Offset-V Osteotomy of the First Metatarsal Shaft in Hallux Abducto Valgus
Gary R. Bauer
Harold W. Vogler
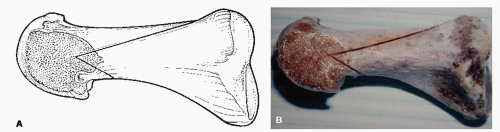
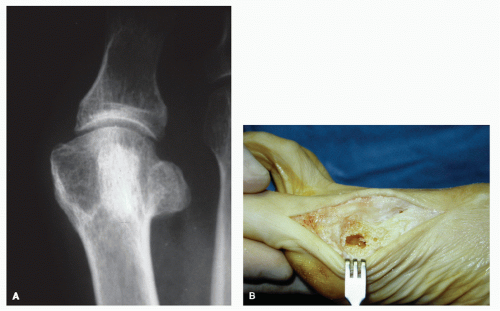
Shaft osteotomies may be employed in the repair of hallux abducto valgus (HAV) deformities in some patients as an alternative to proximal procedures. The offset-V osteotomy is one type of shaft osteotomy and represents a modification of the Ludloff procedure (1). The procedure was first performed by Vogler in 1983 (2,3 and 4). The apex of the osteotomy is located at the distal metaphyseal-diaphyseal junction of the first metatarsal (Fig. 29.1). This zone, the anatomic neck, is transitional bone, representing the junction between primarily cortical and cancellous bone. Compared with a base osteotomy, the procedure is performed at a more distal location with a shorter lever arm and allows protected weight-bearing ambulation in the immediate postoperative course. It has therefore been characterized as a “compromise osteotomy”(2). The procedure is useful in patients with cystic erosion of the metatarsal head that may make performance and stabilization of a capital metaphyseal type osteotomy difficult (Fig. 29.2).
The intrinsic stability of the offset-V osteotomy is conferred by its geometry, with long dorsal and short plantar legs. The procedure is versatile and allows for reduction of intermetatarsal (IM) angles up to 18 degrees and proximal articular set angle (PASA) deviation in excess of 40 degrees. The reduction of the IM angle is achieved through aggressive lateral translation of the distal fragment composed of the metatarsal head and at least one-half of the shaft segment or more as required. Once the composite metaphyseal capital and shaft segment disengages the medial cortical portion of the proximal metatarsal segment, the PASA can be swiveled out by impacting the medial metaphyseal segment within the medullary canal of the proximal shaft. Fibular sesamoidectomy should be cautiously considered in cases where the sesamoidal interface is arthritic or serves as a mechanical block in the IM space restraining the necessary amount of lateralization of the displaced distal bone segment required to achieve correction. The PASA must be normalized if the fibular sesamoid is removed as it will contribute to iatrogenic hallux varus deformity (Fig. 29.3).
TECHNIQUE
Due to the diaphyseal location of the osteotomy and the degree of distal segment displacement often required to achieve correction, surgical dissection is minimized to maintain the vascular supply to the osseous segments (5,6,7,8 and 9). The skin approach is through the classic dorsomedial linear incision (Fig. 29.4B). After incision of the superficial fascia, a limited dissection interval is developed between the superficial and deep fascia along the dorsomedial first metatarsal. The capsular incision is dorsomedial and can employ removal of a wedge of redundant capsular tissue at closure, often with oblique “load sutures” to help maintain rectus hallux alignment. The periosteal incision is extended onto medial cortical bone and continues proximally toward the base slightly above the midline of the shaft. The periosteum is carefully elevated medially along the shaft from the periosteal incision line and extended dorsally to view the exit site of the long upper wing of the osteotomy proximally, thereby avoiding injury to the extensor hallucis longus (EHL) tendon. Once raised, the periosteal-capsular plane can be extended distally exposing the metatarsal “transitional bone” and medial eminence (Fig. 29.4C). Care is taken to preserve the integrity of the capsular tissues for subsequent closure. This can be facilitated by initiating the dissection proximally with a sharp periosteal elevator, then taking down the medial collateral ligamentous complex from beneath the epicondyle of the metatarsal head. The plantar and dorsal capsular recesses are preserved to minimize postoperative adhesions that can restrict range of motion (Fig. 29.4C-H).
The lateral release, if required, is next accomplished. We employ a percutaneous approach just distal to the metatarsophalangeal joint (MTPJ) with care to preserve the lateral metaphyseal vascular plexus. A “vertical puncture dissection” interval is developed between the sling component of the extensor hood and the subcutaneous tissue plane. Two Senn retractors can facilitate exposure with the rake end of one retracting the EHL medially and the deep end of the other protecting and retracting the contained subcutaneous neurovascular elements laterally (Fig. 29.4D). Distal traction on the hallux defines a puckering of the joint capsule that is entered with a scalpel blade delivered deeply hugging the flare of the proximal phalangeal base as the plantar lateral capsular tissues are released including the extensor sling, collateral ligament, combined adductor hallucis tendon, and, in severe deformity, the lateral head of the flexor hallucis brevis tendon. This maneuver can be facilitated by applying a simultaneous adductory force to the great toe tensioning the tissues. A small curved hemostat is then placed within this capsular rent directed proximally beneath the vertical sesamoidal ligament and just above the fibular sesamoid. The ligament is tensioned and released with a scalpel from inside out. As noted earlier, if the fibular sesamoid is pathologically enlarged, arthritic, or offers an obstruction to lateralization of the distal fragment, it can be removed.
Attention is now directed to the medial capital fragment. The phalanx is subluxed laterally and the dorsal capsular fold is retracted to directly visualize the PASA and evaluate any articular damage. The medial eminence is resected orthogonally to the
PASA deviation with preservation of all effective articular cartilage (Fig. 29.4E-H). This is important, along with minimal initial resection of the eminence, to avoid scalloping of the medial metatarsal contour once the PASA swivel is accomplished. Even in severe hallux valgus deformity, the eminence resection is often minimal, which has prompted some surgeons to forgo opening the medial capsular structures in shaft osteotomies that address PASA correction, thus reducing capsular adhesions. A 0.045-inch Kirschner wire (K-wire) is positioned at the anticipated apex of the offset-V osteotomy as an axis guide and is oriented to accomplish the desired displacement plane of the distal fragment (Fig. 29.4I). It is important to recognize that an axis guide pin that is directed plantarly as it passes from medial to lateral creates some plantarflexion of the capital fragment with IM correction; however, this will result in some elevatus of the capital fragment as the PASA is swiveled out. Factors that influence pin orientation include relative length of the first metatarsal, metatarsus primus elevatus, sub-second and third metatarsalgia, and PASA deviation. Occasionally, a Cotton open wedge medial cuneiform osteotomy can be added as an adjunctive procedure to help depress the first metatarsal and restore length when required.
PASA deviation with preservation of all effective articular cartilage (Fig. 29.4E-H). This is important, along with minimal initial resection of the eminence, to avoid scalloping of the medial metatarsal contour once the PASA swivel is accomplished. Even in severe hallux valgus deformity, the eminence resection is often minimal, which has prompted some surgeons to forgo opening the medial capsular structures in shaft osteotomies that address PASA correction, thus reducing capsular adhesions. A 0.045-inch Kirschner wire (K-wire) is positioned at the anticipated apex of the offset-V osteotomy as an axis guide and is oriented to accomplish the desired displacement plane of the distal fragment (Fig. 29.4I). It is important to recognize that an axis guide pin that is directed plantarly as it passes from medial to lateral creates some plantarflexion of the capital fragment with IM correction; however, this will result in some elevatus of the capital fragment as the PASA is swiveled out. Factors that influence pin orientation include relative length of the first metatarsal, metatarsus primus elevatus, sub-second and third metatarsalgia, and PASA deviation. Occasionally, a Cotton open wedge medial cuneiform osteotomy can be added as an adjunctive procedure to help depress the first metatarsal and restore length when required.
The geometry of the offset-V osteotomy varies depending on the size and shape of the metatarsal and the magnitude of the deformity. The typical divergence of the wings of the osteotomy is 40 to 45 degrees. The length of the dorsal wing depends on the overall length and width of the metatarsal and the degree of PASA to be addressed, but it usually extends 50% to 75% of the length of the bone. Significant PASA swivel of the capital fragment requires a shorter dorsal cut to prevent the juxtaposition of the proximal wing against the second metatarsal (Fig. 29.5).
 Figure 29.3 A: Preoperative radiograph demonstrates significant HAV deformity with hypertrophy of fibular sesamoid that mechanically blocked lateralization of the capital fragment. B: Postoperative weight-bearing radiograph demonstrates absence of fibular sesamoid with rectified IM and PASA. C: Failure to rectify PASA coupled with fibular sesamoidectomy contributed to hallux varus.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|