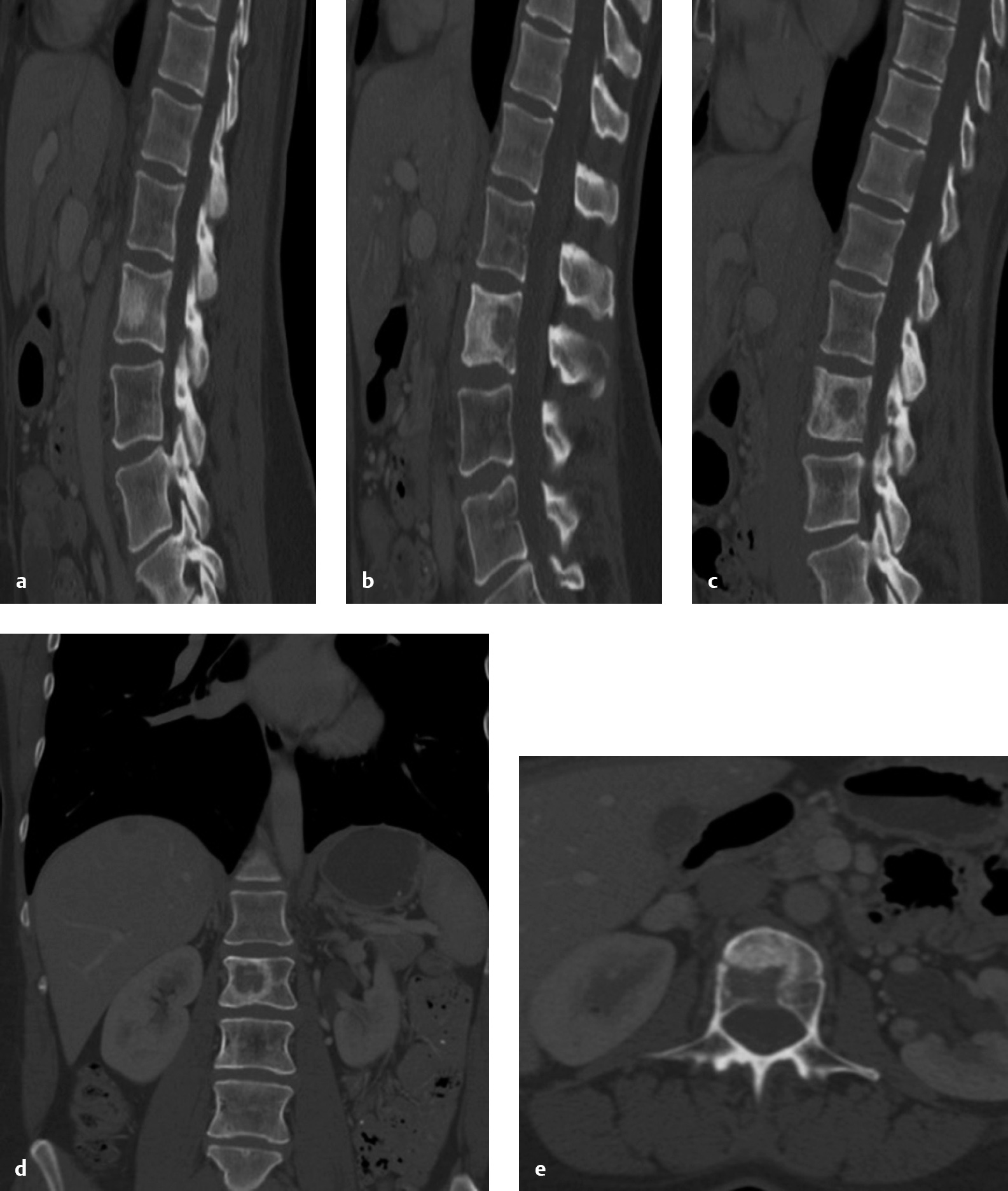
2 Restoration or maintenance of spinal stability is an important objective in the surgical treatment of spinal metastasis, but is often neglected in settings of neurologic compromise. Indeed, a prospective randomized trial has demonstrated the superiority of surgery and radiation therapy compared to radiation therapy alone in the management of high-grade spinal cord compression for solid tumors.1 Spinal instability is a common and distinct indication for surgery or vertebral augmentation with vertebroplasty or kyphoplasty.2 However, it has not been studied as rigorously as spinal cord compression. This reflects the controversy that exists regarding tumor-related instability. The biomechanical and clinical literature in this area is remarkably limited.3 Prior to the Spinal Instability Neoplastic Score, there were few clinical criteria published, and none had been tested for reliability or validity. The lack of standardized criteria led to significant variation with regard to diagnosis and treatment indications. In essence if the problem was not clearly defined, it was very difficult to study. The concept of spinal instability, however, remains a critical and essential component in the surgical decision-making process. Most often, spine surgeons rely on clinical experience to determine if instability is present. Although challenging for the spine surgeon, the diagnosis of instability is even more difficult for the nonsurgeon (radiologist, oncologist), potentially leading to inappropriate referrals or patients with instability being under treated, risking pain, deformity, or neurologic deterioration. This chapter reviews some of the principles of biomechanics as they relate to patterns of instability and deformity that occur in neoplastic disease, describes and applies the SINS in illustrative cases, and discusses the unique anatomic and biomechanical features of the different regions of the spine and options for management. Unlike the appendicular skeleton, the spine presents a very complex environment in which to judge tumor-related instability. Metastatic cancer alters both the material and geometric properties of the bone—the two entities that form the structural property rigidity. Although these properties determine the resistance to axial bending and twisting loads in bone, the “bone” or vertebra’s resistance to load in the spine is unique and significantly influenced by the region and adjacent anatomy. Indeed, there can be fracture or collapse in the spine, but no clinical symptoms, deformity, or fracture progression. The infinite complexity has led to a simpler approach in trying to define and predict spinal in stability in the setting of metastatic disease. The Spine Oncology Study Group (SOSG) defines spine instability as loss of spinal integrity as a result of a neoplastic process that is associated with movement-related pain, symptomatic or progressive deformity, or neural compromise under physiological loads.4 Tumor-related instability is very distinct from high-energy traumatic injuries in the pattern of bony and ligamentous involvement, neurologic manifestations, and bone quality. In addition, the ability of the spine to heal is compromised by the tumor, systemic therapies, irradiation, and the general biological compromise of these patients.5 Disease that involves the cancellous core of the vertebral body with preservation of the cortical bony support may not result in instability. Taneichi et al6 analyzed radiological and clinical data from patients with thoracic and lumbar metastases and created a multivariate logistic regression model to identify the probability of collapse under various states of tumor involvement. They found that in the thoracic spine, destruction of the costovertebral joint was a more important risk factor for collapse than the size of the metastatic lesion within the vertebral body, presumably related to loss of stiffness and strength normally provided by the rib cage. In the thoracolumbar and lumbar spine, the most important factor for collapse was the size of the vertebral body defect. Involvement of the pedicle had a much greater influence on vertebral collapse compared with the thoracic spine. Other studies have suggested that bone mineral density is more important than defect size in predicting fracture threshold. Anterior compressive forces are balanced by a posterior system composed of muscles and ligaments working under tension. The well-vascularized vertebral bodies are the most common sites of tumor involvement, with posterior vertebral elements being much less frequently affected. In general, the dorsal ligamentous complex is less commonly disrupted by neoplasm as compared with high-velocity trauma.5 Iatrogenic destruction of posterior elements by laminectomy is probably more common than disruption by the tumor itself. Destruction of the facet joints by tumor is also rarer than in trauma, but when it is present, it may result in significant translational or rotational deformity. The biomechanical effects of spinal metastases are poorly defined. As a result, there are no standards for predicting the risk of pathological fracture, even when lesions have been identified and characterized with modern imaging studies. Theoretically, vertebral body collapse may be prevented by radiation therapy or systemic therapies if the tumor is sensitive to one of those treatments and its growth (and therefore lytic destruction of the vertebra) can be arrested. Once the tumor reaches a critical size, which may be defined as “impending collapse,” only surgical prophylactic stabilization (e.g., percutaneous cement, pedicle screws) can prevent fracture. Unfortunately, a reliable method to predict impending collapse does not exist due to the regional biomechanical and anatomic issues. Therefore, treatment of instability should generally be on the basis of actual clinical instability rather than asymptomatic or relatively asymptomatic radiological findings that imply the potential for instability in the future. In the SINS classification system, tumor-related instability is assessed by adding together six individual component scores: spine location, pain, lesion bone quality, radiographic alignment, vertebral body collapse, and posterolateral involvement of the spinal elements (see Table 1.1). Each component of SINS has demonstrated clinically acceptable reliability.7 The minimum score is 0 and the maximum is 18. Total SINS scores have near-perfect inter-and intraobserver reliability when collapsed into three clinically relevant assessments of tumor-related instability, which can be described as stability (0–6), indeterminate instability (potentially unstable) (7–12), and instability (13–18). Surgical consultation is recommended for patients with SINS scores ≥ 7. Examples of scoring are presented in Figs. 2.1, 2.2, and 2.3. Content and face validity of the SINS was facilitated by integrating the best evidence provided by two systematic reviews with expert consensus from members of the SOSG.4 At the time of this writing, there are no prospective studies that have assessed SINS. However, a retrospective validity analysis found that the false-negative rate was low (4.3%), and all of these type II errors were due to distinguishing stable from potentially unstable cases (not stable vs unstable).7 Assigning a numerical grade to instability (SINS 0–18) is attractive because it recognizes that, unlike in trauma, spinal stability due to tumor is not lost suddenly in an “all-or-none” fashion. Instead, it is gradual process that at a certain point results in pathological fracture. By being able to reliably define the severity of instability we may come closer to understanding the indications for less invasive forms of stabilization such as vertebroplasty or kyphoplasty. We propose that patients with intermediate grades of instability (SINS 7–12) are more likely to be appropriate candidates for percutaneous cement, whereas those with higher scores may be better treated with spinal instrumentation.8 Vertebral augmentation is particularly useful in patients with limited life expectancy, patients who are too medically frail to have open surgery, and patients with very poor bone quality (e.g., myeloma bone disease).9 Metastasis in this region rarely cause myelopathy because the upper cervical canal is large, and because tumors in this region typically present with severe mechanical neck pain before they become large enough to significantly compress the spinal cord. Therefore, ventral tumor resection (via a transoral or extraoral approach) is rarely indicated, and our surgical management strategy has focused on posterior spinal stabilization.10 We favor occipitocervical fixation over short-segment approaches because it protects the patient against the potential loss of stability due to progression of the destructive process. Our goal is to obtain a durable construct so that the use of any cumbersome and poorly tolerated external orthoses (e.g., rigid collar or halo vest) can be avoided. From C3 through C6, corpectomy reconstructed with a cage and plate is the most common approach. A combined anterior/posterior stabilization is often necessary for multilevel disease, circumferential tumor involvement, severe instability/deformity, and poor bone quality. Supplemental posterior stabilization is often required at the C7/T1 junction.11 Anterior approaches are not feasible in most patients from T2 to T5, due to the great vessels and the heart. Posterolateral approaches (costotransversectomy or lateral extracavitary approach) are recommended for this region, and are also increasingly popular from T6 through L5 (as compared with anterior approaches), because they allow removal of the tumor and the application of spinal instrumentation as a single-stage operation.12 Regardless of the approach used, the vertebral body may be reconstructed with various materials, including allograft bone, polymethylmethacrylate (PMMA), or metal cages. The latter include distractible or telescoping varieties. Polymethylmethacrylate is biologically compatible and very stable in compression, but usually requires anchoring with Steinmann pins or a chest tube. If vertebrectomy has been performed via an anterior approach, anterior column reconstruction and stabilization with a plate without supplementary posterior stabilization may be sufficient, except in certain circumstances: significant kyphosis or deformity, such as translation; thoracolumbar junction zone; significant adjacent chest wall resection (e.g., Pancoast tumor or locally invasive sarcoma); vertebrectomy spanning two or more levels; vertebrectomy caudal to L4 (anterior fixation devices are difficult to apply in this region); and poor bone quality.13 Fig. 2.1a–e Computed tomography (CT) images of (a) select left parasagittal view, (b) select midline sagittal view, (c) select right parasagittal view, (d) representative coronal view, and (e) axial view at L2 of a 42-year-old woman with known metastatic breast cancer who had an asymptomatic L2 lesion identified as an incidental finding on CT imaging. She denies any back pain. The Spine Instability Neoplastic Score (SINS) is calculated as follows: mobile spine location (L2), 2 points; pain-free lesion, 0 points; mixed lytic/blastic lesion, 1 point; normal spinal alignment, 0 points; no vertebral body collapse but > 50% body involvement, 1 point; no posterolateral spinal element involvement, 0 points. Total SINS = 2 + 0 + 1 + 0 + 1 + 0 = 4 (stable lesion).
Neoplastic Spinal Instability
 Introduction
Introduction
 Principles
Principles
Definition of Tumor-Related Spine Instability
Basic Biomechanical Principles in Spine Tumors Versus Trauma
Principle 1: Load Sharing
Principle 2: Tension Band
Impending Collapse
Spinal Instability Neoplastic Score
When Is Vertebroplasty or Kyphoplasty Sufficient for Stabilization?
Treatment of Instability by Spinal Region
Craniovertebral Junction
Subaxial Cervical Spine
Thoracic and Lumbar Spine
Neoplastic Spinal Instability
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree