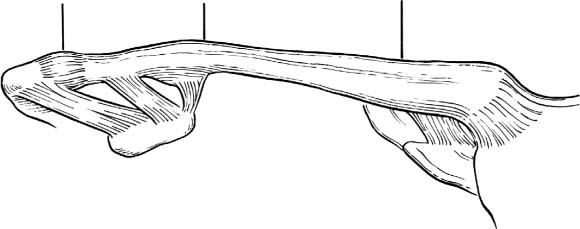
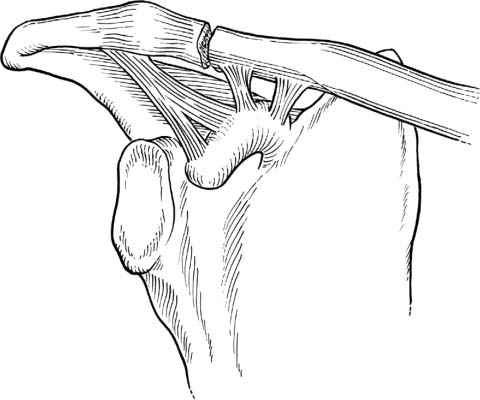
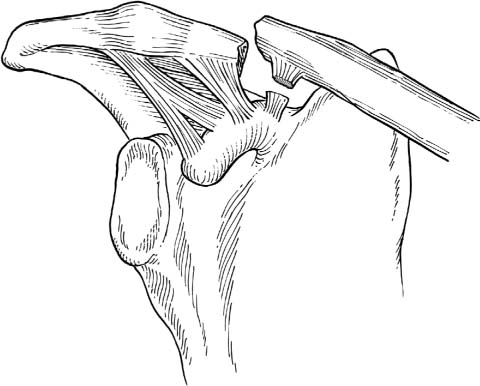
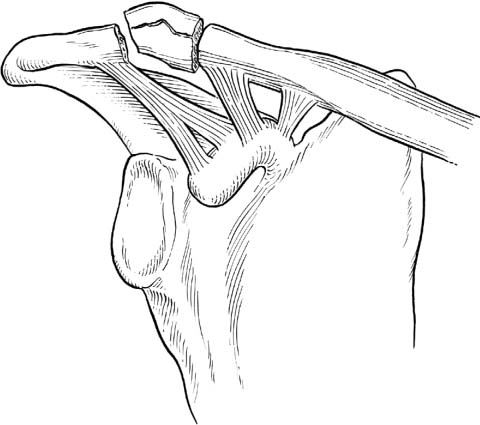
1 Operative Treatment of Fractures of the Clavicle We are proud that our brains are more developed than the animals: we might also boast of our clavicles. It seems to me that the clavicle is one of man’s greatest skeletal inheritances, for he depends to a greater extent than most animals, except the apes and monkeys, on the use of his hands and arms. E. A. Codman, 1934 The incidence of clavicle fractures accounts for ~50 per 100,000 inhabitants per year; only 4% of all fractures involve the clavicle. The management of this fracture, however, has recently evolved because new evidence has demonstrated the importance of the proper healing of the clavicle. With the newfound importance of fitness as a principle of life and the resulting increase in sports activities, clavicle fractures are occurring more frequently in the general population, predominantly in young people. Today, fast, successful treatment without sequelae is a matter of economic importance and a topic of discussion in public affairs. The clavicle is an S-shaped tubular bone with a medial anterior and a posterior lateral convexity. The length varies proportionally to the size of the individual, whereas the male clavicle usually is longer in the middle. The diameter at the medial metaphysic measures 18 mm, at the lateral 15 mm, and at the diaphysis ~7 mm. The narrowest diameter is measured at the meeting point of the two half circles of the S-shaped clavicle, the most frequent location of clavicle fractures. The medial clavicle shows a tubular form; however, laterally it becomes more and more flat on the cranial and caudal face to provide a congruent articulation with the corresponding acromion. It provides attachments for the deltoid, trapezius, sternocleidomastoid, pectoral, and subclavius muscles, which are responsible for the typical displacement seen in mid-shaft fractures. As the clavicle lies subcutaneously throughout its length and contours the upper trunk with its connection to the upper extremity, the fracture deformity also becomes an aesthetic problem. The clavicle is the only tubular bone with a mesenchymal ossification, which starts in the embryo and ends in the third decade (mean age: men, 26 years; women, 25 years). The medial epiphyseal end is responsible for 80% of the clavicle’s growth. Because of the late closure of the epiphyseal growth zone, growth plate separations must be considered in children or younger patients experiencing pain or tenderness proximally or distally over the clavicle. The clavicle is the only link connecting the trunk with the arm. With the above-mentioned muscles, it contributes, together with the thoracoscapular and glenohumeral joints, to the movement of the upper extremity. As a distance holder and strut, it represents an unavoidable link for overhead work, stabilizing the glenohumeral joint, especially in the sagittal plane, and providing a stable, efficient center of rotation for the shoulder joint.1 In the case of trauma, the middle third of the clavicle has to withstand the greatest bending and torsional forces. The clavicle also protects the underlying neurovascular structures. With the surrounding muscles, especially the sternocleidomastoid muscle, the clavicle has an important function in respiratory function; hence, the treatment of injury to the clavicle must be considered in situations where there is a concomitant injury to the rib cage. Based on anatomic peculiarities and typical fracture conditions, the clavicle is divided into three thirds as classified by Allman (Fig. 1–1).2 The medial or proximal part is small and extends from the sternoclavicular joint to the lateral attachment of the costoclavicular ligament. The midportion is the biggest and reaches to the medial beginning of the conoid part of the coracoclavicular (CC) ligament. Fractures lateral to the conoid are therefore described as distal clavicle fractures. For each third, a separate structure classification exists, whereas the one for the medial fractures described by Craig3 lacks the benefit of general classification itself. Medial fractures are rare, and the scarcity of data makes evidence-based conclusions about treatment difficult. We do not use this classification in our clinic; however, we recognize its significance when involved in a comparative investigation. The Academy of Orthopedics/American Association for the Study of Internal Fixation (AO/ASIF) classification is widely used for fractures of the middle third and has been found helpful in therapy decisions. Type A is described as a simple transverse fracture, type B is a wedge fracture, and type C is a comminuted fracture with no contact with the main fragments. Figure 1–1 Classification of midshaft clavicle fractures as per Allman.2 (A) proximal fractures from the sternoclavicular joint to the costoclavicular ligaments, (B) midshaft fractures from the costoclavicular ligaments to the coracoclavicular ligaments, and (C) distal fractures from coracoclavicular ligaments to the acromioclavicular joint. For the lateral third of clavicle fractures, Neer’s classification4 remains the gold standard. Adaptations by Rock-wood5 or Breitner and Jager,6 offer no additional benefit particularly in treatment decisions. Neer’s type I (Fig. 1–2) is a stable fracture located laterally from the nondisabled CC ligaments. In Neer’s type II (Fig. 1–3), the fracture lies between the conoid and trapezoid components of the CC ligaments. The medial part, the conoid ligament, is ruptured, but the distal one, the trapezoid, remains intact. Infrequently, both ligaments are ruptured and combined with a distal clavicle fracture. If we have intact ligaments with a proximal fracture we classify it with the midshaft fractures. Occasionally, distinction is difficult if radiographic displacement of the proximal fragment gives no hint of ligament damage. Neer’s type III (Fig. 1–4) describes a fracture extending into the acromioclavicular (AC) joint. The division in stable and unstable fractures is helpful for dictating further treatment. Figure 1–2 Classification of distal clavicle fractures: type I. Fractures distal to the coracoclavicular ligaments, which remain intact. Figure 1–3 Classification of distal clavicle fractures: type II. Fractures in between the coracoclavicular ligaments with rupture of the conoid ligament. Figure 1–4 Classification of distal clavicle fractures: type III. Fractures distal to the coracoclavicular ligaments (like type I) with extension into the acromioclavicular joint. The frequency of clavicle fractures due to trauma is 2.6 to 4%.7,8 Although this is a small percentage, with increasing recreational activities clavicle fractures are occurring more frequently, 52 in 1952 compared to 64 per 100,000 in 1987.9 In the only prospective trial, Nowak et al8 found in the years 1989 to 1990 a frequency of 50/100,000 inhabitants (males 71/100,000, females 30/100,000). Clavicle fractures represent 35 to 44% of all fractures of the shoulder girdle.7,10 They are more common in males under 30 years of age. Because of the strong fixation of the ends of the clavicle by surrounding ligaments the thinner middle part, 80% are located in the midthird. Among these, 48% are displaced and 19% comminuted7; 10 to 18% of these fractures are distal, and 2 to 10% of fractures are of the medial third of the clavicle.11 Fractures of the medial third show a mean age of 51 years, of the midthird 21 years, and of the distal third 47 years. Patients over 75 years in age show an increasing frequency of medial or distal third clavicle fractures.9 Regarding the fracture displacement, age distribution, nondisplaced fractures have a mean age of 11 years, minimally displaced fractures have a mean age of 27 years, and comminuted fractures have a mean age of 43 years. During clinical examination, the complaints and posture of the patient, local signs of swelling, bruising, and deformity may make the diagnosis evident. The diagnosis is confirmed by an anteroposterior (AP) and 45% cranially and caudally angled radiograph of the injuries located in the middle third of the clavicle. Evaluation should be performed on the vertebral column, proximal humerus, shoulder girdle, and upper thorax and lung, particularly in multiply injured patients. Ignorance of these concomitant injuries can lead to inappropriate treatments. Lateral fractures additionally need axillary radiographs centered on the AC joint. To distinguish stability of lateral fractures, it is sometimes necessary to perform a radiograph with a 5-kg weight pulling on the arm. In these cases, we highly recommend local anesthesia on the affected side. Secondary to the multiple overlying structures of the upper thorax, a fracture of the medial clavicle is often difficult to visualize on plain x-ray. A computed tomography (CT) scan is recommended in cases with obvious signs of injury. Ultrasound can be helpful in children and newborns. Careful neurologic and vascular examinations should be performed in all patients with clavicular injuries. Concomitant injuries such as pneumo- and hemothorax or neurovascular damage have been reported, but are uncommon. In 87% of clavicle fractures, the cause is a fall on the shoulder – either a direct blunt trauma or a fall on the outstretched arm. These injuries are often common in contact sports and cycling, motorcycling, skiing, and riding. The results of operative treatment are always compared with the results of a conservative therapy treatment. Lester in 1929 described the use of plaster spicas, splinting devices, bandages, or simple slings (more than 200 methods) in the treatment of midclavicular fractures. Some clinicians favor reduction, putting a knee between both shoulder blades, others a redressing figure-eight bandage. In a 1987 prospective randomized study, Andersen12 demonstrated identical functional and cosmetic results, comparing a figure-eight bandage and a simple sling. The initial displacement remained unchanged in each group, whereas the simple sling caused less discomfort and perhaps fewer complications. The widely accepted treatment is a simple immobilizer from a few days up to 3 weeks to reduce pain. Elevation over 90 degrees and strengthening should begin after clinical consolidation of the fracture is evident. After 8 to 12 weeks and radiographic healing, shoulder strengthening work and contact sports may be considered. Nondisplaced and minimally displaced fractures will heal with symptomatic treatment and little concern regarding either cosmesis or function. Nordqvist et al13 found among 225 conservatively treated midclavicle fractures, 185 (82%) asymptomatic, 39 (17%) with moderate pain, and 1 (0.4%) with significant pain. In this retrospective study with a mean follow-up of 17 years (12 to 22 years), 68% were displaced and comminuted fractures. This study showed a 24% malunion and a 3% nonunion rate; however, the majority of these patients with radiographic abnormalities had good outcome in this long-term investigation. In contrast, Hill et al14 reviewed 52 midclavicle, completely displaced fractures with a mean follow-up of 38 months, and found 15% nonunions and 31% unsatisfactory results. No patient had significant impairment of range of motion; however, 13 (25%) patients had mild to moderate pain, 15 (29%) had some evidence of brachial plexus irritation, and 28 (56%) had cosmetic complaints. In 2005, Nowak et al15 evaluated prospectively an evaluation of 222 patients with clavicle fractures. They showed 42% of patients treated nonoperatively continued to have significant sequelae 6-months postinjury. The nonunion rate was only 7%; therefore, other symptoms were responsible for their complaints. Displacement of more than one bone width was the strongest radiographic risk factor for symptoms and sequelae. A comminuted fracture and older patients were associated with increased risk of symptoms persisting at 6 months. Regarding sequelae after clavicle fractures, it is important to focus not only on nonunion, which may have no clinical symptoms, but to concentrate more on malunion, which can be responsible for pain, neurovascular symptoms, cosmetic complaints, and functional deficits. Because of the results related above, the decision for operative treatment results in extremely controversial discussions. Without a doubt, therapy for children is in the domain of nonoperative treatment. In children, even displaced fractures are treated with a short immobilization in a sling or a figure-eight bandage. In adults, only absolute indications for surgical treatment include open fractures, fractures with neurovascular damage, refracture, or floating shoulders with midclavicular and Neer’s type II fractures of the distal clavicle. More controversial indications for operative treatment include displacement, comminution or shortening, multiply injured patients, and patients with injuries of the lower extremity and the need for the use of crutches. These questions concern predominantly midclavicular fractures; surgical indications for the proximal and distal clavicle are more evident. Secondary to the low incidence (2% of clavicle fractures), recommendations for treatment of the sternal and clavicle fractures are based on case reports or small series reported in the literature. We find that these fractures, which seldom are significantly displaced, can be treated conservatively in a sling for a few weeks. As patients with this fracture are middle-aged on average, one must be careful not to overlook fractures in younger patients where epiphyseal fusion may not have yet taken place. Because the medial epiphyses typically remain open into the third decade of life, it is important to recognize that apparent sternoclavicular dislocations in some young adults may actually be epiphyseal separation injuries.16,17 Epiphyseal fracture can be difficult to recognize on a CT scan. In rare cases such as an open fracture, operative stabilization may be indicated. Plating should be chosen because pin migration after tension band wiring is a concern with potentially devastating complications. Pin displacements into the aorta and a pin coughed up in the lung have been reported in the literature. Some authors recommend conservative treatment in general because of good therapy options with resection of the sternal end of the clavicle, if the deformity is symptomatic later. The most frequent fracture is the midthird fracture. The middle third of the clavicle actually represents nearly half of the length of the clavicle from the costoclavicular to the CC ligaments. All former studies unanimously called for conservative treatment of all clavicle fractures; however, recently there is some doubt as to the best treatment choice. The sentence “Most clavicle fractures are treated conservatively and heal uneventfully with good outcome” is not true. On behalf of the Evidence-Based Orthopaedic Trauma Working Group, Zlowodzki et al18
Anatomy and Embryology of the Clavicle
Function of the Clavicle
Classification
Epidemiology
Patient Assessment
Fracture Mechanism
Treatment
Nonsurgical Treatment
Surgical Treatment
Fractures of the Proximal Third of the Clavicle
Fractures of the Middle Third of the Clavicle
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree