68
Osteoarthritis: Carpometacarpal Joint (Ligament Reconstruction with Tendon Interposition)
Vincent Ruggiero and Andrew K. Palmer
History and Clinical Presentation
A 55-year-old right hand dominant woman presents with the complaint of pain of 3 years’ duration in the right thumb. The pain has progressed to the point where it now interferes with her activities of daily living in her house and garden. She complains of weakness of both pinch and grasp. She denies any numbness or tingling in her fingertips or loss of motion of the hand or wrist.
Physical Examination
There is tenderness and swelling about the basal joint of the thumb. Axial compression causes pain and palpable grating at the basal joint of the thumb. The thumb carpometacarpal (CMC) joint is unstable to stress testing. Her thumb metacarpal is adducted and the metacarpophalangeal (MP) joint of the thumb hyperextends 15 degrees on stress testing. Her pinch and grip strengths are decreased by one-half of her nondominant side. She has negative Phalen’s, Tinel’s, and Finkelstein’s tests.
Diagnostic Studies
Anteroposterior (AP), lateral, and stress views of the thumb reveal grade 2 osteoarthritic changes of the metacarpal-trapezial joint and scaphotrapezial joint with subchondral sclerosis, cystic change, and surrounding osteophyte formation (Fig. 68–1). A stress view, which is obtained with the thumb and index at maximal pinch, reveals mild radial subluxation of the first metacarpal-trapezial joint (Fig. 68–2).
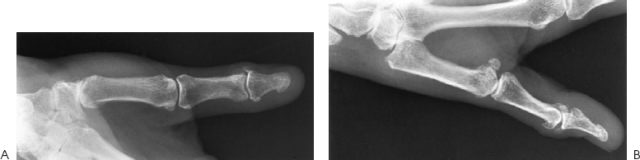
Figure 68–1. (A) Anteroposterior (AP) view of the carpometacarpal (CMC) joint with both trapeziometacarpal and scaphotrapezial degenerative changes. (B) Lateral view with same findings.
PEARLS
- Be sure to dissect the FCR free to its insertion on the index metacarpal to ensure the best possible ligament reconstruction.
- When securing the ligament reconstruction, be sure to pull traction on the thumb metacarpal and obtain maximal adduction of the metacarpal base. When the base is maximally adducted the thumb ray will be abducted.
- If the bony bridge between drill holes fractures, make a second drill hole dorsoradial.
PITFALLS
- When removing the trapezium, be careful not to damage the FCR, which is directly below.
- Not addressing the associated MP hyperextension will lead to instability with pinch and can contribute to failure of the CMC arthroplasty.

Figure 68–2. Maximum pinch view demonstrating mild subluxation of the CMC joint with degenerative change (arrow).
Differential Diagnosis
Carpometacarpal arthritis
Carpal tunnel syndrome
De Quervain’s tendinitis
Flexor carpi radialis tendinitis
Trigger thumb
Diagnosis
Carpalmetacarpal Arthritis: Pan Trapezial
Note the scaphotrapezial joint has arthritic changes also.
Carpometacarpal arthritis is a common condition that has a predilection for middle-aged women. This may be a sequela of idiopathic hypermobility of the CMC joint. It can also be associated with trauma or inflammatory diseases. Activities that require strength and/or mobility of the thumb are difficult to perform. Examples are key pinch and opening a jar.
Eaton has classified CMC arthritis into four stages. Stage I is characterized by no joint degeneration and articular contours that are normal. There may actually be widening of the joint space secondary to an effusion. Stage II is characterized by slight narrowing of the trapeziometacarpal joint on radiographs. If any joint debris is present, it is less than 2 mm in size. Stage III is characterized by significant trapeziometacarpal joint destruction radiographically. Sclerotic and cystic changes are noted in the bone. Stage IV is characterized by scaphotrapezial degenerative arthritis in addition to the changes seen in stage III.
Surgical Management
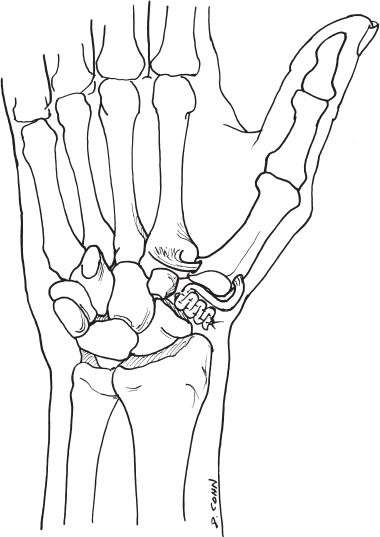
Ligament reconstruction with tendon interposition (LRTI) is our preferred treatment for the late stages of CMC arthritis. The reconstruction of the volar beak ligament prevents thumb ray shortening and instability. The arthroplasty helps to prevent collapse of the thumb. We usually perform a complete trapezial resection, as most of our patients have some degree of scaphotrapezial arthritis that may not be evident on radiographs.
An incision is made bordering the thenar eminence over the first metacarpal border from about 2 cm distal to the CMC joint curving toward the flexor carpi radilis (FCR) tendon at the wrist. The subcutaneous tissue is bluntly dissected, taking care to preserve the branches of the superficial radial nerve. The abductor pollicis longus (APL) and the extensor pollicis brevis (EPB) are identified and protected. The radial artery is identified in the proximal aspect of the wound overlying the trapezium. It is mobilized proximally and protected. Manual traction is applied to the thumb to identify the CMC joint. The capsule is split from the trapezialmetacarpal joint to the scaphotrapezial joint longitudinally. The capsule is then subperiosteally elevated off the trapezium. Using a rongeur, the trapezium is morcellized and removed. This can also be done with the use of an osteotome. Care should be taken to protect the FCR tendon that lies in the depths of the wound.
The FCR tendon is then harvested for ligament reconstruction and interposition arthroplasty. Starting distally, 3 cm above the wrist flexion crease, the FCR tendon is identified by palpation. An incision is made over the tendon transversely, the tendon isolated, a hemostat placed beneath it, and traction applied to the tendon. The tendon is then palpated 8 to 10 cm proximal to the first incision and a second transverse incision is made. The FCR tendon is identified, a hemostat placed beneath it, and the tendon divided. At this juncture, the tendon is sharply separated from the muscle belly distally beneath the skin bridge with scissors. The tendon is then with drawn into the first incision and all FCR muscle belly is removed with sharp dissection. Traction is then applied to the tendon with the wrist flexed, and, using scissors, the tendon is freed from its surrounding adhesions beneath the skin between the first incision and the wrist flexion crease. A Ragnell is then placed beneath the FCR tendon in the trapezial resection wound and the tendon delivered into the wound. A whip-stitch is placed in the tendon for ease of passage through the subsequent drill hole in the first metacarpal.
The thumb metacarpal is prepared for ligament reconstruction by first drilling a ⅛-inch hole in the dorsal aspect of the metacarpal base 1 cm from the articular cartilage. A similar hole is then drilled through the articular cartilage at the metacarpal base. The two holes are enlarged with progressive drill bits to an 11/64;-inch hole. Curettes are used to smooth out the tunnel that has been created through the first metacarpal. Care should be taken not to fracture the bony bridge separating the two holes of the tunnel.
Prior to passage of the tendon through the first metacarpal, scissors are used to gently dissect the tendon free to its insertion on the base of the second metacarpal. The suture previously placed in the end of the tendon is then passed through the tunnel in the first metacarpal from the base of the metacarpal out distally and radially. Moistening the tendon prior to attempting to pass may allow easier passage.
The tendon is then pulled snugly and the first metacarpal is advanced distally. A 2–0 PDS suture is placed through the radial cortex of the first metacarpal and the FCR tendon, holding the metacarpal base in maximum adduction and distraction.