Patient History and Exam
Hal David Martin
Introduction
Over many generations of orthopedic surgeons, the evaluation of the hip has improved and continues to evolve as our understanding of anatomy and biomechanics advance (1,2,3,4,5,6,7,8,9). Throughout history many of the early diagnostic tests of the hip involved muscle contracture, such as the Thomas test, Ober test, and Ely test; and over time the evaluation of hip pain broadened to include range of motion, muscle strength, neurovascular, proprioception, bony geometry; as in the Patrick test, Stinchfield test, Pace test, Trendelenburg gait, and Craig test. Building upon this background, provocative techniques to evaluate the hip were developed, for example the flexion adduction internal rotation (FADDIR) test, the “log roll,” and McCarthy test (1,7). As technology advances and our understanding of the hip joint progresses, new techniques and new diagnostic tests continue to develop (10). In a review of the published literature, there is evident variability in the way that hip specialists evaluate and examine their patients (Table 10.1) (10). The most consistently utilized examination for hip pathology is the FADDIR test (2,3,11,12,13,14,15,16,17,18,19,20,21,22,23), also sometimes referred to as the “impingement test” (20). There is a common base for these different tests in regard to determining an intra-articular source of the hip pain; however, due to a lack of consistent technique and standardization among hip specialists (2,6,13,24,25,26,27), there is a need for improved reliability for the advancement of the clinical evaluation of the hip (21,28). One study reported that the agreement of six orthopedic surgeons for the diagnosis of labral tear, femoroacetabular impingement (FAI), and laxity was 63, 65, and 58% respectively (28). The Multicenter Arthroscopy of the Hip Outcomes Research Network (MAHORN) (21) has determined a common set of clinically important diagnostic techniques of 33 points for evaluating adult hip pathology, comparing favorably to other joints such as the shoulder and the knee and raising awareness for an international consensus and terminology.
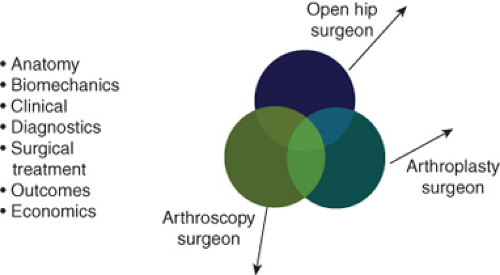
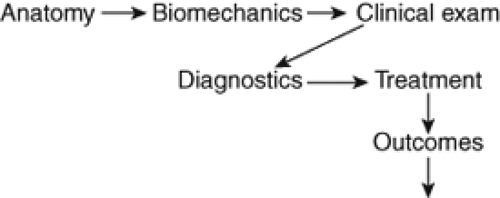
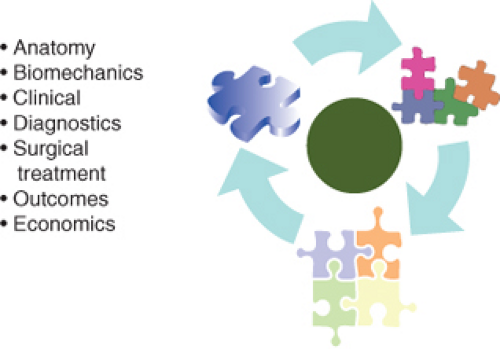
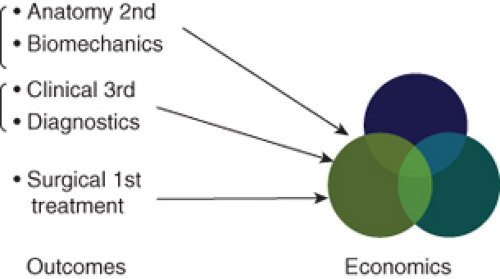
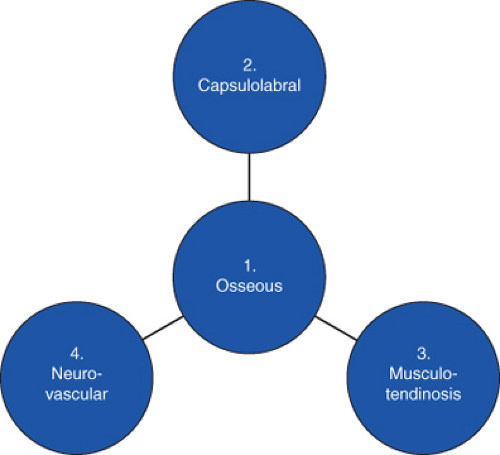
The main objective of the orthopedic hip surgeon, whether it is the open hip surgeon, the arthroplasty surgeon, or the arthroscopic surgeon, is to thoroughly assess the patient outlining and defining the presenting hip pathology. All surgeon groups share this common goal by evaluating the key components to aid in understanding hip pathology (Fig. 10.1). The advancement of surgical treatment does not always proceed linearly through anatomy, biomechanics, clinical examination, diagnostic tests, treatment, then outcomes (Fig. 10.2). Rather, it has developed over time in a more random manner, placing pieces of the puzzle together throughout history (Fig. 10.3). To get through the puzzle more quickly, it is important for the physical examination to lead to an accurate diagnosis in all four layers the osseous, capsulolabral, musculotendinous, and neurovascular (Fig. 10.4).
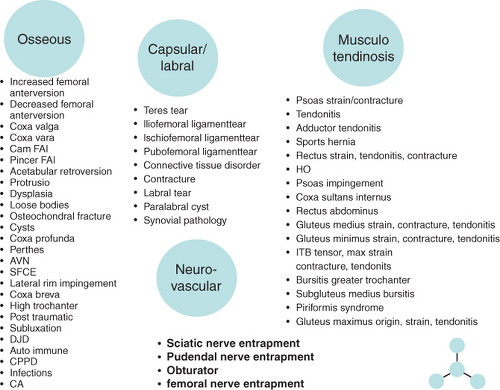
The physical examination of the hip should be performed in a manner that allows the detection of pathologic conditions occurring in the hip in four layers and three planes (Fig. 10.5). Pathologic conditions exist in a single layer or in multiple layers requiring a standardized examination to be followed. Examples of the many different diagnoses of each layer are given in Fig. 10.6. The history is required to help delineate these layers in addition to a comprehensive physical examination. The progression of hip pathology may follow strictly an inside out from osseous to musculotendinous and neurovascular pattern or can have primary associated issues. Acute or chronic conditions may have different patterns and a standardized examination would allow the detection of both. The establishment of a pattern grid or battery of diagnostic tests
as the background on which to cast the light of the pathologic condition is a key for the recognition of any complex pattern. More importantly, the history and physical examination of the hip will direct the differentiation of intra-articular versus extra-articular sources of pain along with the location of the presenting pain and the presence or absence of popping/locking. Reliability is increased by having a standardized examination. Extra-articular sources of pain often respond well to nonoperative treatment, whereas intra-articular sources require further workup, which may include x-rays (4,13,17,18,20,21), magnetic resonance imaging (MRI) (12,15), MRI arthrogram (2,11,16,19), or injection tests (14,29,30).
as the background on which to cast the light of the pathologic condition is a key for the recognition of any complex pattern. More importantly, the history and physical examination of the hip will direct the differentiation of intra-articular versus extra-articular sources of pain along with the location of the presenting pain and the presence or absence of popping/locking. Reliability is increased by having a standardized examination. Extra-articular sources of pain often respond well to nonoperative treatment, whereas intra-articular sources require further workup, which may include x-rays (4,13,17,18,20,21), magnetic resonance imaging (MRI) (12,15), MRI arthrogram (2,11,16,19), or injection tests (14,29,30).
Table 10.1 Physical Examination Maneuvers Reported in the Current Literature | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The goal of this chapter will be to review the key components of the history and key common test patterns encompassing all of the anatomical layers as well as specific more infrequently used physical examination techniques in the hip, that is, differential diagnosis of extra-articular sources of hip pain.
History and Physical Examination
History
A comprehensive history of the patient is obtained before the physical examination of the hip. The first aspects for consideration of treatment are patient age and presence or absence of trauma (31). History of trauma may be indicative of a treatable problem, whereas the absence of trauma may suggest degenerative disease or a predisposition to injury (32). The present condition is documented including the date of onset, mechanism of injury, pain location, factors which increase or decrease the pain, previous consultations, surgical interventions, and past injuries (3,6,10,25). A history of sports and recreational activities help to determine the type of injury (6,10,25,33). Rotation sports, such as golf, tennis, ballet, and martial arts, have been commonly associated with injuries to the intra-articular structures including the labrum, iliofemoral ligament, and ligamentum teres. Any prior treatments the patient has used must be recognized, such as rest, physical therapy, ice, heat, nonsteroidal anti-inflammatories, surgery, injections, orthotics, or the use of support aids.
Functional limitations of patient are documented, which may involve getting in or out of the bathtub or car, activities of daily living, jogging, walking, and or climbing stairs. Several questionnaires are available providing a quantitative and qualitative description of the patient’s functional ability. The modified Harris Hip Score (34) (HHS) is the most documented and standardized functional score to date, which is a quantitative score based on pain and function. Other hip scores have been outlined with quantifications in more specific patient populations such as Merle d’Aubigné (MDA) (35), the Non-Arthritic Hip Score (NAHS) (36), Musculoskeletal Function Assessment (MFA) (37), Short Form 36 (SF-36) (38), and the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) (39). Recently, the MAHORN group has created a new 33-item quality-of-life outcome measure, the International Hip Outcome Tool (IHOT), which is reliable, valid, and responsive. The use of a verbal analog score is also subjectively useful.
Symptoms related to the back, neurologic system, abdomen, or lower extremity complaints must also be recognized (6,10). Thoracolumbar problems are occasionally confused with the hip as a portion or dominant cause of complaint. Associated complaints, such as pain in the abdomen or back, numbness, weakness, cough or sneeze exacerbation help to identify thoracolumbar issues (6,10). In addition, night pain, sit pain, weakness, numbness, or paresthesia in the lower extremity may suggest neural compression which may occur in the lumbar spine or within the subgluteal space (40).
The vascular supply to the femoral head, and any possible sources of disruptions, are screened including metabolic disorders, such as abnormality of lipids, thyroid, homocysteine, and clotting mechanisms (6,10). Factors related to the patient’s social history that can affect the blood supply to the femoral head are reviewed including the presence or use of tobacco, alcohol, steroids, or altitude issues. Family medical history is also taken into account including hip dislocations or disorders, degenerative joint disease, rheumatologic disorders, or cancer.
Patient goals and realistic expectations of treatment are discussed. Patients may differ from surgeons regarding the issues they feel are important when considering treatment outcomes (41). Communication, understanding, empathy, and compassion are important to obtaining an accurate history. A comprehensive history evaluation is presented in Table 10.2.
Physical Examination
Standing Examination
The one-finger rule (Fig. 10.7A) will help to direct the examination, as the patient stands a general point of pain is noted with one finger (32). The groin region directs a suspicion of intra-articular problem and lateral-based pain is primarily associated with both intra- or extra-articular aspects. The “C sign” (Fig. 10.7B) is a characteristic sign of patients with intra-articular hip pain (1). The patient will hold their hand in the shape of a C and place it above the greater trochanter with the thumb positioned posterior to the trochanter and fingers extending into the groin (1). This finding can be misinterpreted as lateral soft tissue pathology such as trochanteric bursitis or the iliotibial band, however the patient is often describing deep interior hip pain (1). Posterior-superior pain requires a thorough evaluation in differentiating hip and back pain (40). The evaluation of leg length discrepancies can be done in the standing position by noting shoulder and iliac crest heights (Fig. 10.8A,B). Incremental wooden blocks placed under the short side heel, aid in orthotic considerations. General body habitus is assessed and ligamentous laxity issues are examined by the middle finger test, thumb test, or hyperextension of the knees or elbows. Structural versus nonstructural scoliosis is differentiated by forward bending (Fig. 10.9A,B). The degree of lumbar flexion range of motion is recorded and side bending range of motion is also useful (Fig. 10.9C,D).
Observation of a patient’s gait and single leg stance is an important aspect of the physical examination of the hip (21). Gait abnormalities (Table 10.3) are often present with hip pathology (42,43). Proper functioning of the hip joint involves three biomechanical planes of the femur and acetabulum. The relationships of joint stability, the labrum, and articular cartilage are important for the transfer of dynamic and static loads to the ligamentous and osseous structures (43).
Gait (Fig. 10.10) is observed in an area large enough for six to eight stride lengths. Key points of gait evaluation include foot rotation (internal/external progression angle), pelvic motion in the coronal and transverse planes, stance phase, and stride length. Arm swing, which is a trigger for the contralateral gluteus maximus, is also noted. Gait viewed from the foot progression angle will detect osseous or static rotatory malalignment as exists with increased or decreased femoral anteversion versus a capsular or musculotendinous issues. The knee and thigh are observed simultaneously to assess any rotatory parameters. The knee may want to be held in either the internal or external rotation to allow proper patellofemoral joint alignment, but may produce a secondary abnormal hip rotation. Excessive internal rotation is usually present in cases of increased femoral anteversion or acetabular retroversion. Excessive external rotation is usually present in cases of increased femoral retroversion or increased acetabular anteversion. Torsional abnormality
or effusion can lead to abnormal foot progression angles, which will trigger a battle between the hip and knee for a comfortable position which will affect the gait. In cases of a painful gait, note the anatomical location of pain and at what point within the gait phase pain presents.
or effusion can lead to abnormal foot progression angles, which will trigger a battle between the hip and knee for a comfortable position which will affect the gait. In cases of a painful gait, note the anatomical location of pain and at what point within the gait phase pain presents.
Table 10.2 Complete Review of Patient History | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
Noting iliac crest rotation and terminal hip extension assesses pelvic rotation. On average, normal gait requires 6 to 8 degrees of hip rotation and 7 degrees of pelvic rotation, equaling a total rotation of 15 degrees (42). The pelvic wink is demonstrated by an excessive rotation in the axial
plane toward the affected hip, thus producing extension and rotation through the lumbar spine, to obtain terminal hip extension. This winking gait can be associated with intra-articular hip pathology, anterior capsule laxity, or hip flexion contractures; especially when combined with increased lumbar lordosis or a forward-stooping posture. Gait changes can affect spinal mechanics and function. Excessive femoral anteversion, or retroversion, can affect a wink on terminal hip extension as the patient will try to create greater anterior coverage with a rotated pelvis. Injury to the anterior capsule can also contribute to a winking gait.
plane toward the affected hip, thus producing extension and rotation through the lumbar spine, to obtain terminal hip extension. This winking gait can be associated with intra-articular hip pathology, anterior capsule laxity, or hip flexion contractures; especially when combined with increased lumbar lordosis or a forward-stooping posture. Gait changes can affect spinal mechanics and function. Excessive femoral anteversion, or retroversion, can affect a wink on terminal hip extension as the patient will try to create greater anterior coverage with a rotated pelvis. Injury to the anterior capsule can also contribute to a winking gait.
 Figure 10.8. Standing length discrepancy. A, B: Shoulder and iliac crest heights are examined with the patient with dynamic loading of the hip joint in the standing position. |
Table 10.3 Standing Examination Assessment | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 Figure 10.10. Gait evaluation. Gait of about six to eight stride lengths is observed from the posterior and anterior views. |
During the stance phase, body weight must be supported by a single leg with the gluteus maximus, medius, and minimus providing the majority of force (42). Maximum ground reactive force occurs upon heel strike at 30 degrees of hip flexion (42). A shortened stance phase can be indicative of neuromuscular abnormalities, iliotibial band pathology, trauma, or leg length discrepancies. The abductor deficient gait (Trendelenburg gait or abductor lurch) is an unbalanced stance phase attributed to abductor weakness or proprioception disruption. This pattern may present in two ways: with a shift of the pelvis away from the body (a “dropping out” of the hip on the affected side), or with a shift of the weight over the adducted leg (a shift of the upper body “over the top” of the affected hip). The antalgic gait is characterized by a shortened stance phase on the painful side limiting the duration of weight bearing (a self-protecting limp caused by pain). A short leg gait is noted by the drop of the shoulder in the direction of the short leg. Trauma, fracture, or synovial inflammation can contribute to an antalgic gait.
In addition to body habitus and gait evaluation, the single leg stance phase test (Fig. 10.11) is performed during the standing evaluation of the hip (21). The single leg stance phase test is performed on both legs, with the nonaffected leg examined first, to establish a baseline. During this test, the examiner stands behind the exposed patient (to the degree the bony landmarks are easily observed). The patient stands with feet shoulder width apart then brings one leg forward by flexing the leg to 45 degrees at the hip and 45 degrees at the knee, thereby simulating the single leg stance phase with load on the examined hip. This position is held for 6 seconds. As the patient lifts and holds one foot off the ground the contralateral hip abductor musculature and neural loop of proprioception are being tested. The pelvis will tilt toward or away the unsupported side if the musculature is weak or if the neural loop of proprioception is disrupted. Normal dynamic mid-stance translocation is 2 cm during a normal gait pattern (42




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree