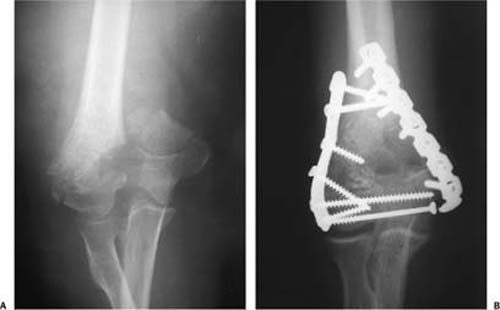
12 Open Reduction and Internal Fixation for Fractures about the Elbow in the Elderly Fractures about the elbow in the elderly are often complicated by metaphyseal comminution, poor soft tissue quality, and diminished bone mineral density. A clear understanding of the surgical decision-making process in osteoporotic elbow fractures is important to prevent failures and optimize the independence of an elderly patient. The surgeon’s ability to obtain stable fracture fixation and restore early function to the elbow has been enhanced by an improved understanding of elbow anatomy and newer techniques to optimize stability in elbow fracture fixation with improved implants. In this chapter, we will discuss the diagnosis, surgical treatment, and rehabilitation of fractures about the elbow in the elderly. Fractures around the elbow in the elderly remain one of the most demanding challenges in surgical fracture treatment. Elbow fractures can lead to significant disability in the elderly due to the difficulties inherent in their treatment, poor tolerance for joint immobilization, and the fact that up to 30% of these patients develop complications.1 Proper function of the elbow is central to positioning the hand in space for fine movements, powerful grasping, and serving as a fulcrum for the forearm.2 Loss of basic elbow function can severely affect activities of daily living. For an elderly patient who may have comorbid illnesses and limited mobility, these injuries can lead to the loss of independence. Fractures of the elbow comprise 7% of adult fractures with less than half of all elbow fractures arising in the distal humerus. Recent evidence suggests that the age-adjusted incidence of elbow fractures in women older than 60 years has more than doubled from 1970 to 1995.3 Although data on bone mineral density values for the elbow in large cohorts of patients are not available, from a clinical point of view, in elderly patients these fractures are often considered “osteoporotic fractures.” The age-related osseous demineralization within the meta- and epiphyseal area of the distal humerus has been shown with preferential loss within the capitellar region.4 The elbow is a complex hinge joint that relies on a combination of bony articulations and soft tissue constraints to optimize stability and mobility.5 The ulnohumeral articulation is the essential factor for osseous stability and mobility in the flexion-extension plane. The olecranon blocks the anterior translation of the ulna with respect to the distal humerus while an intact coronoid process resists posterior subluxation of the proximal ulna in extension beyond 30 degrees or greater.6 The importance of the radial head as a secondary stabilizer to valgus stress and posterior translation is well recognized; however, the radial head also indirectly contributes to varus and posterolateral stability by creating tension in the lateral ligament complex.7 The distal humerus consists of diverging medial and lateral columns joined at their most distal aspect by the “tie arch,” consisting of the articular segment – the trochlea and the capitellum. The capitellum is the most distal portion of the lateral column; the nonarticular medial epicondyle is the most distal portion of the medial column. The trochlea is intermediate between the capitellum and the distal end of the medial column. The articular segment projects slightly anterior to the axis of the shaft at an angle of 40 degrees with the capitellum slightly further forward than the trochlea. The medial epicondyle is on the projected axis of the shaft, whereas the lateral epicondyle is projected slightly forward from the axis. Furthermore, soft tissue constraints play a major role in elbow stability. The anterior band of the ulnar collateral ligament acts as the major stabilizer to valgus stress.8 The major stabilizer to varus or rotatory stress is the lateral collateral ligament complex, including the lateral ulnar collateral ligament.9,10 The majority of elbow fractures in the elderly are the result of a fall from a standing height after a tripping or slipping incident.3 Fractures of the olecranon occur from direct or indirect trauma. A fall or blunt trauma on the posterior tip of the elbow may cause fracture directly. Indirect avulsion of the olecranon by forces generated within the triceps muscle may occur with eccentric contraction during a fall on a partially flexed elbow. In cases of severe force to the elbow, a fracture dislocation can occur with posterior displacement of the olecranon fragment and displacement of the distal ulnar fragment together with the head of the radius anterior to the humerus. Fractures of the distal humerus result from an axial load through the elbow with the joint flexed beyond 90 degrees. Cadaveric studies have shown that when the load is applied with the elbow at 90 degrees, an olecranon fracture is produced. Radial head fractures result from an axial load with maximum force transmission in full elbow extension with forearm pronation.11 In the elderly, restoration of the complex anatomy of the elbow is often complicated by poor bone quality and associated metaphyseal and epiphyseal comminution. As a result, adequate fracture fragment fixation and stable joint reconstruction are often difficult to achieve, but are central to effective care. The primary goal of definitive fracture management in elderly patients is early restoration of function and independence. The tolerance for posttraumatic elbow immobilization is very poor in elderly patients with a duration of immobilization longer than 15 days leading in a high percentage of cases to significant stiffness and loss of function.1 Therefore, the selected treatment should be prompt, definitive, and kept as simple as possible to minimize surgical time, blood loss, and physiologic stress. However, the presence of comorbid illnesses requires thorough evaluation before surgery. Although anatomic restoration is important for intraarticular fractures, in certain cases, a minor degree of incongruity may be preferred to prolonged immobilization. Metaphyseal and diaphyseal fractures are often best managed by attempts to primarily achieve stability rather than anatomic reduction.12 Failure of screw purchase in bone, not implant breakage, is the primary mechanism of failure of internal fixation in osteoporotic bone. Decreased bone mineral density correlates with the holding power of the screws and may result in poor screw purchase.13,14 For these reasons, fractures around the elbow in the elderly mandate a different algorithm for the surgical decision-making process and operative techniques compared with fractures in younger patients with superior bone quality and increased capacity for fracture repair. Fractures around the elbow in the elderly are best classified independently, but must be understood within the context of the overall injury. Associated ulna fractures can involve the coronoid process and/or the olecranon process. Regan and Morrey classified fractures of the coronoid process into three types, depending on the extent of involvement.15 Type I fractures are a small fleck of bone sheared from the coronoid during subluxation or dislocation. Type II fractures involve up to 50% of the coronoid process. Type III fractures involve more than 50% of the coronoid. Recently, O’Driscoll has added an additional fracture pattern (type IV) to describe the sagittal plane fracture of the coronoid involving the attachment of the anterior bundle of the medial collateral ligament.16 Colton’s classification of olecranon fractures reflects displacement and the anatomy of the fracture, thus providing guidance as to the most biomechanically appropriate type of fixation. Fractures are described as nondisplaced and stable if they are displaced less than 2 mm, and exhibit no change in position with gentle flexion to 90 degrees or with extension against gravity. Displaced fractures can be further divided into avulsion fractures, transverse or oblique fractures, isolated comminuted fractures, or fractures with associated dislocations.17 Radial head fractures are classified based on the modified Mason’s classification by Hotchkiss. Type I fractures represent nondisplaced or minimally displaced fractures (<2 mm) of the radial head or neck requiring no surgical intervention. Type II fractures are displaced fractures of the radial head or neck but can be fixed. Type III fractures are displaced radial head or neck fractures, but are not reconstructable. The Orthopaedic Trauma Association (OTA)/AO classification system is most commonly used to describe distal humerus fractures and divides them into type A, nonarticular; type B, partial articular; and type C, complete articular. Based on the position and orientation of the fracture line and degree of comminution additional levels are appended. Patients with a distal humeral, radial head, or proximal ulna fracture present with pain and swelling about the elbow. Those with displaced fractures usually have an obvious deformity, and attempted motion may elicit painful bony crepitus. The mechanism of injury as well as any associated neurovascular complications associated with the initial injury should be elicited from the patient. Thorough assessment for concurrent illnesses precipitating the injury (such as an arrhythmia) and a detailed account of comorbid conditions are important. Physical examination should begin with assessment of the condition of the soft tissues around the elbow. Extensive swelling, ecchymosis, and any abrasions or lacerations should be noted and may influence the timing of surgery or location of incisions. An assessment of range of motion (ROM) or strength of the elbow should not be vigorously pursued. There may be a palpable sulcus at the site of an olecranon fracture, accompanied by painful and limited ROM. An important sign to be elicited with isolated olecranon fractures is the inability to extend the elbow actively against gravity. Although it may be difficult to get the patient’s cooperation secondary to pain, this inability indicates discontinuity of the triceps mechanism. A careful neurovascular examination, especially of the ulnar nerve, is essential prior to any planned manipulation of the elbow. Plain radiographs in the anteroposterior, true lateral, and oblique projections are usually sufficient to provide enough information for an accurate diagnosis. Severe comminution with displacement and overlap of the fracture fragments can obscure thorough determination of the fracture pattern. Thus, radiographs need to be good quality, out of splint, and obtained while maintaining gentle longitudinal traction with inclusion of the elbow joint on the film. Nontraction in the splint radiographs is not as well suited for accurate diagnosis, for classifying the fracture, and for formal preoperative planning. Rarely does computed tomography (CT) of the elbow provide additional information that alters decision making and preoperative planning. Historically, distal humerus fractures have been difficult to treat with unpredictable outcomes prior to the 1960s.18 Nonoperative treatment, the “bag of bones” technique, was advocated by many authorities as the best treatment for fractures of the distal humerus, especially in elderly patients due primarily to the lack of adequate surgical techniques and implants. During the past few decades nonoperative treatment has been shown to result in poor outcomes with high rates of joint stiffness, malunion, or painful nonunion.1,19,20 Advances in the theory, techniques, and instrumentation for operative management of intraarticular fractures has made open reduction and internal fixation (ORIF) the treatment of choice for displaced intraarticular distal humerus fractures in adults. Disagreements remain on how to treat these fractures in elderly patients as stable fracture fixation and early initiation of therapy can be difficult. Current controversy remains regarding the indications for performing a primary total elbow arthroplasty for the treatment of comminuted fractures of the distal humerus in the elderly (see Chapter 13). The rationale for ORIF is the limited longevity of arthroplasty compared with successful primary osteosynthesis. In addition, infection or implant failure is more difficult to manage in the context of arthroplasty. The complete articular fractures (C-type) are the most commonly encountered in elderly patients. ORIF can be performed through several approaches such as the triceps-splitting approach, the posterior transolecranon approach, or the extensive triceps sparing approach.21 In open distal humeral fractures, the wound is most commonly posterior or posterolateral with an associated defect in the triceps from the protrusion of the humeral shaft. In this scenario a triceps-splitting approach has been shown to have several advantages compared with olecranon osteotomy.22 The plating construct that optimizes fracture fixation stiffness is two plates on separate distal humeral columns and in different planes.23 This is commonly performed with a medially positioned reconstruction plate and a small fragment compression plate on the posterolateral surface or an anatomical lateral buttress “J” plate. Alternatively, precontoured anatomical plates can be placed directly medially and laterally with screws directed into the opposite column and the distal fragments further stabilized by the compressive effect of the plates.24,25 The general principles are anatomic restoration of the articular surface, followed by restoration of joint shaft alignment, then stable fixation of the reduced distal fragment to the humeral shaft. Polymethylmethacrylate (PMMA) may be utilized to augment screw fixation proximally.26,27 The patient is placed in the lateral decubitus position with the arm at 90 degrees abduction and the elbow flexed at 90 degrees over a bolster. A midline posterior incision is made curving around the lateral tip of the olecranon. Full-thickness skin flaps are created laterally and medially with care taken to minimize soft tissue handling. The ulnar nerve is identified at the medial aspect of the triceps proximal to the injury and carefully exposed, including release of the cubital tunnel. A Penrose drain is placed around the nerve to assist in protection; however, traction is avoided. A midline split in the triceps muscle and tendon is created proximally and extended distally along the dorsal crest of the ulna. Meticulous sharp dissection is used to create full thickness flaps at the triceps insertion onto the ulna. Dissection is carried laterally and medially along the distal humerus to expose the lateral and medial column, respectively, taking care to protect the ulnar nerve medially and the radial nerve laterally. The fracture fragments are gently cleaned of clot and debris and the distal humeral articular surface is reassembled and stabilized with Kirschner wires (K-wires). The articular fragment is stabilized with a transverse lag screw or fully threaded position screws when there is intercondylar comminution or bone loss to avoid narrowing the trochlea. The lateral plate, usually a 3.5-mm compression plate or specially designed anatomic lateral buttress “J” plate, is applied along the straight lateral column. The medial plate, usually a 3.5-mm reconstruction plate or compression plate, is contoured to lie directly over the medial epicondyle or more posteriorly along the medial column respectively (Fig. 12–1). Figure 12–1 (A) Anteroposterior (AP) radiograph of a comminuted, intraarticular distal humerus fracture caused by a fall in an elderly patient. (B) AP radiograph following open reduction and internal fixation with a precontoured lateral J plate and a compression plate contoured to fit the medial column. Both plates “cradle” the distal fragments with good screw purchase distally. Precontoured anatomical plates are available and may be helpful to provide a lower profile implant on the medial side. In addition, angular fixed locking plates have been introduced with the potential advantage of improved stability and pull-out strength within the osteoporotic bone of the distal fragment.4,28 Regardless of implant choice, the distal placement of plates to “cradle” the distal fragments is imperative, thus relying on a combination of plate strength, placement of as many screws as possible in the distal fragment, and interdigitation of screws in the distal fragment to optimize stability.24 A portable radiograph should be obtained following fixation. The triceps is reattached to the olecranon using three #2 Ethibond sutures (Ethicon, Inc., Somerville, NJ) passed through bone in a horizontal mattress fashion. The remainder of the triceps is reapproximated using interrupted figure-eight sutures. The ulnar nerve is transposed anteriorly to a subcutaneous position and prevented from migrating posteriorly with a suture between the fascia and subcutaneous tissue. The medial intermuscular septum is released and the nerve is checked to ensure there is no tethering or pressure in its transposed location. Subcutaneous tissue and skin are then closed in layers. The subcutaneous location of the proximal ulna makes this area prone to fracture from a direct blow to the posterior surface of the elbow. This is a frequent mechanism suffered during falls in elderly patients and similar to distal humeral fractures can present a challenge because of associated comminution.
Anatomy of the Elbow
Epidemiology and Mechanisms of Injury
Goals of Fracture Management in the Elderly
Classification of Elbow Fracture
Patient Assessment
History
Clinical Examination
Radiographic Assessment
Treatment
Distal Humerus Fractures
Technique
Proximal Ulnar Fractures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree