CHAPTER 42 Ossification of the Posterior Longitudinal Ligament
History
Despite reports of ossification of the posterior longitudinal ligament (OPLL) by Key in 18381 and by Oppenheimer in 1942,2 it was not recognized as a distinct clinical entity until 1960. The first report in Japan of cervical compressive myelopathy caused by OPLL was based on autopsy findings obtained by Tsukimoto in 1960.3 Onji and colleagues4 reviewed clinical symptoms of 18 cases of OPLL in 1967. Since then, many reports of OPLL have been published, and it has been recognized as a common clinical entity that causes compression myelopathy, especially in Japan. The Investigation Committee on Ossification of the Spinal Ligaments, organized by the Japanese Ministry of Public Health and Welfare, has conducted studies of the etiology of OPLL and patient care for OPLL since 1975. Their studies of the pathogenesis, diagnosis, and treatment of OPLL have contributed to improvement in management of OPLL and other spinal disorders in Japan.
OPLL is a common cause of cervical myelopathy in middle-aged and older Japanese adults. Although OPLL has been thought to be rare among whites and to be a “Japanese disease,” several reports of OPLL in whites and in natives of other Asian countries have been published.5 Several studies of growth factors, cytokines, and other molecular and genetic factors in OPLL have been reported, but the etiology of OPLL has not yet been fully elucidated.
Etiology
OPLL has been found in 26% of the parents of probands and 29% of the siblings of probands.6 Familial surveys and human leukocyte antigen (HLA) haplotype studies reveal that genetic background plays an important role in the occurrence of OPLL. A genetic locus for OPLL is thought to be located close to the HLA region, on chromosome 6p. Although a candidate gene in the region, the gene for collagen 11A2, has been analyzed for the presence of molecular variants in affected probands, the pathogenesis of OPLL does not seem to be entirely the result of defects in this gene.7
Pathology
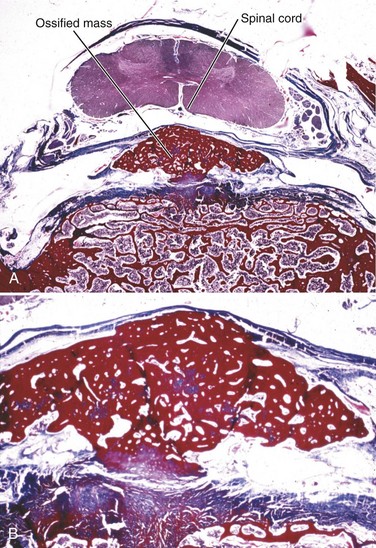
Although OPLL was previously thought to involve calcification of the posterior longitudinal ligament, studies have shown that it actually involves ossification of the ligament.8 OPLL involves ectopic bone formation within the spinal ligaments. The mature form of the ossification consists of lamellar bone with well-developed haversian systems. Immature lesions are often accompanied by woven bone with fibrocartilaginous cell proliferation in the marginal area (Fig. 42–1). The main characteristics of OPLL are as follows9,10: (1) ossification accompanied by ligamentous tissue hyperplasia and cell proliferation; (2) sequential occurrence of fibrocartilaginous cell proliferation, calcification, and tissue resorption with vascular ingrowth; and (3) ossification of the ligament that occurs at specific sites of predilection and often in combination with diffuse idiopathic skeletal hyperostosis.11 The ossification process of the ligament is not always endochondral ossification but sometimes is membranous ossification.10
The posterior longitudinal ligament is initially replaced with bony tissue. Hyperplasia of the fibrocartilaginous tissue may occur in the posterior aspect of the intervertebral disc, extending into the ossified posterior longitudinal ligament.9 Progression of ossification follows an evolutionary process, beginning as endochondral or membranous ossification. There may be no correlation between disc degeneration and occurrence of OPLL.8 Generally, in cases of dense OPLL, normal disc thickness is maintained in the cervical spine, and there are no signs of inflammation or bleeding in these areas of ossification.9
Myelopathy caused by OPLL is characterized by chronic compression of the spinal cord. Autopsy studies of OPLL show the following pathologic characteristics12,13: (1) Demyelination and loss of axon, which is more dominant in the posterolateral than in the anterior column, is observed in the white matter; (2) pathologic changes are restricted to the gray matter, and the white matter is preserved in cases with a boomerang shape in which the transverse area of the spinal cord is greater than 60% of the normal; (3) a triangular shape in which the transverse area of the spinal cord is reduced to less than 60% of the normal is associated with severe and irreversible pathologic changes showing white matter and gray matter are severely involved, and only the anterior column is preserved.
Metabolic Background
A high incidence of diabetes mellitus (non–insulin-dependent) and impaired glucose tolerance has been reported among patients with OPLL.14,15 Glucose tolerance tests of 535 patients with OPLL showed that 28% were diabetic, and 18% were borderline diabetic.16 There have also been reports of a relatively high incidence of OPLL and hormonal disorders such as hypoparathyroidism and hypophosphatemic rickets among diabetic patients.16 This finding seems to implicate abnormal calcium metabolism in ossification of the ligaments, although conventional blood chemistry tests have shown no abnormalities in patients with OPLL.16
Epidemiology
Incidence
The incidence of OPLL in Japanese older than 30 years of age has been reported to range from 2% to 4%. In Taiwan, Korea, Hong Kong, and Singapore, the incidence of OPLL reportedly ranges from 0.8% to 3%.5 In the United States and Europe, the incidence of OPLL reportedly ranges from 0.1% to 1.7%.5 In a survey of 599 patients in Utah University Hospital, 8 patients (1.3%) were found to have OPLL in the cervical spine.5,8
Natural History of Myelopathy
A cohort study showed that all patients with more than 60% spinal canal stenosis by OPLL exhibited cervical myelopathy.17Although static compression of the spinal cord is the main cause of myelopathy in OPLL, radiologic findings do not always correlate with clinical severity of neurologic manifestations. In a study of the natural history of 207 patients with OPLL over an average period of 10 years, clinical symptoms did not change in 66% of patients, and myelopathy developed in 16% of patients.18 Kaplan-Meier analysis of 323 patients who did not have myelopathy at their initial evaluation showed a myelopathy-free rate of 71% after 30 years.19
Despite spinal stenosis (6 mm < space available for the spinal cord < 14 mm), myelopathy may not develop in patients with the severe limitation of range of motion of the cervical spine.19,20 This finding indicates that not only static factors, but also dynamic factors such as listhesis or hypermobility at discontinuity of the ossified lesion play important roles in the development of myelopathy, especially in mixed or segmental OPLL.
Presentation
Location
Although OPLL has been observed at all levels of the spine, it occurs most frequently in the cervical spine. Thoracic OPLL occurs at the upper and middle thoracic levels.16 In contrast, ossification of the ligamentum flavum (OLF) is frequently observed at the lower thoracic level and the thoracolumbar junction. Lumbar OPLL occurs relatively infrequently, and it does not usually cause severe disabilities.
Symptoms
Many patients with subclinical or latent OPLL are asymptomatic, and many patients with large ossified lesions experience no disability. Symptoms most typically include myelopathy or myeloradiculopathy rather than radiculopathy alone. The symptoms develop secondary to spinal cord compression caused by the space-occupying lesion of the ossified ligament. These neurologic symptoms develop insidiously without any obvious causes in 80% to 85% of patients, but acute onset or aggravation of the symptoms is often related to a minor trauma or hyperextension of the neck.16
Patients can be divided into three groups according to their neurologic symptoms: (1) patients with spinal cord signs presenting with motor and sensory disturbances predominantly in the lower extremities; (2) patients with segmental signs presenting with motor and sensory disturbances predominantly in the upper extremities; and (3) patients presenting with pain in the neck, shoulder, and arm region without obvious neurologic deficits (axial symptoms alone).9
Diagnosis
Physical Examination
The most common complaint at onset of OPLL is paresthesia or numbness in the hands. Clumsiness of the hands is another symptom. The complaints gradually extend to the lower extremities, leading to gait disturbance. Physical examination generally reveals spasticity of the lower extremities with exaggerated deep tendon reflexes and sensory disturbance in upper and lower extremities. Patients sometimes complain of neck pain or discomfort around the neck. Myelopathy affecting the hand, as indicated by the tests (finger escape sign and 10-second grasp and release test) proposed by Ono and colleagues,21 is a sensitive and specific sign of pyramidal tract involvement in the cervical spine. It is important to differentiate OPLL from other skeletal and neurologic disorders, including cervical spondylosis, spinal cord tumor, periarthritis of the shoulder, entrapment neuropathy in the upper extremities, and motor neuron disease.8
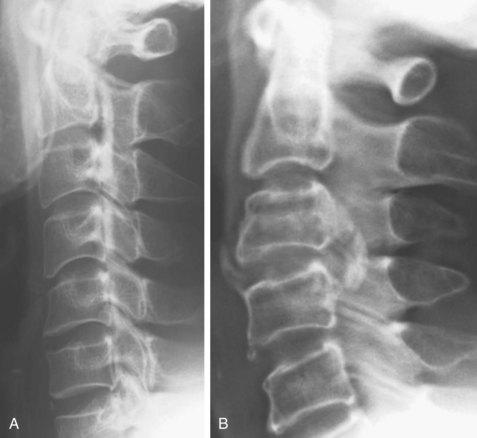
Plain Radiography
Narrow disc spaces or spondylotic changes are occasionally observed at the lower cervical region of OPLL patients, but disc spaces located in the ossified area are usually well preserved.9 There is no involvement of sacroiliac joints or apophyseal joints, which is usually observed in cases of ankylosing spondylitis.
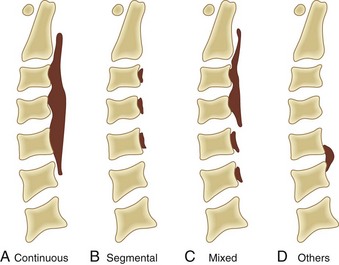
Based on radiographic findings, cervical OPLL is classified into four types (Fig. 42–2): (1) continuous type, in which ossification extends over several contiguous vertebrae; (2) segmental type, in which ossification is fragmented and located immediately behind each vertebral body with interruption at the intervertebral disc levels; (3) mixed type, which is a combination of continuous and segmental types of ossification; (4) others type (circumscribed or localized), in which ossification is confined to the intervertebral disc space.16 In addition to this conventional typing, sagittal shape of the ossified lesion is classified into plateau-shaped or hill-shaped (see Fig. 42–6).22 Plateau-shaped ossification, which is found in segmental-type OPLL and most continuous-type and mixed-type OPLL, is characterized by a narrow spinal canal without massive localized ossification. Hill-shaped ossification, which is found in circumscribed-type OPLL and some cases of continuous-type or mixed-type OPLL, shows massive beak-shaped ossification localized to certain levels.
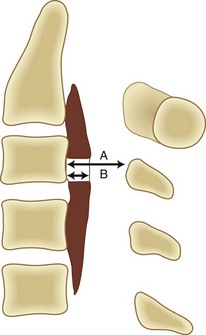
The occupying ratio of OPLL is calculated as the ratio of the maximum anteroposterior thickness of OPLL to the anteroposterior diameter of the spinal canal at the corresponding level on a lateral radiograph or tomogram (Fig. 42–3).16 An occupying ratio greater than 60% indicates high risk of the development of myelopathy.17,23 Matsunaga and colleagues19,20 reported that with a constant tube-to-film distance of 150 cm, all of the patients with a value of space available for the spinal cord (SAC) of less than 6 mm had myelopathy, whereas none of the patients with SAC of 14 mm or more developed myelopathy. They also reported that in patients with myelopathy whose minimal SAC diameter ranged from 6 mm to less than 14 mm, the range of motion of the cervical spine was significantly greater.18,20 These results suggest that the primary factor in the development of myelopathy is reduced SAC diameter resulting from static compression by the ossified ligament, although below the critical point (SAC >6 mm or maximum spinal canal stenosis ≤60%), dynamic effects seem to be the main factors in the development of myelopathy.
Computed Tomography
Computed tomography (CT) is particularly useful for imaging of the lower cervical spine and visualizing ossification that is difficult to detect with plain radiographs (Fig. 42–4). Because of the high frequency of association of cervical OPLL with thoracolumbar OPLL and OLF, a preoperative survey should include imaging of the entire spinal column. Because it is difficult to detect ossified lesions at the cervicothoracic and thoracolumbar junctions on plain radiographs, careful preoperative and postoperative CT or magnetic resonance imaging (MRI) or both should be performed to assess spinal stenosis throughout the entire spine. Myelography is useful to assess spinal canal stenosis by OPLL or OLF or both from the cervical spine to the lumbar spine, and combined myelography and CT is mandatory for planning of anterior removal or floating of the ossified lesion.
Magnetic Resonance Imaging
MRI is not effective for detection of OPLL because OPLL lacks signal intensity on T1-weighted and T2-weighted images (Fig. 42–5). Bone marrow within the ossified lesion appears as an isointense or hyperintense area, however. MRI can illustrate pathology of the spinal cord. Kameyama and colleagues12 reported that in cases of OPLL, a triangular spinal cord with a transverse area of less than 60% of normal in more than one segment seemed to be associated with severe and irreversible pathologic changes. MRI is also useful for detection of cervical disc herniation. In one study, disc protrusion was detected in 81% of patients with segmental OPLL, and intramedullary hyperintensity was observed on T2-weighted images in 43% of the patients whose neurologic deficits were significantly more severe than average (see Fig. 42–5B).24
Treatment of Ossification of the Posterior Longitudinal Ligament of the Cervical Spine
Conservative Treatment
A cervical orthosis and skull traction are used in conservative treatment of OPLL. Such conservative treatment is indicated to eliminate dynamic factors of the cervical spine for patients whose predominant complaint is neck, shoulder, and arm pain (local pain, radicular pain, or both) without any symptoms of myelopathy or patients with mild ossification in whom myelopathy is subclinical and not predominant.25 It is important to advise patients with OPLL not to hyperextend the neck and to be vigilant regarding trauma and falls secondary to motor vehicle accidents, sports activities, or excessive alcohol intake.25
Surgical Treatment
Surgical decompression of the spinal cord is necessary for patients with apparent myelopathy because long-term compression of the spinal cord may cause irreversible degeneration. For patients with symptoms and signs of moderate or progressive myelopathy, the authors recommend early surgical decompression, especially for younger patients with a narrow spinal canal, because reports indicate that better neurologic recovery is associated with younger age at operation and milder myelopathy.26 Even if the myelopathy is mild, surgery may be indicated for patients with severe spinal stenosis (SAC ≤6 mm or occupying ratio ≥60%). There is no evidence indicating the effectiveness of prophylactic surgery for patients who have no symptoms or signs of myelopathy.23
Authors’ Preferred Choice of Surgical Procedure
There is some controversy over the appropriate method of surgery for myelopathy caused by cervical OPLL. In Japan, most surgeons use an anterior approach with extirpation or floating of the ossified lesion or a posterior approach including various types of expansive laminoplasty. The choice between two approaches should be based on the following considerations: skill of the surgeon, age and general condition of the patient, extent of ossification, OPLL type and sagittal shape of the ossified lesion (plateau-shaped [Fig. 42–6A] or hill-shaped [Fig. 42–6B]), OPLL occupying ratio, sagittal curvature of the cervical spine and spinal cord (kyphotic or lordotic), and intervertebral mobility at the maximum compression level (dynamic factors).22,27–30
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree