22 Ossification of the posterior longitudinal ligament (OPLL) is a condition in which bone forms within the posterior longitudinal ligament (PLL), which lies posterior to the vertebral bodies within the spinal canal. The PLL is ~ 1 to 2 mm thick, consisting of a deep and a superficial layer. It traverses the posterior surface of the vertebral bodies from the cervical spine to the sacrum. As it transverses the vertebral column, it has strong attachments to the vertebral bodies and intervertebral disks. It is at these sites of “traction” that the PLL will first hypertrophy and, in many cases, partially or completely ossify. This growth of the PLL with bone and ligament may cause compression of the spinal cord. OPLL is more prevalent in the Asian population, with rates ranging from 1.9% to 4.3% in the Japanese population. It presents more often in the fifth and sixth decades of life, with a male-to-female preponderance of 3.5 to 1. Patients with OPLL are at higher risk for spinal cord injury following trauma due to the stiffness in their neck and pre-existing pressure on the spinal cord. The exact etiology of OPLL is currently unknown, although there are multiple theories. It has been postulated that there may be a genetic factor, given that the siblings of patients with OPLL who share a greater number of human leukocyte antigen (HLA) haplotypes are at an increased risk for developing OPLL. In addition, it has been observed that excessive weight gain between the ages of 10 and 40 is also an independent risk factor for OPLL, and there is an association between OPLL and diabetes mellitus. Other studies have suggested that elevated blood levels of markers for bone formation may indicate patients pre-disposed to forming OPLL. Finally, associations between OPLL and other bone-forming diseases, such as diffuse idiopathic skeletal hyperostosis (DISH), have been suggested. There are four different patterns of OPLL that can be identified. The first pattern is continuous, in which the ossification proceeds in a flowing, uninterrupted fashion along the posterior border of the vertebral border of the vertebral body, spanning the retrovertebral space. The second pattern is noncontinous ossification, which appears only adjacent to each vertebral body and is often referred to as segmental. The third type is localized, where only one area of ossification is identified adjacent to a single vertebra. The forth type is “mixed” and contains features of each of these aforementioned three types. OPLL of the cervical spine may present with a spectrum of findings. Many patients are asymptomatic and are unaware that they have OPLL. The natural history of the disease in these individuals is unknown; however, it is known that even patients who are asymptomatic are at higher risk of spinal cord injury following a trauma. When OPLL causes symptoms, the initial presentation can be that of neck pain, arm pain, and/or weakness. Patients may also report symptoms of cervical myelopathy, including loss of dexterity or clumsiness of the hands and difficulty walking. With increasing ossification of the PLL, patients may begin to notice a decrease in range of motion of the neck. Among the majority of these patients who present with myelopathy, the severity of the symptoms can be graded using the Japanese Orthopedic Association (JOA) scoring system. A detailed history obtained from the patient at the time of initial presentation should clarify the spectrum and duration of symptoms. Key complaints include myelopathic symptoms, such as difficulties with dexterity and manipulating small objects, worsening handwriting, problems with balance and gait, and alterations in bowel/bladder function. In addition, radicular patterns of sensory loss or motor weakness may be identified. A careful physical exam should elucidate any signs of myelopathy as well, such as disturbance in gait, loss of manual dexterity, and the presence of hyperreflexia, especially in the lower extremities. Abnormal reflexes may also be present, such as Hoffmann sign, Babinski reflex, reversed radial reflex, finger-escape sign, or sustained ankle clonus. Although these findings are classically associated with spinal cord compression, some patients with extensive cord compression due to OPLL nevertheless exhibit few of these findings. This may be due to the very slow growth of OPLL over time. The presence of OPLL can be confirmed with radiographic evaluation. Plain radiographs are commonly used in the initial assessment. The four different patterns of OPLL (continuous, segmental, localized, and mixed) can be identified on lateral radiographs. Narrowing of the spinal canal can be seen on radiographs in areas where the ossification is significant. It can be seen anywhere from the levels of C2 to C6. OPLL can also be seen at the thoracic and lumbar levels, most commonly at the levels T4 to T7 and L1–L2. Below the level of the conus medullaris, OPLL is rarely clinically significant. Computed tomography (CT) is the most useful radiographic modality in evaluating OPLL. It is particularly effective in defining the extent of the ossification and the resulting stenosis. Myelography is often used as an adjunct with CT scans to provide better definition of the neural elements and the compressive effects placed on these structures. However, myelography is an invasive procedure and carries with it risks of infection, dye allergy, and spinal headache if a cerebrospinal fluid (CSF) leak occurs. Magnetic resonance imaging (MRI) is able to define the neural elements while remaining noninvasive and precluding the need for patient radiation. MRI is also able to identify subtle parenchymal changes within the spinal cord and nerve roots. However, the typical lesions in OPLL are not well defined on T1- or T2-weighted scans, thus making MRI a poor test for diagnosing OPLL. Nonoperative management of OPLL is appropriate for those patients with neither symptoms nor physical findings of cervical myelopathy. These patients, whose only complaint is usually neck pain, may be helped with a course of physical therapy and anti-inflammatory medications. In addition, a judicious trial of cervical traction may benefit patients who present with radicular complaints. However, traction is not appropriate for patients with progressive myeloradiculopathy. Operative treatment is generally recommended for patients with any degree of significant myelopathy or radicular symptoms unresponsive to nonoperative measures. These patients usually have a JOA score of 12 or lower (maximum score of 17). The fundamental goal may be best achieved through an anterior, posterior, or combined decompressive procedure. Although most patients with myelopathy are safely decompressed via an anterior approach, anterior decompressive procedures in the presence of OPLL have an additional high risk of dural injury due to adherence of the OPLL to the dura anteriorly. As a result, many prefer a posterior decompression in patients with severe OPLL, especially when it occurs in a continuous fashion. Posterior approaches provide an indirect decompression of the spinal cord via cervical laminectomy, which is usually performed in conjunction with a fusion procedure, or laminoplasty. Cervical laminectomy involves complete removal of the cervical lamina across the involved segments. Laminoplasty entails enlargement of the spinal canal by hinging the lamina open on one side and securing it in an open position. Houten and Cooper showed in their retrospective review that cervical laminectomy with fusion not only halted the progression of disease but also showed significant improvement in JOA scores in 97% of patients. Excellent recovery rates have also been reported for laminoplasty. Laminoplasty has been shown in at least one comparative study to be superior to laminectomy and fusion, although that study was not specific to patients with OPLL. However, Hirabayashi et al. have shown laminoplasty to be at least as effective as laminectomy in treating OPLL. Cervical kyphosis precludes the use of posterior surgery because the spinal cord is not able to shift away from the anterior compressive lesions. Decompressive surgical treatment of cervical spinal cord compromise, whether performed anteriorly or posteriorly, carries inherent risk present in all surgery, such as infection, bleeding, deep vein thrombosis/pulmonary embolism, and complications from anesthesia. Specific risks with cervical surgery may be damage to nearby anatomic structures, such as the trachea, esophagus, and great vessels within the neck. Anterior, posterior, or circumferential decompressive procedures performed on or around the spinal cord in particular carry specific risks, such as paralysis, CSF leak, nerve damage leading to paresthesia or motor deficits, continuation of symptoms, axial pain, and reduced neck range of motion. Hilibrand et al. demonstrated that patients with OPLL have a significantly higher risk of neurophysiologic changes and possible spinal cord injury than other patients undergoing cervical spine decompressive procedures. Intraoperative neurophysiologic monitoring may allow early recognition of an impending neurologic injury. Early recognition of these insults may allow early institution of intraoperative maneuvers, which may curtail or reverse evolving spinal cord injuries. A complication unique to patients with long-standing cord compression due to OPLL and severe spondylosis is the presence of thinning or complete erosion/absence of the dura. This absence of dura is usually recognized after the ossified longitudinal ligament has been removed. It is often discrete and well demarcated, with the spinal cord and nerve roots being clearly visible through the remaining arachnoid layer. This can ultimately result in CSF leakage or a CSF fistula. The limited exposure often precludes a direct repair and requires an alternative technique, such as the use of sealants (such as fibrin glue), fascial grafts, or even subarachnoid drains. Chikuda H, Seichi A, Takeshita K, et al. Acute cervical spinal cord injury complicated by preexisting ossification of the posterior longitudinal ligament: a multicenter study. Spine 2011; 36(18):1453–1458 PubMed The authors retrospectively reviewed 453 patients with spinal cord injury and found OPLL in 106 (23%) of the patients. Of the injuries in patients with OPLL, 94 out of 106 occurred without bony injury. Only 25% of patients were aware of the diagnosis of OPLL prior to the injury. Most injuries were incomplete. Patients with gait dysfunction prior to the injury did better with surgical treatment. The study was conducted in Japan, which has a higher incidence of OPLL. Epstein NE. Circumferential cervical surgery for ossification of the posterior longitudinal ligament: a multianalytic outcome study. Spine 2004;29(12):1340–1345 PubMed This study reports the results for combined anterior and posterior procedures. It demonstrates that patients show the greatest improvements 1 year following surgery. Epstein NE. Identification of ossification of the posterior longitudinal ligament extending through the dura on preoperative computed tomographic examinations of the cervical spine. Spine 2001;26(2):182–186 PubMed This article evaluates the ability of CT to predict involvement of dura in the ossified lesion. Heller JG, Edwards CC II, Murakami H, Rodts GE. Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: an independent matched cohort analysis. Spine 2001; 26(12):1330–1336 PubMed This study compares two posterior procedures, laminectomy and laminoplasty, and shows that laminoplasty has both higher recovery rates and lower complication rates. Hilibrand AS, Schwartz DM, Sethuraman V, Vaccaro AR, Albert TJ. Comparison of transcranial electric motor and somatosensory evoked potential monitoring during cervical spine surgery. J Bone Joint Surg Am 2004;86-A (6):1248–1253 PubMed The authors of this study showed that transcranial electric motor evoked potential appeared to be a better modality than conventional somatosensory evoked potential, for monitoring patients during spinal surgery, especially those patients with OPLL. Hirabayashi K, Toyama Y, Chiba K. Expansive laminoplasty for myelopathy in ossification of the longitudinal ligament. Clin Orthop Relat Res 1999;359(359):35–48 PubMed This study compares laminoplasty to laminectomy and shows that similar success is seen with either procedure, and although an advantage of laminoplasty has been theorized, it has not yet been shown. Houten JK, Cooper PR. Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment, spinal cord compression, and neurological outcome. Neurosurgery 2003;52(5): 1081–1087, discussion 1087–1088 PubMed This study shows that laminectomy has a high rate of success while having lower complication rates than anterior surgery. Japanese Orthopedic Association. Scoring system for cervical myelopathy. J Orthop Sci 1994; 68:490–503 This article by the JOA reports a method with which to score cervical myelopathy, thus enabling objective comparison between cases and studies. Kobashi G, Washio M, Okamoto K, et al.; Japan Collaborative Epidemiological Study Group for Evaluation of Ossification of the Posterior Longitudinal Ligament of the Spine Risk. High body mass index after age 20 and diabetes mellitus are independent risk factors for ossification of the posterior longitudinal ligament of the spine in Japanese subjects: a case-control study in multiple hospitals. Spine 2004;29(9):1006–1010 PubMed This study demonstrates a link between OPLL and weight gain and diabetes mellitus, and suggests that these may be risk factors for the disease. Li H, Dai LY. A systematic review of complications in cervical spine surgery for ossification of the posterior longitudinal ligament. Spine J 2011;11(11):1049–1057 PubMed The authors performed a meta-analysis that included 27 studies with 1,558 patients. They found that the rate of complications following surgery was 21.8%, including an 8.3% risk of neurologic injury. The overall rate of complication did not vary with regard to approach (anterior vs. posterior); however, C5 palsy was more common with a posterior approach, and CSF leak, hoarseness, dysphagia, implant complications, and dyspnea were more common with anterior surgery. Matsunaga S, Yamaguchi M, Hayashi K, Sakou T. Genetic analysis of ossification of the posterior longitudinal ligament. Spine 1999;24(10):937–938, discussion 939 PubMed This study shows that OPLL has a definite genetic link. Onishi E, Sakamoto A, Murata S, Matsushita M. Risk factors for acute cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Spine 2011 Aug 18. [Epub ahead of print] The authors reviewed patients with OPLL and spinal cord injury, OPLL and myelopathy, and normal controls to identify risk factors for spinal cord injury in patients with OPLL. They identified advanced age, mixed/segmental OPLL, and ossification of the anterior longitudinal ligament as risk factors for spinal cord injury. Spinal stenosis was not an essential risk factor. Smith MD, Bolesta MJ, Leventhal M, Bohlman HH. Postoperative cerebrospinal-fluid fistula associated with erosion of the dura. Findings after anterior resection of ossification of the posterior longitudinal ligament in the cervical spine. J Bone Joint Surg Am 1992;74(2):270–277 PubMed The authors of this study concluded that given the higher risk of dural tears with anterior surgery for OPLL, the surgical plan should always include preparation for a dural tear. Sugimori K, Kawaguchi Y, Ohmori K, Kanamori M, Ishihara H, Kimura T. Significance of bone formation markers in patients with ossification of the posterior longitudinal ligament of the spine. Spine 2003;28(4):378–379 PubMed This study shows that certain markers may indicate the presence of OPLL and that a hyperostotic state exists in OPLL patients. Wu JC, Chen YC, Liu L, et al. Conservatively treated ossification of posterior longitudinal ligament increases risk of spinal cord injury: A nationwide cohort study. J Neurotrauma. 2011 Oct 12. [Epub ahead of print] The authors compared 265 patients with conservatively treated OPLL and an age-matched cohort of 5,339 patients with no OPLL. They found statistically higher rates of spinal cord injury among the OPLL cohort (4.81 vs. 0.18 per 1000 person-years), resulting in a 32-times increased risk of spinal cord injury. CT, computed tomography; MRI, magnetic resonance imaging; NEXUS, National Emergency X-Radiography Utilization Study; NSAIDs, nonsteroidal anti-inflammatory drugs; PT, physical therapy
Ossification of the Posterior Longitudinal Ligament
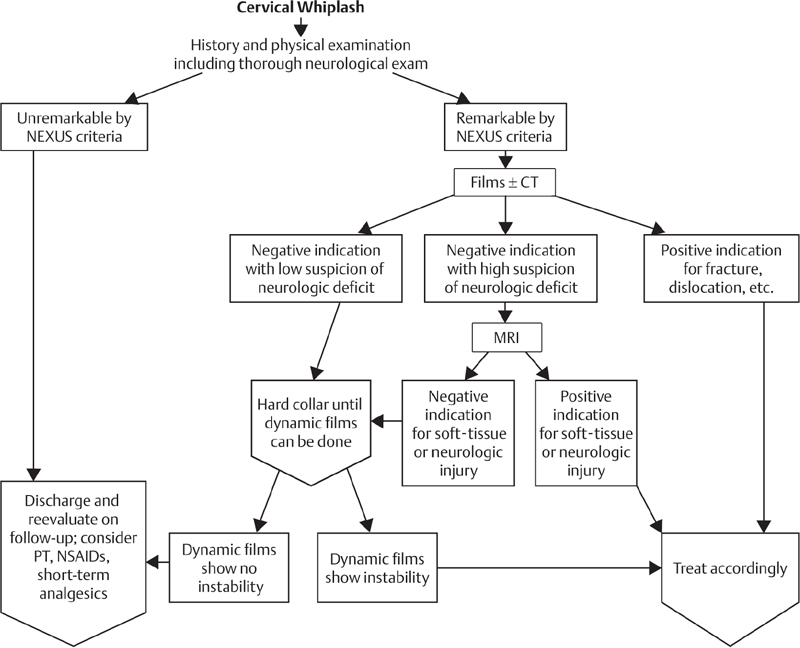
![]() Classification
Classification
![]() Workup
Workup
History
Physical Examination
Spinal Imaging
![]() Treatment
Treatment
![]() Outcome
Outcome
![]() Complications
Complications
Suggested Readings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







