Chapter 69 Overview of Psoriatic Arthritis
General Considerations
Psoriatic arthritis is defined as arthritis, spondylitis, or dactylitis occurring in association with the skin disease psoriasis (PsO). The recent CASPAR criteria for PsA (Box 69-1) dramatically explain the spectrum of this disorder by allowing the inclusion of patients who do not currently have psoriasis, but have a past history of psoriasis or a family history of psoriasis.7 The criteria also recognize the importance of changes in the nails, as well as changes in the skin.
Box 69-1
From Taylor WJ, Gladman D, Helliwwell P et al: Classification criteria for psoriatic arthritis; development of new criteria from a large international study. Arth Rheum 54(8):2665–2673, 2006.
Caspar Criteria for Psoriatic Arthritis
Epidemiology
The National Psoriasis Foundation has estimated that PsO affects 1% to 3% of the population.3,4 Estimates of the prevalence of PsA in patients with PsO are 15% to 39%, with the higher estimates being based on patient series in which patients have actually been examined. As a consequence, PsA is likely a more common disorder than rheumatoid arthritis.
Patterns of Arthritis
Moll and Wright have described five patterns of PsA, which are listed in Box 69-2.5 Any given patient may present with a combination of arthritis, spondylitis, dactylitis, and enthesitis (insertional tendinitis).
Box 69-2 Moll and Wright Classification of Psoriatic Arthritis*
The arthritis itself tends to be preferentially involves large joint, is lower extremity predominant, and is often asymmetrical (Fig. 69-1). It frequently involves the foot and ankle and may involve the axial skeleton. The arthritis is often palindromic, unlike the additive pattern seen in rheumatoid arthritis (RA). Spine involvement often begins in the cervical spine rather than the lumbar spine, which serves to distinguish it from ankylosing spondylitis. Insertional tendinitis is a prominent feature that may dominate the clinical presentation. The net effect of the disease is to cause stiffening rather than gnarling and the end result may be ankylosis of the spine or arthrofibrosis of the knee. Each of these criteria serve to distinguish it from rheumatoid arthritis. (Table 69-1).
Table 69-1 Contrasting Clinical Features of Rheumatoid Arthritis and Psoriatic Arthritis
| Rheumatoid Arthritis | Psoriatic Arthritis |
|---|---|
| Female predominance | No gender predominance |
| Peak onset at 45-55 yr | Variable age of onset |
| Sporadic | Familial occurrence |
| Symmetrical | Asymmetrical |
| Upper extremity | Lower extremity |
| Small joint | Large joint |
| Polyarticular | Oligoarticular |
| No axial disease | Axial disease |
| Synovitis | Enthesitis |
Radiographic Features
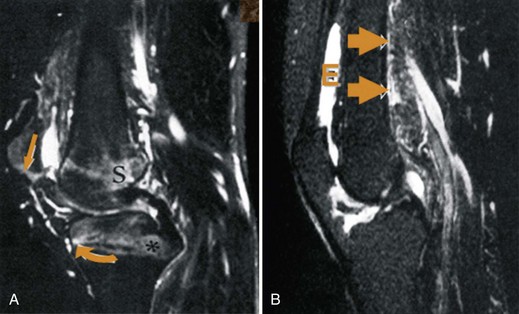
PsA may be distinguished from RA by its radiographic findings. These are summarized in Table 69-2. The earliest lesion of PsA is bone marrow edema, best demonstrated on T2 images. Figure 69-2 contrasts the magnetic resonance imaging (MRI) appearance of PsA with that of RA. As expected, the inflammation in PsA centers on the enthesis rather than the synovium as seen in RA.
Table 69-2 Radiographic Differences Between Rheumatoid Arthritis and Psoriatic Arthritis
| Rheumatoid Arthritis | Psoriatic Arthritis |
|---|---|
| Periarticular osteoporosis | Periarticular osteosclerosis |
| Small marginal erosions | Atypical,large erosions |
| No periostitis | Periostitis |
| MCP, PIP changes; no DIP changes | DIP common |
| Bone resorption | Proliferative changes |
| Spine changes limited to C1-2 | Sacroiliitis, spondylitis |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree