg cast in 10° to 15° of flexion is worn for 4 to 6 weeks. Irreducible Type II and III fractures may have a meniscus blocking reduction. Reduction is performed open or with arthroscopic assistance. Fragment fixation should be done with absorbable sutures in young children. In older children, non-absorbable sutures or an intraepiphyseal screw is used.
E. Complications—Loss of knee extension occurs in up to 60% of cases but is rarely a functional problem. Anterior laxity of the knee occurs in 75% of cases, probably as a result of plastic deformation of the anterior cruciate ligament (ACL) before fracture. Patients generally have good outcomes despite residual laxity.
VI. Meniscal Injuries
A. Overview—The menisci are semilunar cartilaginous cushions in the medial and lateral compartment of the knee. They are completely vascularized at birth. With maturation, the vascular supply to the inner two thirds diminishes. The discoid meniscus is an uncommon congenital anomaly occurring in 3% to 5% of the population. Meniscal tears are rare in prepubescent children unless a discoid meniscus is present. Injuries occur primarily in adolescents.
B. Evaluation—The child typically complains of activity-related pain, possibly mechanical symptoms. Acutely the child may have an effusion of the knee, but it usually develops over a few hours after injury. There may be joint-line tenderness, or the results of McMurray’s test may be positive. Plain films should be done to rule out osteochondritis dissecans or a loose body. MRI is the test of choice.
C. Classification—Injuries are classified by the anatomy of the tear: radial, flap, longitudinal, horizontal cleavage, and bucket handle.
D. Associated Injuries—Associated injuries include cruciate ligament tears.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







