Open Surgical Débridement for Femoroacetabular Impingement
Rafael J. Sierra and Robert T. Trousdale
Key Points
• Trochanteric slide osteotomy with anterior capsulotomy and anterior dislocation of the hip provides
• Supervised rehabilitation is valuable in enhancing recovery.
Introduction
Femoroacetabular impingement (FAI) occurs when the proximal femur repeatedly contacts the native acetabular rim during normal or abnormal hip range of motion (ROM).1–5 It most commonly occurs with flexion and internal rotation but may also occur with extension and external rotation. It is well recognized now that FAI is a mechanism that leads to osteoarthritis (OA),1–4 and its role as a prearthritic hip condition has been studied extensively. Treatment of FAI is aimed at restoration of normal structural anatomy about the hip.5,6 Open surgical hip dislocation has been the gold standard for management of the patient with FAI.6–8 The aim of this chapter is to discuss the indications, contraindications, technique, and postoperative care associated with surgical hip dislocation for treatment of FAI.
Indications
A good candidate for femoroacetabular impingement (FAI) surgery through surgical hip dislocation is a patient who (1) has reasonably preserved articular cartilage, (2) has a correctable structural abnormality that involves both femoral and acetabular sides with or without labral chondral pathology, and (3) understands limitations and outcomes of the procedure. Relative contraindications include (1) patients into the fourth and fifth decades of life or greater, (2) patients with Tonnis grade II osteoarthritis (OA) unless extremely young, (3) patients with a retroverted acetabulum with poor posterior coverage (a reverse periacetabular osteotomy [PAO] would be a better option), and (4) patients with anterior translation of the femoral head into an anterior acetabular cartilage defect, as seen radiographically or on magnetic resonance imaging (MRI). Absolute contraindications include (1) patients with Tonnis grade III or higher OA, (2) patients with hip pain with an uncorrectable structural deformity, (3) infection, and (4) the older patient with advanced degenerative joint disease for whom total hip arthroplasty (THA) would be a better option.
Preoperative Planning
The anteroposterior pelvic radiograph provides useful information for planning a surgical hip dislocation. Interpretation of this x-ray, however, is very sensitive to the position of the pelvis at the time of exposure. It is commonly accepted now that a well-centered anteroposterior pelvic view is obtained when there is symmetry of the iliac wings and of the obturator foramina, and when the coccyx is at a point in the midline at a distance 0 to 2 cm above the symphysis pubis.9 A well-centered radiograph is very important in assessing structural anomalies about the pelvis and the proximal femur. Plain radiographs are used to assess retroversion of the acetabulum or whether coxa profunda or protrusion is present10–13 and to study the shape of the proximal femur. The shape of the femoral head is classified as “pistol grip” if the lateral contour of the femoral head extends in a convex shape to the base of the neck, and is classified as aspherical if the epiphysis of the head protrudes laterally out of a circle drawn around the contour of the head.6,14,15
An MRI arthrogram also helps with preoperative planning. The protocol for obtaining magnetic resonance arthrography (MRA) has been described previously.16 In brief, axial, coronal, oblique, sagittal oblique, and radial sequences are obtained. This last sequence is useful for evaluating the proximal femur and for calculating the alpha angle, and it has been useful in evaluating the localization of labral tears (see Chapter 31).17 Acetabular cartilage degeneration is less reliably seen on MRI.18–21 Assessment of the status of the cartilage is very important when surgical intervention is planned. In patients with FAI, the cartilage lesion is often anterosuperior, and in patients with advanced cam-type FAI, this may be seen as extensive chondral lesions as a result of the outside-to-in shearing mechanism. Superior and lateral acetabular cyst formation can also be seen on MRI and is indicative of more advanced disease.
For patients with symptomatic coxa profunda or protrusio, surgical hip dislocation for acetabular rim trimming would be the treatment of choice for management of their global overcoverage; however, they may benefit from a PAO or intertrochanteric osteotomy. Patients with large retroverted acetabulae with labral pathology who require rim trimming are also good candidates for surgical hip dislocation. Patients with isolated cam impingement with a normal acetabular contour and minimal labral pathology may be treated with less invasive procedures such as hip arthroscopy22–37 or the anterior Hueter or Smith-Petersen approach.38–40 Indications for less invasive procedures are continually evolving, and there is certainly a trend toward less invasive techniques for management of patients with FAI. Only time will tell whether the results of arthroscopic treatment are comparable with those of open treatment.
Description of Technique
The patient is placed in the lateral decubitus position. A straight incision distal to the iliac crest crossing anterior to the greater trochanter and over the proximal femur is made. For the fascial incision, a Gibson approach, which preserves the anterior aspect of the gluteus maximus, or a Kocher-Langenbech split of the gluteus maximus can be performed. We prefer the Kocher-Langenbech because the length of the skin incision is smaller, allowing access to the posterior aspect of the hip. The trochanteric bursa is incised longitudinally with the incision. Then a trigastric trochanteric osteotomy is performed. The osteotomy should not be performed under, but should end within, the trochanter proximally to protect the medial femoral circumflex artery as it courses superiorly behind the greater trochanter, and to ensure that most of the tendon fibers of the piriformis remain on the stable portion of the trochanter (Figs. 55-1A and B). A safe distance is 5 mm anterior to the trochanteric overhang. The stable trochanter is preserved with most or almost all the piriformis and all the other external rotators (Fig. 55-2). A capsular exposure is performed posteriorly in between the interval of the piriformis and the gluteus minimus. Staying proximal to the piriformis tendon diminishes the risk of damage to the anastomosis between the deep branch of the medial femoral circumflex and the inferior gluteal artery that runs inferior to the piriformis. Elevate the gluteus minimus off the superior and posterior capsule down to the sciatic notch. The superior dissection can be carried anteriorly to the reflected head of the rectus, which becomes visible over the acetabular rim. Anteriorly and inferiorly, the insertions of the short head of the minimus onto the capsule should be released. The trochanteric fragment is retracted anteriorly throughout this exposure, facilitated by increasing flexion and abduction. A Z-shaped capsulotomy is started by carrying the capsulotomy along the long axis of the neck from distal to proximal, starting at the anterosuperior edge of the stable trochanter and coursing toward the acetabular rim (Fig. 55-3). The capsulotomy should be carried out with a knife from inside-out, so that the labrum is not damaged as the rim is approached (Fig. 55-4A and B). The distal limb of the Z-shaped capsulotomy is made longitudinally, anteriorly, and inferiorly at the level of the psoas tendon.
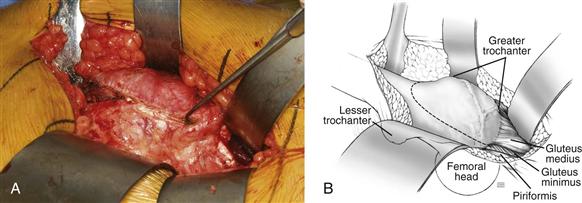
Figure 55-1 Surgical photograph and illustration depicting the posterior aspect of the trochanter with external rotators. Osteotomy should be performed 5 mm anterior to the posterior overhang of the trochanter. Posterior dissection should be carried out between the piriformis and the gluteus minimus.
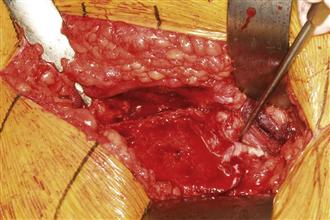
Figure 55-2 Surgical photograph depicting preservation of the piriformis and its attachment to the stable part of the trochanter.
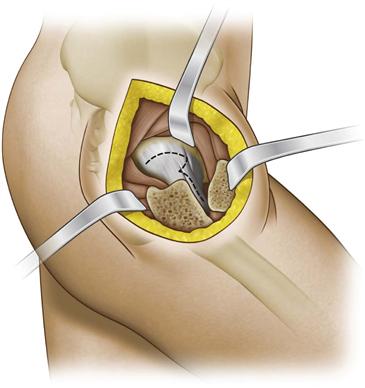
Figure 55-3 Z-shaped capsulotomy performed on the right hip. The capsulotomy is carried along the long axis of the neck from distal to proximal, starting at the anterior superior edge of the stable trochanter and moving toward the acetabular rim.
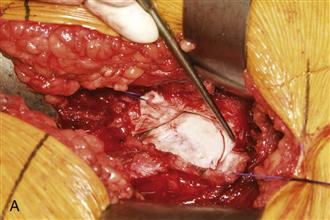
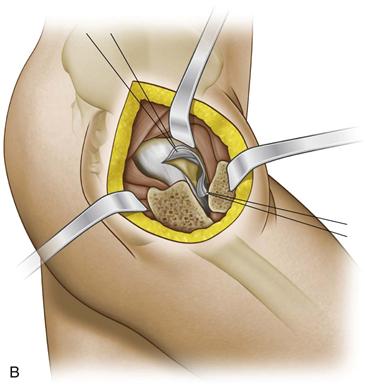
Figure 55-4 The capsulotomy should be carried out with a knife from inside-out, always with visualization of the labrum to prevent iatrogenic injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








