Chapter 132 Patellar Fractures in Total Knee Arthroplasty
Extensor mechanism problems frequently are cited as among the most common reasons for failure after total knee arthroplasty (TKA).21,22,26 This may have changed as surgeons have learned more about the importance of tibial and femoral rotational alignment,1 patellar component and trochlear groove design, and optimal patellar resurfacing techniques. Nevertheless, patellar fractures still occur after TKA.2,3 About half of patellar fractures heal without major consequence; unfortunately those that do not often are associated with serious problems.17 Patellar fracture after TKA occurs far more commonly in resurfaced than in non-resurfaced patellae. A large proportion of fractures occur in the absence of a clear traumatic event. This chapter reviews risk factors for fracture, fracture classification, fracture results, and techniques of fracture management.
Prevalence and Risk Factors for Patellar Fracture
The prevalence of patellar fracture varies in different series, with most reports describing between 0.5% and 6% for resurfaced patellae.* The prevalence is higher after revision TKA.2 Prevalence probably varies according to many factors, including patient demographics, implant design, and surgical technique. The reported prevalence also undoubtedly varies in part in terms of completeness of follow-up for this complication. As surgeons and implant designers have become more aware of what causes extensor mechanism problems and how to prevent them, there is reason to believe that the incidence of patellar fracture has declined or shall decline.
The strongest risk fracture for patellar fracture is resurfacing of the patella.16,36 Grace and Sim16 reported that the risk of fracture of non-resurfaced patellae was only 0.05%. Gender is a risk factor for fracture, and unlike most periprosthetic fractures, men are at higher risk for fracture than women. In the series of Ortiguera,28 the overall prevalence of fracture in 12,246 consecutive TKAs was 0.68%. The prevalence was 0.40% in women, but 1.01% in men. One possible reason for the higher incidence in men could be the capability to generate greater quadriceps forces. Analysis of large patient groups by Meding and associates27 from Indiana and Tamachote and colleagues39 from the Mayo Clinic has demonstrated that increased body mass index (BMI) is a risk factor for fracture. Diagnosis leading to TKA and age at TKA have not yet been demonstrated to be major risk factors for patellar fracture.
Most patellar fractures are not associated with a substantial traumatic event. In the series of Ortiguera,28 11 of 78 fractures were associated with a blow to the knee, 6 occurred as the patient stood from sitting, 5 spontaneously while walking, 3 with knee hyperflexion, and 2 in patients with previous patellar subluxation; notably, in 48 patients, no clear event leading to fracture was recognized.
Technical and design factors also probably affect risk of fracture. Revision arthroplasty patients are at higher risk than primary TKA patients. The thickness of the patella probably affects risk, and both very thin and very thick resurfaced patellae are at increased risk. Thin patellae are likely at risk because of bone weakness. Erak and coworkers13 reported that fractures were more common in revision TKA with an inset “biconvex” patellar component when the patellar remnant measured less than 6 mm in thickness.
Some patellar fractures clearly appear to occur in the presence of patellar osteonecrosis, but a clear link between lateral retinacular release and patellar fracture has not been established, and papers have been published both for and against an association.25,31–33,37 Lateral retinacular release has been shown by scintigraphy methods30 to produce transient patellar hypovascularity. However, Kusuma and associates23 evaluated 1108 consecutive TKAs, of which 314 had a lateral retinacular release, and reported no cases of patellar fracture.
Malalignment of the limb and of tibial and femoral implants has clearly been shown to increase patellar fracture risk.14 In Ortiguera’s series,28 76% of patients had a major limb or implant axial malalignment and 6% a minor malalignment by Figge’s criteria.14 Seventeen of 18 patients in Tria’s series41 had a minor malalignment. In recent years, the strong relationship between malrotation of tibial and femoral implants and extensor mechanism complications, including patellar fractures, has increasingly been demonstrated.1 Certain femoral component designs with a boxy configuration on lateral projection may have been associated with higher patellar fracture risk. Patellae of certain designs,43 including some components with a large central peg (as opposed to a three-anchoring-peg design), also may be associated with increased fracture risk.24
Little has been written about the chronology of patellar fractures after TKA, but they seem to occur most often in the first several years after TKA.9 Ortiguera and Berry28 reported that 82% of fractures occurred in the first 3 years after TKA, with 46% recognized in the first year. In the series of 18 fractures reported by Tria and colleagues,41 fractures occurred from 3 to 22 months postoperatively, with a mean at 11 months postoperatively.
Classification
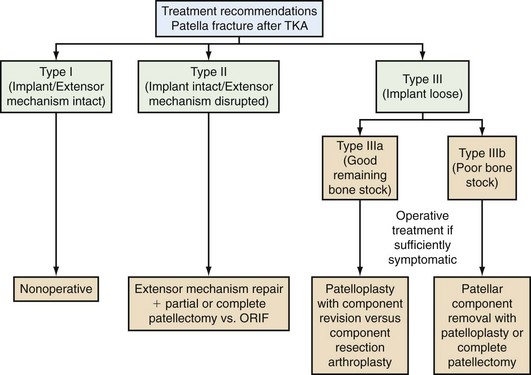
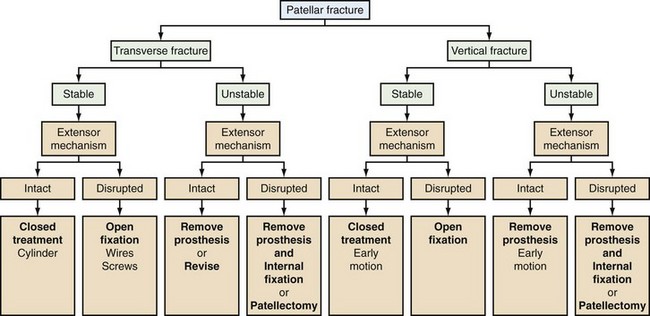
Several different classification schemes for patellar fractures around TKA have been proposed35 (Figs. 132-1 and 132-2). The classification of Goldberg and coworkers15 considers fracture pattern, extensor mechanism disruption, and patellar subluxation. Type I fractures do not have disruptions of the extensor mechanism or implant fixation; type II fractures do have disruption of the extensor mechanism or implant fixation; type IIIa fractures have a disrupted extensor mechanism with an inferior patellar pole fracture; type IIIb fractures have the same characteristics as IIIa but with an intact extensor mechanism; and type 4 fractures are patellar fracture-dislocations. Hozack and associates19 used a classification that included fracture displacement, presence or absence of extensor lag, fracture location, and failure of previous treatment.
The classification of Ortiguera and Berry28 (Table 132-1) focuses on three main factors: integrity of the extensor mechanism, fixation status of the patellar implant, and remaining patellar bone stock. Type I fractures have an intact extensor mechanism and a fixed patellar component, type II fractures have a functionally disrupted extensor mechanism, and type III fractures have a loose implant but an intact extensor mechanism. Type III fractures are further subdivided as IIIa (satisfactory remaining bone stock for patellar component revision) and IIIb (unsatisfactory remaining bone stock for patellar component revision).
Table 132-1 Classification of Periprosthetic Patellar Tracking According to Ortiguera
| Type I | Extensor mechanism intact; patellar implant well fixed |
| Type II | Extensor mechanism disrupted |
| Type IIIa | Patellar implant loose; patellar bone stock allows revision |
| Type IIIb | Patellar implant loose; patellar bone stock does not allow revision |
From Ortiguera CJ, Berry DJ: Patellar fracture after total knee arthroplasty. J Bone Joint Surg Am 84:532–540, 2002.
Results
Minimally displaced or nondisplaced fractures with an intact extensor mechanism commonly are successfully treated nonoperatively with satisfactory results. Ortiguera and Berry28 reported that all but 1 of 38 such fractures were treated successfully without operation. In the series of Parvizi and associates,29 six of seven patients with such fractures had good results with nonoperative (cast or brace) treatment. In Goldberg’s series,15 good results of treatment also were seen in 16 patients with an intact extensor mechanism.
Fractures associated with a disrupted extensor mechanism have had the poorest results. In the series of Ortiguera and Berry28 11 of 12 patients with this type of fracture were treated operatively, and complications occurred in 6 of these patients. Only one of six patients treated with open reduction and internal fixation went on to bone-to-bone healing of the patella, and three of four patients treated with fragment excision and tendon advancement to bone had complications necessitating reoperation. Seven of the 12 patients had residual pain, weakness, or extensor mechanism instability. In the series of Goldberg and colleagues,15 five of eight patients with an inferior pole fracture and a disrupted extensor mechanism had poor results. Keating and coworkers20 reported on 17 patients with a disrupted extensor mechanism: 2 were treated with open reduction and internal fixation, and neither healed.
For fractures associated with a loose patellar component, results vary considerably. In the series of Ortiguera and Berry28 a few patients with sufficient bone stock for patellar component revision (2 of 28 fractures with a loose implant) did well, as did many patients with sufficiently fewer symptoms to allow nonoperative treatment of this fracture type. When patients required resection arthroplasty and partial or complete patellectomy, the results were less satisfying: six of eight knees treated with resection arthroplasty and partial patellectomy remained symptomatic, and two of three knees treated with patellectomy remained symptomatic. Goldberg and colleagues15 reported poor results in four of six patients with a loose patellar component. Keating and coworkers20 reported that infection developed in four of nine patients treated with patellar component excision for an extruded patellar component in association with patellar fracture. Chang and associates8 reported on 9 knees treated with patellectomy for comminuted patellar fracture after TKA: 2 of 12 patients had a complication of extensor mechanism disruption, 2 were unable to use stairs, and 4 patients had some mild extensor lag (less than 10 degrees). They concluded that patellectomy often provided satisfactory pain relief, but that functional results were often poor.
Treatment
A number of different fracture treatment algorithms have been proposed based on different fracture classification methods.4,5,34 The Ortiguera classification method may be used as a framework for treatment of periprosthetic patellar fractures.
Type I Fractures
A great majority of type I fractures may be treated nonoperatively with a good likelihood of a favorable result (Fig. 132-3). At the time of presentation, the orthopedist should attempt to understand the time frame during which the fracture occurred. In many patients, these fractures occur spontaneously and are asymptomatic, and the first time they are found is on a routine follow-up radiograph. If it appears that the fracture is not acute and that it occurred at an indeterminate time in the past, discussion of the finding with the patient followed by observation alone is appropriate for most asymptomatic or minimally symptomatic patients. For acute fractures, the goal is to prevent notable displacement that could lead to functional extensor mechanism disruption. In most cases, this means protection or immobilization with a knee immobilizer or a cast for about 6 weeks. Depending on the clinical course and serial radiographic findings, the patient may progress to gentle passive motion of the knee at some point during the first 6 weeks of treatment in selected cases. The more at risk for displacement the fracture, the more cautious the orthopedist should be in progression of range-of-motion and active quadriceps activities. Many fractures will go on to bony healing, others to fibrous healing with an intact extensor mechanism; most eventually will be asymptomatic.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree