CHAPTER 4 Diagnostic Arthroscopy for the Ankle and Subtalar Joints
The ankle is a highly constrained joint composed of complex, curved articular surfaces that are stabilized by ligaments with various degrees of laxity. These anatomic constraints make arthroscopy of the ankle joint more difficult than in larger joints such as the knee and shoulder. Early attempts to perform arthroscopy of the ankle joint were met with various degrees of success. In a 1931 cadaver study, Burman suggested that the ankle joint “… is not suitable for arthroscopy.”1
Arthroscopists in the 1980s began to apply modern techniques to instrumentation of the ankle and defined the basic portals with which to approach the joint.2–4 Since then, two technical advances have facilitated routine performance of ankle arthroscopy for diagnosis and surgical procedures. First, the development of high-quality, small-diameter arthroscopes has allowed instrumentation of the ankle with increased ability to visualize the entire joint while decreasing the likelihood of iatrogenic articular cartilage injury. Second, techniques have been developed for noninvasive joint distraction to facilitate instrument passage and decrease joint injury.5 Without distraction, it is often impossible to visualize the central and posterior compartments of the joint from the anterior portals. Early attempts to distract the joint used pins placed into the tibia and calcaneus that were connected to a distractor device similar to an external fixator. The use of these devices was associated with significant complications, including pin tract infection and neurovascular injury.6 Elimination of these complications while effectively distracting the joint with noninvasive strap distraction is a major advantage, and invasive ankle joint distraction is no longer recommended.
PATIENT POSITIONING
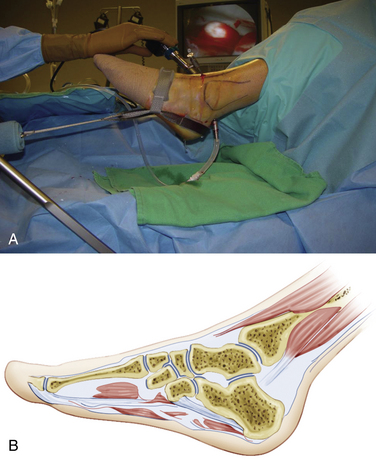
The patient is placed supine on the operating table with the hip and knee flexed and supported by a well-padded leg holder (Fig. 4-1). I prefer a leg holder with a long thigh segment and short knee segment to diffuse the distraction force over the wide area of the thigh rather than concentrating the force in the popliteal space and potentially causing obstruction to venous outflow. Sterile drapes are applied after skin preparation.
A sterile clamp is attached to the operating table side rail over the sheets, and a bar is fixed to the clamp. The noninvasive ankle distractor strap is placed around the hindfoot and midfoot and connected to the bar using a segment of sterile two-sided Velcro. This distraction setup allows the ankle and foot to rest in a plantigrade position while retaining the ability to move the ankle in dorsiflexion and plantar flexion intraoperatively (Fig. 4-2).
Invasive distraction is not required for standard ankle arthroscopy. It poses unnecessary risks to neurovascular structures, along with risks of infection and stress fracture.
PORTAL CREATION
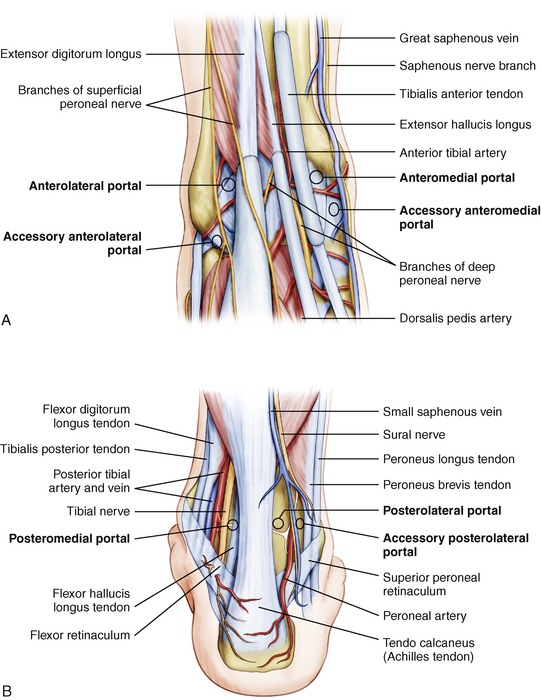
The three standard working portals for ankle arthroscopy are the anteromedial portal, the anterolateral portal, and the posterolateral portal (Fig. 4-3). The anterocentral portal was used in the early days of ankle arthroscopy because of the purported benefit of increased visualization in the central compartment. However, this portal placement poses significant risk of injury to the deep peroneal nerve and the dorsalis pedis artery. The use of small joint arthroscopes and noninvasive joint distraction obviates the use of this portal for ankle arthroscopy.
The first portal created should be the anteromedial portal. In most patients, there is an indentation in the anteromedial articular surface of the distal tibia, known as the notch of Harty, that facilitates passage of instruments across the ankle joint from medial to lateral aspects. The surgeon palpates the tibialis anterior tendon and inserts an 18-gauge needle into the joint immediately adjacent to the tendon’s medial border (Fig. 4-4). As the needle enters the joint, the surgeon notices the sound of air entering the joint, which also allows the ankle to be distracted more easily. Needle placement is adjusted proximally or distally until the position that allows easiest passage across the joint is identified as the optimal location for the portal. The cannula is introduced through this portal, and the 2.7-mm arthroscope is introduced into the joint.
With the arthroscope in the anteromedial portal, the posterolateral portal is created under direct visualization. The portal is located adjacent to the lateral border of the Achilles tendon and approximately 1 to 2 cm distal to the anterior portal so that an upwardly angled 18-gauge needle passes into the joint beneath the posterior syndesmotic ligament complex and accommodates the posterior curvature of the talar dome (Fig. 4-5). Another 2.7-mm cannula is placed and functions as a dedicated inflow cannula attached to an arthroscopic fluid pump.
PEARLS& PITFALLS