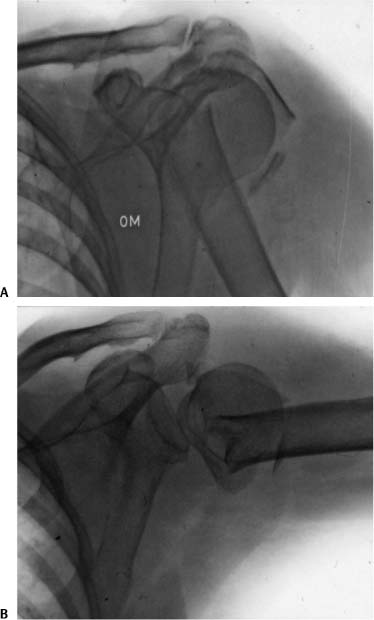
8 Operative Treatment of Proximal Humeral Nonunions In general, surgical neck fractures of the proximal humerus heal with nonoperative treatment. Good and excellent results can be expected after anatomic reduction and stable internal fixation of fractures of the proximal humerus.1 Therefore, the prevalence of delayed union and nonunions after conservative and operative treatment is low. The etiology of nonunions following conservative treatment is severe displacement or interposition of soft tissue. Failed internal fixations are based on excessive soft tissue dissection, neglect of the basic principles of internal fixation, and finally vascular disturbance of the fracture area itself. For both treatment modalities, aggressive physiotherapy and poor patient compliance might be reasons for the nonunion as well.2 Established nonunions of the surgical neck pose a significant disability to the patient, causing pain, instability, and limitation of motion of the shoulder joint. In general, the patients are elderly and often have associated medical problems, posing a treatment challenge to the surgeon. Despite these obstacles, we believe that a joint-preserving approach is indicated because the functional outcome of hemiarthroplasty is questionable.3 In comparison with femoral neck fractures, a proximal humeral fracture should unite within 4 months, otherwise we consider it a nonunion. These nonunions are usually atrophic as a consequence of motion in the nonunion, leading to bone resorption with cavitation of the humeral head and producing a true pseudarthrosis. The combination of nonunion and humeral head necrosis is theoretically possible, but not seen in our series because most proximal humeral nonunions develop after two-part fractures of the surgical neck. Nonunions after three- and four-part fractures are rare.4 We might classify the proximal humeral nonunions in two specific types: Type A are nonunions with a rather big, well-vascularized head-metaphyseal fragment; type B are nonunions of the surgical neck leading to resorption with excavation of the humeral head. Previous operation reports and analysis of the available x-rays will give the necessary information concerning the quality of the bone and rotator cuff. Range of motion (ROM) and neurovascular examination should be assessed before the operative intervention. A detailed examination of the axillary nerve function is critically important as well. Most or all of the shoulder motion results generally from motion at the false joint rather than at the glenohumeral joint (Fig. 8–1). In those hyper-mobile nonunions, forward elevation is impossible or at least modest. Severe muscle atrophy is present and the rotator cuff function is difficult to assess. Standard anteroposterior and axillary radiographic examination is generally sufficient. Computed tomography (CT) or magnetic resonance imaging (MRI) has no influence on the indication for operative treatment. Fluoroscopy allows the evaluation of the ROM in the glenohumeral joint and in the nonunion. Stiffness occurs only when the tuberosities are involved. The goal of the preoperative evaluation is to decide which technique is most suitable and if bone grafting is indicated. Infection can be excluded by clinical examination and appropriate blood studies including complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein screening, and radionuclear scanning. All concomitant comorbid medical conditions need optimal treatment before the intervention. Figure 8–1 Type B nonunion – technique II (see Fig. 8–6). Not every nonunion needs surgical treatment: Operative interventions are indicated in patients whose nonunions cause relevant pain and result in a nonfunctional shoulder. Different stabilization techniques are used–intramedullary rods (Rush, Ender, etc.), intramedullary cortical bone grafts, open reduction, and internal fixation with tension-band techniques and plates.2–10 Recently, the use of proximal humeral locking plate fixation techniques has been advocated for these nonunions. Those techniques are described in Chapter 4. Fixation problems that one encounters in the treatment of acute proximal humeral fractures are often magnified in the setting of a nonunion. Nevertheless, the same principles, techniques, and implants are used to create the optimal stability that is necessary for any nonunion treatment. Approach and implant should not compromise the vascularity of the nonunion and the humeral head. Extra stability and biological stimulation by autologous bone grafting are often required, especially in atrophic nonunions of the resorption type. Analyzing the literature and our own experience with referred patients, we conclude that the overall results of surgical treatments with nails of any type have not been satisfactory. Open reduction and internal fixation is the method of choice in the treatment of proximal humeral nonunions. The principles of internal fixation are the same as in the primary fracture treatment.1 Simple tension-band techniques may be sufficient if impaction of the shaft into the head of the humerus leads to intrinsic stability.1,7 Concerning surgical approaches, the use of blade plates is less invasive than those of T-plates, but for both similar results have been reported.1,5,6 Double plating in combination with bone grafting using semi- or third-tubular plates is a valid alternative when there is cavitation of the humeral head (Fig. 8–2)
Classification
Patient Assessment
History
Physical Examination
Radiologic Evaluation
Laboratory Studies
Treatment
Nonsurgical Treatment
Surgical Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree