CHAPTER 26 Pediatric Kyphosis
Scheuermann Disease and Congenital Deformity
The normal adult spine has four curves in the sagittal plane. In utero and at birth, there are two primary kyphotic curves in the thoracic spine and sacrococcygeal region. The lordotic curves in the cervical and lumbar spine are compensatory curves and develop as a child holds his or her head upright and begins to stand and walk.1 Lordotic curves are considered secondary and compensate for the degree of kyphosis in the primary curves to allow a balanced spine in the sagittal plane.
There is great variability in defining the normal range of thoracic kyphosis. As measured by the Cobb method, the normal range of thoracic kyphosis is 20 to 45 degrees.2,3 Normal kyphosis increases with age and is slightly greater in women.3 Thoracic kyphosis is measured on a lateral radiograph using the Cobb method from the superior endplate of T2 to T5 depending on visibility to the inferior endplate of T12. The thoracolumbar junction is normally neutral or slightly lordotic (0 to 10 degrees of lordosis). Any degree of kyphosis at the thoracolumbar junction is considered abnormal. Lumbar lordosis is measured from the superior endplate of L1 to the superior endplate of S1, and normal values are 40 to 65 degrees.
The importance of achieving a neutral sagittal balance has been emphasized in recent years in the evaluation and treatment of various kyphotic deformities. The C7 plumb line should fall through the posterosuperior corner of the L5-S1 disc space. If it falls anterior to this point, there is positive sagittal balance, and if it falls posterior to this point, there is negative sagittal balance. Jackson and McManus4 reported values in asymptomatic adults with a mean sagittal vertical axis offset of 0.5 cm (± 2.5 cm SD). According to these data, offset greater than 2.5 cm anteriorly or posteriorly is considered beyond the normal range. A positive sagittal balance is poorly tolerated because intradiscal pressures increase in the lumbar spine, and the posterior spinal musculature is placed at a mechanical disadvantage leading to back pain.
Scheuermann Disease
In 1921, the Danish radiologist Scheuermann described a pathologic condition and distinguished it from passively correctable postural humpback when he noted the development of painful fixed kyphosis in 105 children.5 Scheuermann likened the entity to the femoral head abnormality described by Calvé and Perthes and named it osteochondritis deformans juvenilis dorsi. Several terms have been used in the past to describe this entity, including kyphosis dorsalis juvenilis, but Scheuermann disease and Scheuermann kyphosis are the most common.6
Scheuermann disease is the most common cause of severe thoracic kyphosis in adolescents with reported prevalence of 1% to 8%.7–9 The prevalence is approximately equal in boys and girls. Approximately one third of patients have concomitant scoliosis, which is usually mild.10
In 1964, Sorensen11 defined the radiographic criteria that have now become widely accepted for diagnosing Scheuermann disease: anterior vertebral wedging greater than 5 degrees on three or more consecutive vertebrae at the apex of the curve. Associated radiographic findings include endplate irregularities and Schmorl nodes (herniation of disc into vertebral endplates). Schmorl nodes are not specific to Scheuermann disease and can be found in various conditions. Scheuermann disease is typically diagnosed at age 10 to 12 years. Sorenson’s criteria are typically not present in patients younger than age 10 because the ring apophysis has not ossified before this age.
There are two curve patterns in Scheuermann disease. The thoracic type is most common, and its apex is located between T7 and T9. The thoracolumbar type has also been referred to as “atypical” Scheuermann disease; its apex is located between T10 and T12, and it is more likely to become symptomatic in adult life.10 Vertebral endplate changes, Schmorl nodes, and disc space narrowing are much more common in the thoracolumbar form of Scheuermann disease. Sorenson’s criteria (three consecutive wedged vertebrae) are unnecessary to diagnose the thoracolumbar form of Scheuermann disease.
Lumbar Scheuermann disease is a distinct entity in which significant degenerative changes are present in the lumbar spine (typically L1-4) without vertebral wedging or significant kyphotic deformity (Fig. 26–1). Schmorl nodes and endplate irregularities are common. Lumbar Scheuermann disease is more common in males, especially laborers who engage in heavy lifting activites.
Etiology
Although the etiology of Scheuermann disease is unknown, several theories exist. Scheuermann’s initial description suggested that the condition results from avascular necrosis of the vertebral ring apophyses, which leads to a premature growth arrest with resultant wedging of the anterior portion of the vertebral bodies, and mentioned that it resembled Legg-Calvé-Perthes disease of the hip.5,6 Schmorl and Junghans12 hypothesized that herniation of disc material into the vertebral body endplates occurred as a result of inherent weakening of the cartilaginous endplate, with resultant damage to the endplate causing growth disturbance and kyphosis. Schmorl nodes are not specific to kyphotic deformities, however, and are found in normal spines.
Genetic factors have also been proposed. An autosomal dominant inheritance pattern with incomplete penetrance and variable expression in families with Scheuermann disease has been described.13–15 Three cases of Scheuermann kyphosis in monozygotic twins have been reported in the English literature,11,16,17 supporting the genetic etiology hypothesis.
Other etiologies of the deformity have been attributed to defective endplates, upright posture, juvenile osteoporosis, increased release of growth hormone, defective formation of collagen fibrils with subsequent weakening of vertebral endplates, strenuous manual labor, trauma, vitamin A deficiency, epiphysitis, poliomyelitis, prolonged sitting, and osteochondrosis.18–23 Mechanical factors have also been proposed to play a role in pathogenesis, owing to partial reversal of vertebral wedging with brace treatment and thickening of the anterior longitudinal ligament.10,24
Clinical Evaluation
The clinical evaluation begins with a complete history and physical examination. The deformity is often attributed to poor posture in an adolescent, delaying diagnosis and treatment.10 One should inquire about the onset of the deformity and the location of pain. If the patient has pain, it is usually mild and aggravated by prolonged sitting or exercise and typically is near the apex of the kyphotic deformity.10 Spondylolysis and spondylolisthesis have been noted with an increased incidence in patients with Scheuermann disease and can be a source of low back pain.25 There is a 50% incidence of spondylolysis in Scheuermann kyphosis,25 presumably resulting from increased stress on the pars interarticularis in the lower lumbar spine as a result of hyperlordosis. With significant deformity, the erector spinal musculature is placed at a mechanical disadvantage, which may also contribute to pain that is common with this condition.
Increased lumbar lordosis is often noted in these patients as compensation for the kyphotic deformity to maintain overall sagittal balance. It is important to assess coronal and sagittal balance. Lowe and Kasten26 studied the sagittal contour of 24 patients with Scheuermann kyphosis and found that most patients with Scheuermann kyphosis have negative balance before surgery and have slightly more negative balance after surgery. Lumbar hyperlordosis was reduced from an average of 75 degrees before surgery to 55 degrees after surgery.
Tightness and contracture of pectoral and hamstring muscles is common.27 One should look for cutaneous lesions, foot deformities, or muscle contractures. These may signal an underlying neurologic problem. A complete neurologic examination should be performed. Although neurologic findings are rare in Scheuermann disease, spinal cord compression has been reported.18,28–31 Causes of cord compression include thoracic disc herniation, dural cysts, or severe kyphosis.
Imaging Studies
Routine radiographs include standing posteroanterior and lateral 36-inch films. Sorenson’s criteria (three consecutive wedged vertebrae of ≥5 degrees) are used as diagnostic criteria. On the lateral view, the fists are placed in the supraclavicular fossa to visualize the upper thoracic spine better. Arm position has a tendency to displace the C7 plumb line. Patients with Scheuermann kyphosis typically have normal or negative sagittal balance, however. It is important to be consistent with the methods used when obtaining x-rays in the preoperative and postoperative periods. A supine hyperextension bolster lateral view is useful in assessing the flexibility of the deformity and can help differentiate it from postural kyphosis.32 Other radiographic abnormalities that may be present, such as spondylolysis, scoliosis, disc space narrowing, and endplate irregularities, should be noted.
All patients with a rapidly progressive kyphosis, neurologic abnormalities, or any evidence of congenital kyphosis should undergo magnetic resonance imaging (MRI). One report showed transient paraparesis owing to thoracic spinal stenosis and recommended preoperative MRI in patients undergoing surgical correction.33 Thoracic disc herniations are known to occur with increased frequency in patients with Scheuermann disease.34,35 The issue of whether all surgical patients should undergo MRI preoperatively is controversial; the authors’ practice is to obtain MRI in all patients before surgery to rule out stenosis, disc herniation, or other pathologies.
Natural History
Several early studies suggested an ominous natural history for Scheuermann disease, with significant back pain, embarrassment about physical appearance, interference with social functioning, and cardiopulmonary failure.11,36–40 Ponte and colleagues36 showed in their series that all curves greater than 45 degrees progressed during the adolescent growth spurt and continued to increase after age 30. Sorensen11 reported a 50% incidence of pain during the adolescent growth spurt, and a high rate of pain was noted in patients with kyphosis greater than 60 degrees.37 Other studies noted the often unremitting and incapacitating nature of the pain, progressive nature of the deformity, risk of cardiopulmonary failure, and unacceptable appearance of the deformity in untreated adults.38–40 Aggressive surgical treatment was recommended to prevent these problems in the future.40
In 1993, Murray and colleagues18 provided the first long-term follow-up study on the natural history of untreated Scheuermann disease in patients with an average age of 53 years and average kyphosis of 71 degrees. These investigators found that 64% of patients (compared with 15% of controls) reported back pain. The proportion of patients who had pain that interfered with their daily lives was not significantly different, however, from control subjects. Their data suggested that although patients with Scheuermann disease may have some functional limitations, they do not have major interference with their lives. Murray and colleagues18 found that their patients adapted reasonably well to this condition and recommended that surgical treatment should be carefully reviewed. Other reports have also suggested the generally benign natural history of this condition.41–43
The natural history is more favorable when the deformity is in the thoracic spine, rather than the thoracolumbar spine. Back pain is much more common in the latter. It is believed that thoracolumbar kyphosis has a higher incidence of progression because of the lack of support provided by the surrounding rib cage.44 When a thoracolumbar kyphosis exceeds 50 to 55 degrees, the deformity is readily apparent, especially in thin patients, and pain is common.44 The thoracolumbar spine is typically neutral to slightly lordotic, and any degree of kyphosis may be clinically apparent. In adults, degenerative disc disease is frequently seen at the apical segments of the kyphosis and may be a source of back pain.45,46
Although progression of deformity can be rapid during the adolescent growth spurt, it is unknown whether the deformity would progress after skeletal maturity is reached. Thoracic curves greater than 80 degrees and thoracolumbar curves greater than 55 to 60 degrees may be at risk of progression after skeletal maturity, although the true incidence of progression is unknown.10,44 If nonsurgical treatment is chosen for curves of this magnitude, periodic follow-up is recommended into adulthood.
Pulmonary failure secondary to severe deformity is very rare. Murray and colleagues18 found that lung volume, lung mechanics, and diffusing capacity were not significantly affected and were normal in patients with curves less than 100 degrees. They found that as the deformity reaches 100 degrees, restrictive lung disease occurs more often when the curve apex is between T1 and T8.
Nonsurgical Treatment
The use of the Milwaukee brace for the treatment of scoliosis was first reported by Blount and colleagues in 1958.47 In 1959, Moe began treating Scheuermann kyphosis with the Milwaukee brace.38 In 75 patients who completed treatment, the kyphosis improved by 40%, and the vertebral wedging improved by 42%. Bradford and colleagues38 reported factors that limited the amount of correction included kyphosis greater than 65 degrees, skeletal maturity, and vertebral wedging averaging more than 10 degrees.
Sachs and colleagues32 found that curves less than 74 degrees in skeletally immature patients can be successfully treated in a Milwaukee brace. They reported 120 patients with Scheuermann disease who were treated with the Milwaukee brace with more than 5 years of follow-up; 76 patients had improvement in kyphosis, 10 patients had no change in kyphosis, and 24 patients had worsening of deformity compared with initial studies. One third of patients with an initial kyphosis of 75 degrees or greater subsequently underwent surgery. Results showed that treatment with the Milwaukee brace consistently improved kyphosis by approximately 50% during the active phase of treatment, but some loss of correction occurred over time. The final result showed improvement in 69% of patients.
Gutowski and Renshaw48 reported 75 patients treated with either a Milwaukee or Boston brace. For compliant patients, the average improvement in kyphosis was 27% in the Boston orthosis group and 35% in the Milwaukee orthosis group, despite the fact that patients in the former group were younger and had smaller, more flexible curves. Compliance with orthosis wearing was twice as likely with the Boston orthosis (61% compliance vs. 29% compliance for Milwaukee orthosis). Results in patients who wore their orthoses at least 16 hours per day were equal to results in patients with 23 hours of daily wear. The Boston brace provided satisfactory correction in curves less than 70 degrees and had better compliance. For larger curves, a Milwaukee brace was recommended.
Ponte and colleagues36 reported on 1043 patients treated with casts for 8 to 16 months, followed by Milwaukee brace and physical therapy until skeletal maturity. Patients had a mean initial curve of 57 degrees and at 3-year follow-up had a mean 62% wedge improvement and 40% curve correction.
If bracing is chosen, physical therapy should be initiated for trunk stabilization and postural exercises and to stretch the pectoral and hamstring muscles. The brace should be worn for 23 hours a day. To get a meaningful correction with brace treatment in Scheuermann disease, correction of the vertebral wedging deformity by bone remodeling is necessary. In contrast to scoliosis, in which bracing does not correct the curve, bracing in Scheuermann disease may help achieve some curve correction. After 12 to 18 months of bracing, partial reversal of anterior wedging of vertebral bodies is often noted.10 Loss of correction can occur, however, after discontinuation of the brace. Montgomery and Hall24 reported an average loss of correction of 15 degrees in 21 patients 18 months or more after they stopped wearing the brace. Brace treatment initially leads to some correction by opening the disc spaces, which close down again unless sufficient time is allowed to reverse the wedging of the vertebral bodies.
Indications for Surgery
Neurologic compromise is an indication for surgery, but it rarely occurs in Scheuermann disease. Cord compression may be due to disc herniation at the apex, severe kyphosis, and extradural cysts.34 Similarly, pulmonary compromise is rare and does not occur until the curve is greater than 100 degrees.7,18,40,43
Surgical Treatment
The surgical options for Scheuermann disease include posterior-only correction and fusion, combined anterior and posterior fusion, and anterior-only procedures. Historically, the surgical treatment of Scheuermann disease consisted of apical anterior release and fusion followed by posterior fusion. This approach originated from work by Bradford and colleagues49 in 1975, in which they found an unacceptably high rate of correction loss after posterior-only fusion with Harrington compression instrumentation. These investigators reported a 9% pseudarthrosis rate and 23% risk of instrumentation complications. In 1980, work from the same institution showed solid fusion and good maintenance of correction with anterior release and fusion followed by posterior compression instrumentation in 24 patients.39
The efficacy of combined anterior release and posterior fusion is well documented in the literature.39,50–52 Anterior release traditionally has been recommended for patients with severe, rigid deformities that do not correct to less than 50 degrees on a hyperextension lateral radiograph. With use of modern pedicle screw instrumentation, the indications for performing an anterior release are less common, however, and even severe deformities are being successfully treated with a posterior-only approach.
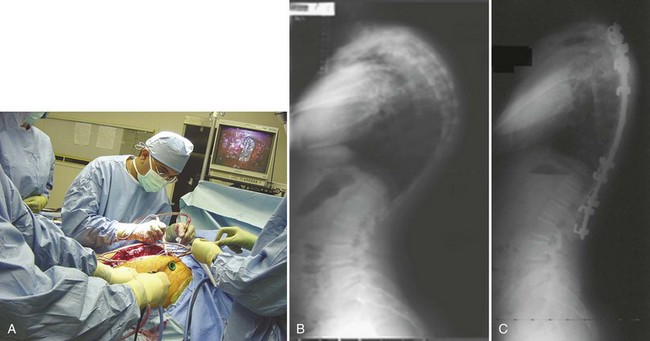
The anterior release can be performed through an open thoracotomy or thoracoabdominal approach depending on the location of the apex of the deformity or can be performed through a video-assisted thoracoscopic surgery approach.53,54 The senior author has achieved excellent results with simultaneous video-assisted thoracoscopic surgery release and posterior fusion and instrumentation in the prone position (Fig. 26–2). The levels requiring anterior release typically include six to eight segments centered around the apex of the deformity. The anterior longitudinal ligament and entire disc are removed, and the space is packed with fibular structural allograft bone. In very severe deformities, an intervening period of halo-femoral traction may be considered between the anterior and posterior procedures.
Anterior release and fusion ensures that correction is reliably achieved and solid fusion is obtained. There is, however, the obvious morbidity of the additional operating time and reported complications including hemothorax, pneumothorax, and pulmonary embolism.7,50,55 There may be potential negative effects on pulmonary function, which may not return to baseline even at 2 years postoperatively.56–58 Although anterior surgery has benefits in achieving correction of severe deformities, the additional surgery is not without consequence.
Over the last 3 decades, several studies have shown good results with posterior-only fusion and instrumentation with various constructs.37,55,59–62 Speck and Chopin37 found posterior-only fusion to be adequate in skeletally immature patients, but that combined anterior and posterior surgery is needed for skeletally mature patients.
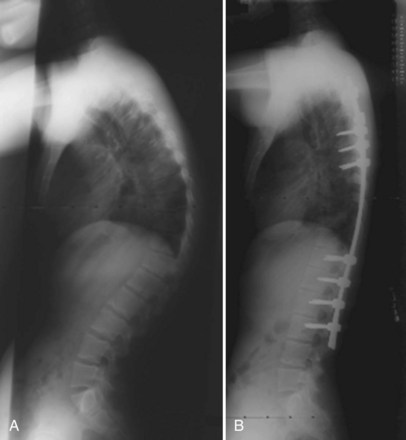
In 1984, Ponte and colleagues63 described shortening of the posterior column by employing multiple osteotomies and posterior compression instrumentation and fusion. The Ponte osteotomy is similar to the Smith-Peterson osteotomy except that it is performed at multiple levels in the thoracic spine (Figs. 26-3 and 26-4). Smith-Peterson’s original osteotomy was in the lumbar spine, at one level, in patients with rheumatoid arthritis.64 After Ponte’s description in 1984,65 this procedure did not gain popularity for many years, especially among North American surgeons, until pedicle screw instrumentation became popular in the thoracic spine. As pedicle screws became more widely used and the ability to obtain strong, three-column fixation in the spine became possible, several studies have documented successful results with posterior-only treatment of more severe deformities.66,67
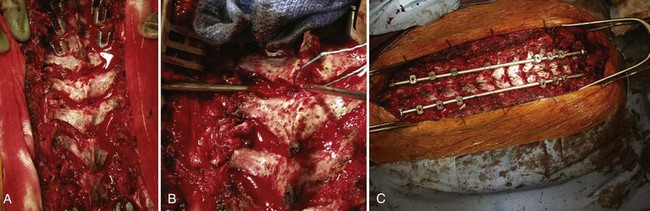
FIGURE 26–4 A-C, Multilevel Ponte osteotomies performed on the patient shown in Figure 26–3. Removal of ligamentum flavum and superior and inferior facets out through neural foramen allows shortening of posterior column and correction of kyphosis.
Lee and colleagues67 compared posterior-only fusion (18 patients) with combined anterior and posterior fusion (21 patients) and found better correction and fewer complications in the posterior-only group at a mean 2-year follow-up. The anterior and posterior group did not have Ponte osteotomies, and hybrid hook and screw constructs were used, whereas the posterior-only group had Ponte osteotomies (in 67%) and had all pedicle screw constructs.
Geck and colleagues66 obtained good correction in 17 patients employing multiple osteotomies and pedicle screw fixation, averaging 9.3 degrees of correction per osteotomy across the apex. There is growing evidence that anterior release may be unnecessary to obtain satisfactory correction of even severe deformities if multilevel segmental osteotomies are performed in conjunction with pedicle screw fixation.66–68 Hosman and colleagues68 suggested that posterior-only correction is often adequate for correcting up to a 100-degree kyphosis to a physiologic range of 40 to 50 degrees without an anterior release.
Surgical Principle
Degree of Deformity Correction
Surgical treatment of Scheuermann kyphosis should aim to correct the thoracic kyphosis to the high-normal range of thoracic kyphosis (40 to 50 degrees). Overcorrection of a kyphotic deformity can lead to neurologic complications, postoperative sagittal malalignment, and proximal junctional kyphosis. The last condition may occur as a result of forces being transferred to the proximal junction after an aggressive corrective maneuver.10,51,68 Lowe and Kasten26 recommended that no more than 50% of the preoperative kyphosis be corrected and that the final kyphosis should never be less than 40 degrees. These authors also found that the negative sagittal balance is worsened postoperatively, and this may predispose patients to junctional kyphosis.26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree