CHAPTER 14 Osteochondral Lesions of the Talar Dome
Cartilage Replacement Using Autologous Chondrocyte Implantation and Allografts
Osteochondral lesions of the talus (OLTs) are rare, representing only about 4% of all such lesions in the body.1 This lesion also has been called osteochondritis dissecans, transchondral fracture, talar dome fracture, and osteochondral defect. OLTs consist of a focal cartilage deficit with associated reactive bone edema.
Several staging systems have evolved since Berndt and Harty proposed the first system based on radiographic imaging of the talus in 1959 (Table 14-1).2 Loomer and colleagues3 reviewed computed tomographic (CT) data of 92 patients with OLTs and found a previously unclassified lesion—the radiolucent lesion—in 77% of the patients in their series. In 1999, Hepple and coworkers,4 using magnetic resonance imaging (MRI) added another characteristic to the original classification system—stage 5, subchondral cyst formation.
TABLE 14-1 Staging System Proposed by Berndt and Harty
| Stage | Description |
|---|---|
| Stage 1 | Compression of the border of the talus |
| Stage 2 | Incomplete detachment of fragment |
| Stage 3 | Complete detachment, no displacement |
| Stage 4 | Displaced fragment or loose body |
From Berndt AL, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959;41A:988-1020.
NORMAL AND PATHOLOGIC ANATOMY
The articular cartilage of the talus is inconsistent with the posteromedial corner, having a greater depth of cartilage than the anterolateral. This manifests in geographic mechanical properties and may influence the rate and type of articular injury.5–7
PATIENT EVALUATION
History and Physical Examination
A history of trauma is documented in more than 85% of patients.8–12 In most cases, the mechanism of injury is an inversion injury to the lateral ligamentous complex. Although the cause of nontraumatic OLTs is unknown, a primary ischemic event may be responsible. Nontraumatic OLTs can also be familial, multiple lesions can occur in the same patient, and identical medial talar lesions have occurred in identical twins.13
Diagnostic Imaging
Patients with an acute ankle injury with hemarthrosis or substantial tenderness should first undergo weight-bearing plain radiography (i.e., anteroposterior, lateral, and mortise views). Radiographs in various degrees of plantar flexion and dorsiflexion may help in diagnosing posteromedial and anterolateral lesions, respectively.14 Plain radiographs of the contralateral ankle should be obtained, because there is a 10% to 25% incidence of a contralateral lesion.15
MRI can identify occult injuries of the subchondral bone and cartilage that may not be detected with routine radiographs.16,17 Classic MRI findings include areas of low signal intensity on T1-weighted images, which suggests sclerosis of the bed of the talus and indicates a chronic lesion.18,19 T2-weighted images reveal a rim that represents instability of the osteochondral fragment.18,20 After treatment, MRI should reveal a reduction or disappearance of the low signal intensity on T1-weighted images and the rim on T2-weighted images.
TREATMENT
Indications and Contraindications
Surgical repair of OLTs is contraindicated when the risks outweigh the perceived benefits. Risks include active infection in the operative area, the likelihood of patient noncompliance, and patients who are medically unstable. Relative contraindications include degenerative changes of the ankle involving more than an isolated OLT. Studies have shown that a trial of conservative therapy does not adversely affect surgery performed after conservative therapy has failed.1,21
Treatment Options
Arthroscopy of the Ankle
Anterior Ankle Arthroscopy.
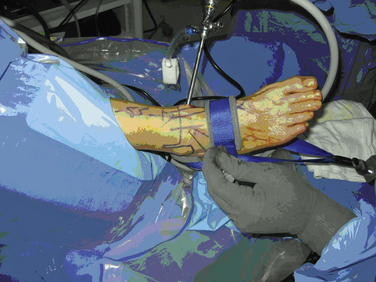
Distraction techniques facilitate the placement of the arthroscope and instruments into the tightly configured ankle joint (Fig. 14-1). Noninvasive techniques involving straps, harnesses, and outriggers are distraction methods used most commonly. These techniques minimize the risk of neurovascular injury and other complications.22
Posterior Ankle Arthroscopy.
Occasionally, posterior lesions are not accessible from the anterior ankle. In these cases, a posterior arthroscopic approach is favored. Through the posterior scope, 54% of the talar dome surface can be visualized and treated.23
Arthroscopic Débridement with Microfracture.
Arthroscopic treatment of OLTs involves three principles: removing loose bodies, securing the OLT to the talar dome (i.e., open reduction with internal fixation), and stimulating development of fibrocartilage. Open reduction with internal fixation is reserved for large, acute OLTs. More often, the lesion is débrided to a stable articular rim, and marrow stimulation techniques are used to create the healing cartilage.
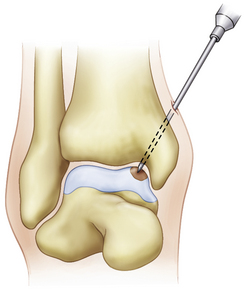
The microfracture technique for OLTs is based on the success of similar techniques in the knee (Fig. 14-2).24,25 Using awls, microfractures (i.e., perforations) are made approximately 3 to 4 mm apart in the subchondral bone while maintaining the integrity of the bone plate. The microfracture technique promotes new tissue formation by releasing substances such as mesenchymal stem cells, growth factors, and healing proteins.24 Ultimately, cartilage-like cells (i.e., fibrocartilage) form and fill the original defect.
Tol and associates26 reviewed 32 studies that reported the results of treatment for OTL. Nonoperative treatment had an average success rate of 45%, whereas the best success rate of 85% was achieved with excision, curettage, and drilling. Posteromedial lesions are difficult to access with this technique. The size of the lesion also plays a role in the success or failure of this procedure. In the meta-analysis by Tol and colleagues,26 the lesion size averaged 0.7 cm; currently, lesions larger than 1 cm are thought to have a less predictable outcome with microfracture.
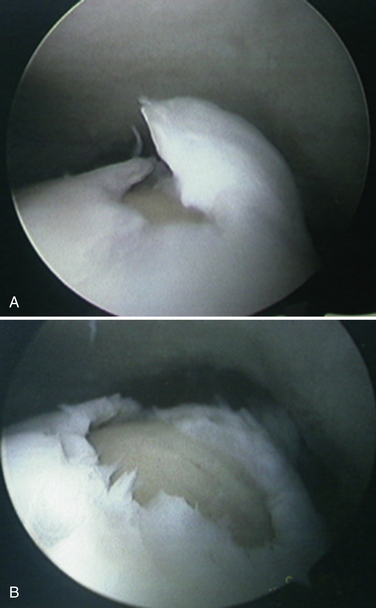
The limitation of microfracture is that fibrocartilage is created to fill the defect. This is predominantly type I cartilage, which lacks the organized structure of normal hyaline cartilage and therefore has inferior wear characteristics (Fig. 14-3).
We retrospectively reviewed the results of arthroscopy and microfracture in 189 patients; MRI was used to determine the size of the lesion.27 Good results were achieved in 132 patients with an average lesion size of 0.67 cm2; 22 patients with an average lesion size of 0.76 cm2 had fair results; and 36 patients with an average lesion size of 1.09 cm2 had poor results (Fig. 14-4).
Open Approaches to the Ankle: Malleolar Osteotomies
The tibiotalar articular surface can be accessed through arthrotomies and arthroscopically. For techniques in which an articular graft must be delivered to the articular defect, an open approach is often favored. Muir and colleagues28 studied nine cadavers to evaluate the accessibility of the talar dome by various approaches about the ankle. They used four arthrotomies and three osteotomies and characterized the percentage of the talar dome that could be accessed in a perpendicular fashion with respect to the articular surface. They found that without an osteotomy, up to 24% of the medial talar dome (average, 17%) and 25% of the lateral talar dome (average, 20%) could not be accessed. Osteotomies add an average of 22% exposure, although there remains a central 15% that is inaccessible in a perpendicular manner.28