CHAPTER 17 Fusion for Degenerative Arthritis of the Ankle
Unlike hip and knee arthritis, primary ankle osteoarthritis is rare, and most degenerative ankle arthritis is post-traumatic in nature. Autopsy studies demonstrate that degenerative changes are about three times more prevalent in the knee than the ankle and that degenerative changes in both joints increase with increasing age.1,2 Radiographic studies that aim to quantify the prevalence of ankle osteoarthritis are of limited value because of the low correlation between the identification of osteophytes on plain films and the development of symptomatic osteoarthritis.3 Clinical studies suggest that knee and hip osteoarthritis is 8 to 10 times more common than ankle osteoarthritis.1,4
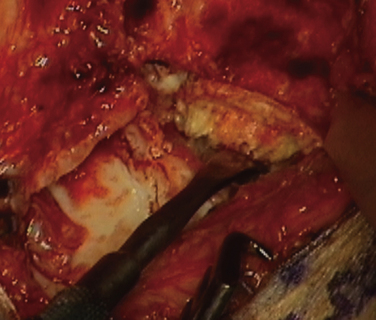
Because ankle arthritis is primarily post-traumatic, it affects a younger and more active patient population than hip and knee osteoarthritis. This fact demands a durable surgical option when nonoperative interventions have failed. The use of total ankle replacement is evolving, and new designs are being developed, but the gold standard for most cases of end-stage ankle arthritis has been open ankle arthrodesis. During the past 2 decades, arthroscopic ankle arthrodesis has become a viable alternative to the open procedure and has shown encouraging results.5–8 Proposed advantages of arthroscopic techniques are less postoperative pain and morbidity, decreased blood loss, and shorter hospital stay. One important advantage of arthroscopic ankle arthrodesis is that it can be performed in patients with a poor soft tissue envelope (Fig. 17-1).
ANATOMY AND PATHOGENESIS
The ankle is relatively resistant to primary degenerative osteoarthritis, possibly because of the properties of ankle cartilage, including relatively better retention of tensile fracture stress and tensile stiffness with age, as described by Kempson and colleagues.9 The cartilage in the ankle is metabolically different from that in the knee. Ankle cartilage appears to be less affected by the catabolic cytokine interleukin 1 (IL-1) and deleterious collagenases that are produced in response to IL-1.10
Secondary osteoarthritis of the ankle can develop after fracture or ligamentous injury. Rotational ankle fractures and ligamentous injury with recurrent instability are the most common causes.11–15 In Saltzman’s practice during 13 years, 445 (70%) of 639 patients with Kellgren-Lawrence grade 3 or 4 ankle arthritis were post-traumatic cases, and only 46 patients (7.2%) had primary oseteoarthritis.13 Other recorded causes in this study of ankle arthritis included neuropathic disease (e.g., Charcot neuroarthropathy), inflammatory arthropathies (e.g., rheumatoid arthritis), crystalline arthropathies (e.g., pseudogout), osteochondritis, osseous necrosis, and postinfectious arthropathy.
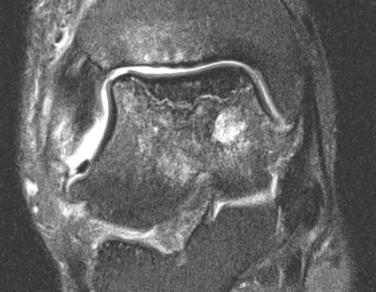
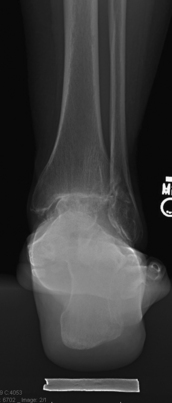
The relative resistance of the ankle joint to primary osteoarthritis is likely a combination of its congruency, which results in inherent stability and restrained motion; unique tensile properties; and distinctive metabolic characteristics. Unfortunately, the ankle is quite susceptible to post-traumatic arthritis, and this may be related to its thinner and stiffer articular cartilage not being able to accommodate articular step-offs or the stresses of improperly constrained motion. Step-offs lead to increased local contact stresses that the thin cartilage of the ankle may not be able to accommodate as well as the thicker cartilage in the hip and knee.16,17 These increased localized contact stresses likely contribute to the degeneration of articular cartilage that is seen after trauma. Other disease processes, such as Charcot arthropathy and osteochondritis, with large osteochondral defects can lead to step-offs or incongruity in the articular surface and result in increased contact stresses (Figs. 17-2 and 17-3).
PATIENT EVALUATION
History and Physical Examination
The first step in evaluating the patient with ankle pain is to obtain a proper history, particularly any history of trauma. One major ankle sprain can result in a significant injury to ankle joint cartilage or persistent instability, with the eventual development of degenerative changes.13 Inquiring about other joint pain is important because multiple joint involvement may indicate systemic causes, such as inflammatory arthropathy. Ankle arthritis is not usually the first manifestation of a systemic disease process. Ascertaining a diabetic history is important, because diabetes is a risk factor for Charcot neuroarthropathy and related to perioperative morbidity in those with end-stage organ disease.
The seated examination includes evaluation of range of motion in the ankle, hindfoot, midfoot, and forefoot. Ankle stability should be assessed by drawer testing, with the foot in plantar flexion and neutral position, which investigates the competence of the anterior talofibular ligament and calcaneofibular ligament, respectively. Talar tilt should be assessed. Foot alignment is important because deformity in the foot may cause secondary ankle disease. For example, pes planus with medial column instability may be associated with secondary ankle valgus and eventual degenerative change. Conversely, realignment of a deformed ankle can alter the foot position and adversely or positively affect function of other joints, particularly the subtalar joint. If compensatory foot deformities are identified on examination, their passive, manual correctability has to be assessed.
Diagnostic Imaging
Radiographs should be done weight bearing if possible. The four radiographic views we use in our clinic to evaluate ankle pain include the anteroposterior, lateral, mortise, and hindfoot alignment views. Radiographs of the degenerative ankle can show joint space narrowing, osteophyte formation, subchondral sclerosis, and subchondral cysts. The hindfoot alignment view is important in the evaluation hindfoot varus or valgus and ankle deformity in the coronal plane.18 It is taken with the patient standing on a platform facing a collector that angles away from the platform at 20 degrees. The x-ray tube is posterior to the ankle, with the beam perpendicular to the plane of the film at the level of the ankle. The source-to-collector distance is 40 inches. On average, the most inferior aspect of the calcaneus lies just medial to the longitudinal midaxis of the tibia (Fig. 17-4). Magnetic resonance imaging (MRI) has limited usefulness unless the examiner suspects an osteochondral lesion of the talus, osseous necrosis, or ligamentous abnormality that will alter patient care. In such cases, MR arthrography may be advantageous. Computed tomography (CT) is the better choice for three-dimensional bony imaging, and it allows visualization near hardware, unlike MRI. Noninvasive joint distraction plus air-contrast arthrography enhances visualization of the ankle’s articular features.19
Selective fluoroscopically guided injections can be helpful in diagnosing patients who have clinical or radiographic findings that suggest more than one source of pain. It is reasonable to expect 75% pain relief in an area that is injected.20 It is important to identify the patients’ ankle pain as global (i.e., affecting most of the joint) or focal (i.e., affecting a specific region), because this distinction may guide the treatment options. It is essential to identify patients with coexisting subtalar pain, because that population needs to be counseled more intensely about the risks of residual pain and progression of adjacent joint arthritis.
TREATMENT
Nonoperative and operative treatments can help reduce symptoms and improve the function of painful ankle arthritis. There are no well-designed retrospective or prospective clinical trials reporting on nonoperative treatment of diffuse ankle arthritis. Our experience is that nonsteroidal anti-inflammatory drugs have variable efficacy in addressing the pain of ankle arthritis. The judicious use of corticosteroid injections may provide temporary relief and be beneficial in acute exacerbations in someone who has tolerable steady-state pain. Clinical trials suggest that hyaluronate-based injectables may diminish ankle pain and improve function in patients with ankle osteoarthritis, and additional trials exploring this treatment modality are being conducted.21,22
Nonoperative interventions primarily focus on mechanical unloading and immobilization. Devices that address this goal include the cane, ankle foot orthoses (AFOs), and the leather ankle lacer with an embedded polypropylene shell.23 To fully unload the ankle joint requires a rigid linkage between the acceptance of force on the sole of the foot and the leg above the ankle. The prototypic device, a weight-bearing patellar brace (PTB), is poorly tolerated because load transfer irritates the soft tissues in front of the knee. Adding a rocker-bottom sole to a shoe or the use of a solid ankle-cushioned heel (SACH) may also provide relief by reducing ankle excursion with gait.
Operative intervention should be considered only after failure of nonoperative treatment methods. The surgeon should identify the cause of the patient’s problem and to what extent ligamentous instability, malalignment, or other foot deformity contributes to the perceived pain from ankle arthritis. When planning surgical interventions, recreating normal foot alignment can encourage improved foot function, regardless of the chosen surgical technique. Surgical options for end-stage degenerative ankle arthritis include osteotomies about the ankle, débridement, distraction, ankle arthroplasty, and ankle arthrodesis. Ankle arthrodesis can be performed in a variety of ways, including open, mini-open, and arthroscopic techniques.
In terms of arthroscopic ankle arthrodesis, the indications remain the same, with the exception of a failed total ankle replacement. Well-aligned ankles and those that are easily realigned are excellent candidates for arthroscopic fusion. Patients with soft tissue compromise (e.g., those with prior trauma, burn victims, patients with skin grafts) or vasculopathy are strongly considered for an arthroscopic approach. In the past, it was thought that ankle varus or valgus greater than 5 degrees was an absolute contraindication to arthroscopic arthrodesis. However, later reports suggested that substantial ankle varus or valgus is a relative contraindication rather than an absolute one.24,25 The investigators consider any ankle that can be re-aligned properly after arthroscopic débridement appropriate but acknowledge that patients should be counseled that conversion to an open approach is prudent if an extensive capsulotomy is required to achieve correct alignment. Additional contraindications for the arthroscopic procedure are significant focal bone loss and deformity and extremely rigid ankles. In general, the desired position of the arthrodesis is neutral dorsiflexion, 5 degrees of ankle valgus, equal or slightly greater external rotation compared with the contralateral leg, and placement of the anterior aspect of the talar dome at the level of the anterior aspect of the tibia.
Arthroscopic ankle arthrodesis was first developed in the mid-1980s. Myerson and Quill reported the first comparative series, with 17 arthroscopic procedures compared with 16 open procedures done with a medial malleolar osteotomy.7 They found an average fusion time of 8.7 weeks in the arthroscopic group and 14.5 weeks in the open group, with similar fusion rates for both groups. Their criteria for clinical union included an absence of tibiotalar motion, crepitus, or pain with ambulation or on examination. Radiographic union was defined as the appearance of osseous trabeculae across the tibiotalar arthrodesis site and incorporation of bone graft into the fusion mass when bone graft was used.
One of the first long-term series was published in 1996 by Glick and colleagues.6 They reported 34 cases with an average follow-up of 8 years. Fusion rates were 97%, and good or excellent results were reported for 86% of patients. Three ankles in this series were rated poor because of subtalar pain and a nonunion, and a malunion accounted for the other poor results.
O’Brien and colleagues added support to arthroscopic arthrodesis by showing comparable fusion rates between 19 arthroscopically treated patients and 17 patients undergoing open arthrodesis using flat cuts.8 The arthroscopic group had decreased operative times, decreased tourniquet times, less blood loss, and decreased hospital stays.