Specifically, the synovial membrane may have a mild to moderate inflammatory reaction and may contain fragments of articular cartilage (9). Within the synovial fluid, pathological changes include significant alteration in synovial fluid HA, including a decrease in the concentration of normal molecular weight hyaluronate and the production of abnormal hyaluronate. The resultant decreased hyaluronate concentration is a result of both defective hyaluronate production and increased hyaluronate breakdown. In addition, there is increased water content and an increased concentration of inflammatory mediators (10). These pathological changes result in defective synovial fluid viscosity, elasticity, barrier exclusion and shielding. Exposure of synovial nociceptors perhaps explains in part the pain associated with the osteoarthritic joint.
Various factors including abnormalities that are unrelated to obesity; adiposity lying below the hip joint, which does not contribute to loading; and distribution of body weight load more broadly may be an explanation of less clear relationship between obesity and hip OA (16).
the joint environment. The subchondral bone contains not only bone marrow and trabecular bone but also end arteries and veins. The subchondral bone has marked porosity, with vessels penetrating the calcified cartilage zone. These help provide nutrients to the cartilage and facilitate the removal of metabolic waste products. The perfusion of these vessels accounts for more than 50% of the glucose, oxygen, and water requirements of the cartilage (44). The underlying bone also undergoes turnover as per Wolff’s law that states that the bone remodels in response to externally applied forces. Thus, loads applied to the joint also help the subchondral bone to remain metabolically active.
TABLE 31.1 Components of Normal Synovial Joints | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 31.2 Nonpharmacologic Guidelines for Hip and Knee OA | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
take control over the debilitating aspects of the disease, this volunteer-driven organization supplemented by dedicated staff to provide professional expertise and support for volunteer efforts helps individuals with arthritis improve quality of life through its many community-based, educational programs and activities. Outreach is provided through telephone and e-mail information services as well as the foundation’s internet site, www.arthritis.org, which serves as an outstanding resource for online information and support. Professional education directives also benefit health care providers to better diagnose and treat patients with arthritis. Publications, for both professional and consumer groups, continue to provide accurate and sound health information to record numbers.
performance of slow, continuous movements and postures. These techniques are thought to integrate the mind and the body resulting in a harmonious inner and outer self. Known benefits include increasing flexibility, muscle strength, fitness, balance, and cardiovascular (CV) health. The Sun Style of Tai Chi is especially suited for persons living with arthritis. This style utilizes forward or backward stepping motions, which is believed to improve mobility. When one foot moves forward or backward, the other foot follows. The higher stance places less stress on lower extremity joints. The coordinated breathing tied to motion promotes symptom relief and relaxation. Thus, the target audience for the Arthritis Foundation Tai Chi program is individuals with arthritis or related conditions characterized by diffuse muscle pain, decreased muscle strength, and fatigue. Preliminary outcome data suggest that participation results in improved lower extremity strength, balance, and reach.
Recently, the uses of patellofemoral taping techniques have been applied to relieve knee pain and improve reported physical function. While the taping group reported significantly less pain and improved function than those with no tape, the placebo tape group also reported benefit (86). Energy conservation techniques may help in minimizing unnecessary activities and joint stressors, so that the OA patient will be able to use his or her sometimes limited abilities to gain the most functional independence possible.
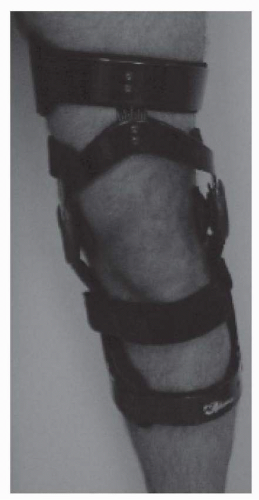
pain relief includes two main studies. Smith et al. described the emphasis of their studies as follows: “It was often possible during weight bearing for the physician to control instability of the knee by applying forces with his own hands, and in so doing relieve the associated pain. This relief can occur even though the disease is still present, a fact emphasizing the role of mechanical stress in pain production. If pain can be reduced by the proper application of forces manually, it may also be possible to relieve it with a properly designed brace” (93). In 1975, the Canadian Arthritis Research Symposium—University of British Columbia knee orthosis (CARS UBC), as described by Cousins and Foort, was designed specifically for the treatment of knee OA (94). The brace was comprised of plastic thigh and calf shells, utilized universal hinges and a telescoping tube assembly, and required a waistband for suspension.
Patients must adapt to the wedge via changes in muscle activity and posture, ultimately modifying their standing and walking mechanics. In addition to their effects on knee pain and forces acting at the knee, other investigators have examined the effects of lateral wedged insoles on knee kinetics. In this study, three-dimensional analysis was performed on 17 subjects with and without them wearing a 5-degree lateral wedged insole. They found no significant differences in temporal and spatial parameters; joint angles at the hip, knee, and ankle; or kinetics at the hip and ankle. The external varus moment and estimated medial compartment load at the knee were reduced significantly (102). One can interpret the results to indicate that lateral wedged insoles are a potential effective component of a conservative treatment regimen for patients with mild medial compartment OA.
is very common and especially affects the first CMC joint, the proximal interphalangeal (PIP) joints, and the DIP joints.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree