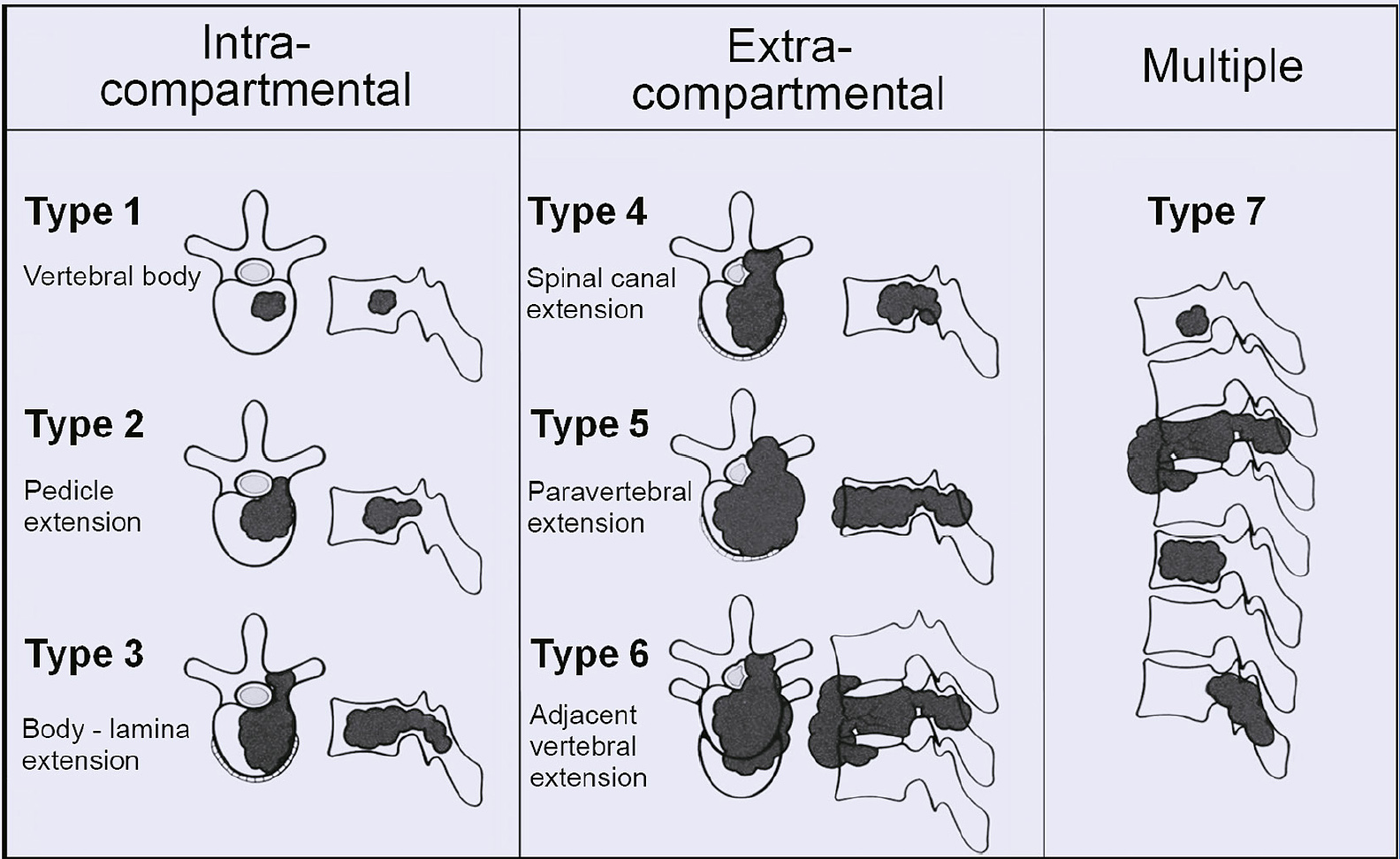
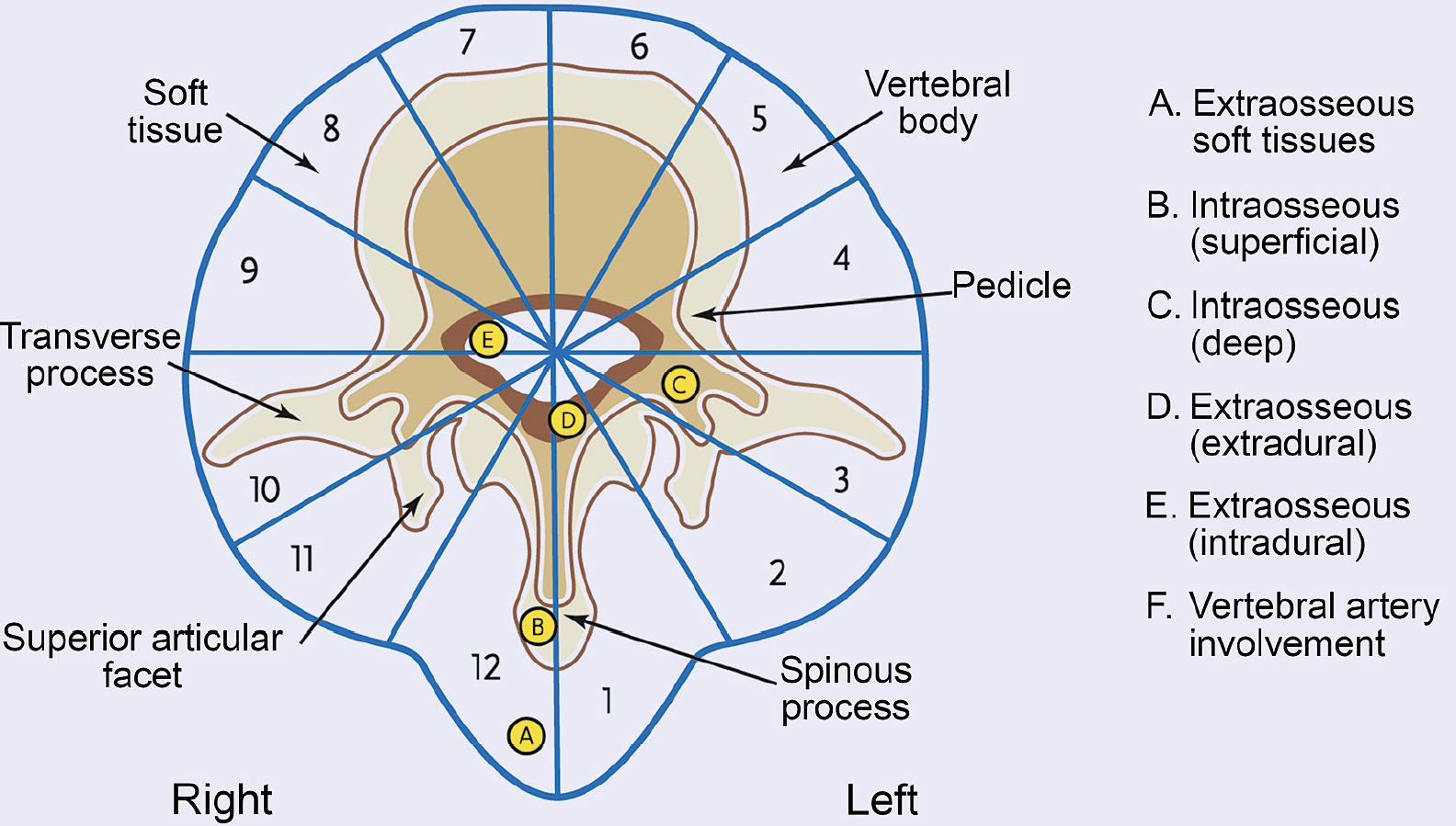
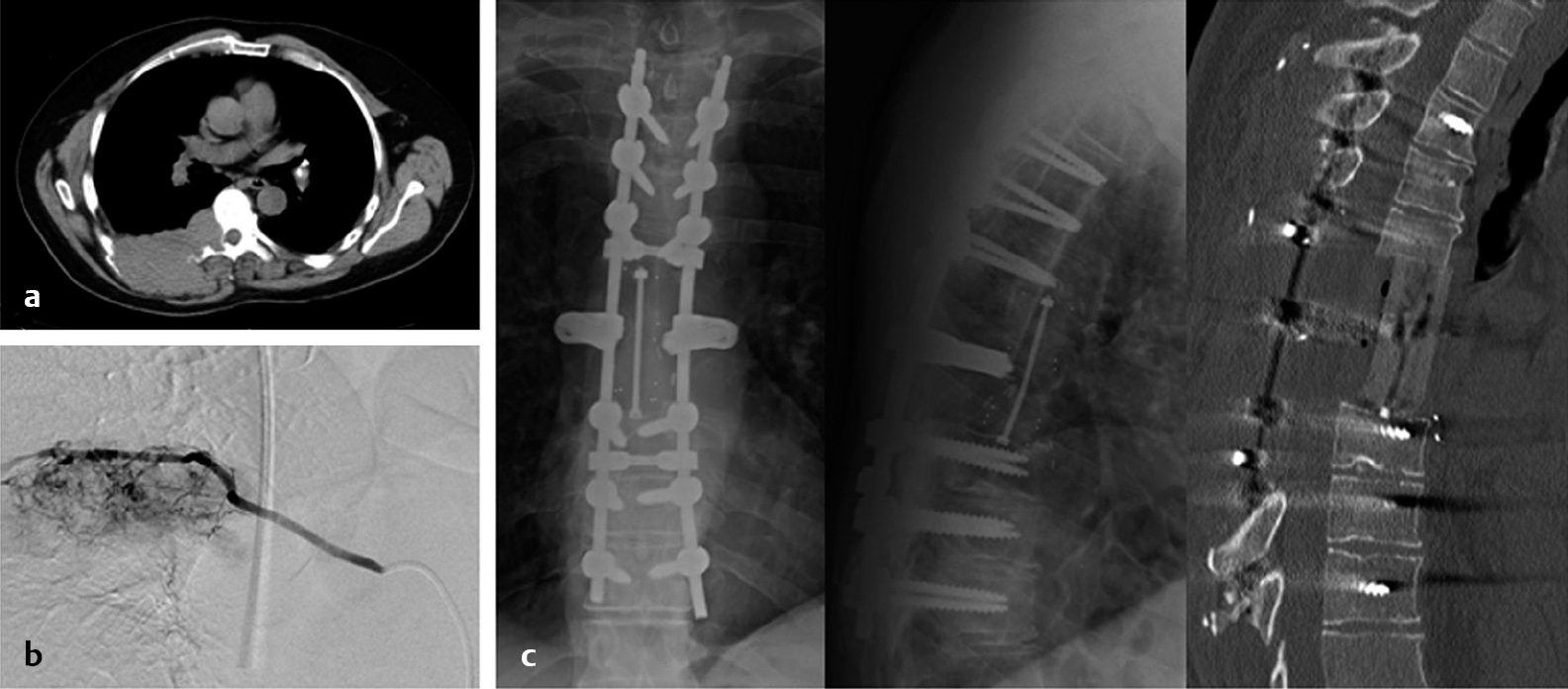
4 The principles of primary musculoskeletal tumor excision were thoroughly detailed by William Enneking et al.1 Although treatment concepts applicable to primary and metastatic tumors differ, the Enneking system elucidates the concept of surgical margin and may provide the historic context for the development of metastasis-specific surgical concepts. The Enneking system recommends radical or wide margin en bloc resection in cases of primary high-grade malignant tumors. The goal of en bloc resection is to remove the tumor in one piece without entering the margin. Radical margin surgery requires the excision of the entire anatomic compartment that harbors the tumor. Wide margin resection preserves normal tissue around the entire tumor, whereas a marginal margin resection is carried through the reactive zone of the tumor. The residual reactive tissue after a marginal margin surgery may contain “satellite” tumor cells and both marginal and wide margin dissection cannot eliminate the risk of residual skip lesions. Thus, in the absence of radical margin, Enneking recommended adjuvant therapy in cases of high-grade malignant tumors in order to treat the skip lesions and minimize the risk of recurrence.1,2 The complex anatomy of the surrounding structures and the central location of the spinal cord within the spinal column present unique challenges to the application of the Enneking principles in the treatment of spinal tumors. The majority of spinal metastatic solid tumors originate from the osseous structures of the vertebrae, with the dorsal vertebral body being the most common tumor site.3 The discussion of a single vertebra as an individual surgical compartment requires clear understanding of the surrounding tissues that may prevent tumor spread and that are the most likely routes of tumor spread outside of the vertebra.4 The barrier tissues surrounding the vertebra include ligaments (anterior longitudinal ligament [ALL], posterior longitudinal ligament [PLL], ligamentum flavum, interspinous ligament, and supraspinous ligament), periosteum (lateral to the vertebral body, surrounding the spinal canal, and dorsal and lateral to the lamina and spinous process), and intervertebral disk (cartilaginous end plate, annulus fibrosus, and nucleus pulposus). Examination of en bloc surgical specimens demonstrated the highest degree of tumor invasion in the PLL and lateral periosteum.3 The ALL, ligamentum flavum, and intervertebral disk appeared to act as good barriers to tumor penetration. Further analysis of tumor spread pattern showed that the lateral PLL was the most likely route of vertical extension in metastatic tumors, followed by the central PLL. The strong longitudinal central attachment of the PLL compared with the thinner ligament laterally provides an explanation for this spread pattern. The presence of a fibrous reactive membrane was noted in several specimens even after extension outside of these anatomic barriers. The presence of such a capsule implies the possibility of a marginal margin resection according to the Enneking principles. However, the high likelihood of satellite microscopic disease outside of the capsule has to be considered in cases of malignant tumors, which includes all metastases. In 1997, two systems aimed at translating the resection principles of the Enneking system into the spine-specific context were proposed. The Surgical Classification of the Vertebral Tumors developed by Tomita et al5 (Fig. 4.1) and applicable to metastases, divides the tumors into intracompartmental (confined to the vertebra), extracompartmental (extraosseous extension), and multifocal skip lesions, and classifies them also based on the extent of dorsal extension along the vertebra (vertebral body only, extension into pedicle and then lamina). The Weinstein, Boriani, and Biagini (WBB) Surgical Staging System, applicable to primary spinal tumors, divides the axial plane of the vertebral body into 12 radial zones, similar to a clock face, and into five concentric zones, thereby providing a systematic description of the extent and location of the tumor around the spinal cord and its extraosseous extension6 (Fig. 4.2). Both systems were developed in order to provide a common language when describing the location and extent of the tumor and to determine what type of surgical margin would be feasible. Although a radical margin, or resection of the entire spinal compartment, is not feasible, certain tumors may be amenable to wide or marginal margin resection. Vertebrectomy, sagittal resection, and posterior arch resection represent the three main methods of en bloc resection in the spine.6 Tumors centered in the vertebral body may be removed en bloc by carrying out a vertebrectomy or excision of the entire vertebral body. Tumors arising from the pedicle, transverse process, or eccentrically located in the vertebral body may be removed en bloc using sagittal osteotomy through the posterior elements and the vertebral body. Tumors arising from posterior elements may be removed en bloc by sectioning the pedicles and removing the posterior arch in one piece.2 Any method of total spondylectomy must include the opening of the spinal canal in order to permit safe passage of the spinal cord through the opening. Therefore, in cases of a tumor that begins to encircle the spinal cord, deliberate transgression of the tumor is likely required. Fig. 4.1 Tomita classification of vertebral tumors. (From Kawahara N, Tomita K, Murakami H, Demura S. Total en bloc spondylectomy for spinal tumors: surgical techniques and related basic background. Orthop Clin North Am 2009;40:47–63. Reproduced with permission from Elsevier.) Fig. 4.2 Weinstein-Boriani-Biagini surgical staging system. (From Boriani S, Weinstein JN, Biagini R. Primary bone tumors of the spine. Terminology and surgical staging. Spine 1997;22:1036–1044. Reproduced with permission from Wolters Kluwer Health.) Prior to en bloc resection of spinal tumors, embolization may be undertaken in order to decrease intraoperative blood loss. Kawahara et al7 recommend embolization of bilateral segmental arteries at the excision levels in order to facilitate the separation of the artery from the vertebral body and along with the cephalad and caudal levels. Such embolization may reduce blood loss in cases where intentional or unintentional tumor transgression takes place. Embolization of three levels significantly reduced the intraoperative blood loss compared with embolization of only the level with tumor invasion. Preoperative embolization also helps to define segmental arteries that anastomose with the anterior spinal artery, including the artery of Adamkiewicz.8 Although sacrifice of the artery of Adamkiewicz is generally avoided, Murakami et al9 reported a series of 15 total spondylectomies where the artery of Adam-kiewicz was ligated during tumor resection without neurologic deterioration. The location of the tumor dictates the approach. En bloc resection can be carried out using a single posterior or anterior approach, or a combination of the posterior and anterior approaches. The combined approaches may be performed on the same day or as two separate operations. The extent of tumor invasion of the surrounding structures and the level and the extent of required spinal reconstruction determine the optimal combination of approaches. Generally, a combination of anterior and posterior approaches is required in order to perform an en bloc resection of lumbar tumors. When invasion of the major vessels, segmental arteries, and thoracic or abdominal organs is suspected, an anterior dissection may be performed during the first stage of the operation, followed by the posterior approach for the en bloc excision. The order of the anterior and posterior approaches has to be tailored to specific level and tumor anatomy and determined individually for each case. The posterior approach should expose two or three levels above and below the tumor. Laterally, approximately 4 to 5 cm of the bilateral ribs or the entire transverse process must be exposed at the levels involved by tumor and at least one level adjacent to the tumor. Superiorly the spinous process and the inferior articulating processes of the level above the tumor and inferiorly the ligamentous attachment of the spinous process and the superior articulating processes of the level below the tumor must be sectioned in order to release the posterior elements of tumor. In the thoracic spine, the 3- to 4-cm segments of the ribs distal to the costovertebral junction are removed in order to expose the pedicles of the tumor level. The neurovascular bundle running along the inferior edge of the rib is identified and separated or sacrificed prior to removal of the rib. Periosteal dissection is carried out along the pars interarticularis and pedicles in order to allow a safe osteotomy through the pedicles. Posterolateral pedicle fixation is carried out two or three levels above the excision. Only one rod is placed at this time, on the side opposite the direction of the rotation of the final en bloc specimen. Only temporary tightening of the screw rod construct should be carried out because distraction and compression maneuvers may be required. The osteotomy may be carried out using a thread-wire saw, an osteotome, or a drill. Once the pedicles are sectioned and the posterior elements are released from the levels above and below the tumor, the pedicle, transverse process, lamina, and spinous process complex of the levels involved by tumor may be removed in one piece. Identification of the segmental artery at the level of the vertebrectomy is of paramount importance. This artery is usually located lateral to the pedicle. The spinal branch of the segmental artery must be identified and ligated. In the thoracic spine, the nerve roots can generally be safely sacrificed below T1, which eliminates the risk of evulsion and facilitates the circumferential exposure and dissection. The surrounding pleura or iliopsoas muscle are bluntly dissected off the vertebral body, with care being taken to control the segmental artery at all times. The bilateral segmental arteries are followed to the aorta, which is carefully dissected off the left ventral surface of the vertebral body. The segmental arteries are clipped, coagulated, and sectioned in order to prevent evulsion of these arteries off the aorta. This dissection is completed in the cephalocaudal direction until all of the vertebral bodies that will be removed en bloc are separated from the surrounding lateral and ventral structures. Malleable retractors are used to maintain the separation and to protect the paraspinal structures. The vertebrae involved by tumor are generally separated from the remaining spinal column at the cephalad and caudal disk spaces. This can be carried out using a thread-wire saw or osteotomes.7,8 Various devices have been developed to facilitate this step. If a lateral direction of the cut is chosen, the surgeon must remember the concave shape of the dorsal surface of the vertebral body and create a safe channel for the saw prior to stretching it in order to avoid dural damage. The anterior and posterior longitudinal ligaments must also be sectioned in order to complete the release of the tumor, and the epidural venous plexus dorsal to the PLL must be fully coagulated in order to minimize the bleeding. Finally, the ventral dural surface must be separated from the vertebrectomy segment and Hoffman’s ligaments must be carefully sectioned. This can be carried out through blunt dissection using angled dissectors. At this point the vertebrectomy specimen is entirely mobilized and can be rotated around the spinal cord in order to complete the removal. Anterior column reconstruction is completed using a distractible or mesh titanium cage; alternatively, a distractible polyetheretherketone (PEEK) cage may be used. Axial loading of the anterior construct is ensured with compression of the posterolateral instrumentation. Autologous rib graft may be used to maximize the chances of osseous fusion during the reconstruction of the anterior and posterior columns. Irrigation of the resection cavity with distilled water and high-concentration cisplatinum can be performed to locally treat microscopic residual tumor. If anterior release of the tumor from vital thoracic or abdominal structures is required prior to the posterior approach, a thoracotomy may be used or a retroperitoneal approach to L2-L4 and a transperitoneal approach to the L5 level. An approach surgeon may be consulted, depending on the preference and experience of the surgeon and institutional practice. These procedures can be carried out using traditional open techniques or a mini-open or thoracoscopic approach.10 Thoracoscopy provides a minimally invasive alternative to ventral ligation of the segmental arteries and does not require a postoperative chest tube.11 The combined posterior-anterior approach may be carried out with the patient placed in the lateral position.12 En bloc excision of spinal metastases provides excellent neurologic outcomes and reliable local tumor control (Fig. 4.3), with only a few recurrences reported (Table 4.1). Murakami et al13 examined the neurologic function after thoracic en bloc tumor resection in 79 patients, with 53 of these patients undergoing surgery for metastatic tumors. Within the entire group, 46 patients had a neurologic deficit, and 25 of them experienced an improvement of at least one Frankel grade, whereas the remaining patients experienced an improvement in neurologic symptoms even if it did not translate into a full Frankel grade improvement. Tomita et al5 reported no recurrences in 20 patients who underwent en bloc resection for a variety of metastatic tumor histologies. The median follow-up in this group was 9 months, with nine patients alive at the completion of the analysis and a range of 8- to 30-month follow-up among survivors. Fifteen metastatic tumors, mostly metastatic renal cell carcinoma, were resected using a simultaneous anterior-posterior approach with the patient placed in the lateral position. No recurrences were observed after a median follow-up of 6 months, with two patients surviving over 2 years without local recurrence. Sakaura et al14 reported the outcome of en bloc resection in 12 patients, mostly with metastatic breast, thyroid, and renal cell carcinoma metastases. The overall survival was 58%, with median follow-up of 61 months in survivors and 23 months in patients who died. The authors observed two local recurrences 25 months after surgery, both in patients with tumors with paraspinal extension. Eight patients had tumor progression at other sites at a median of 5 months after surgery. Fig. 4.3a–c Case example of a 58-year-old man with (a) solitary renal metastasis to the T6 and T7 levels with chest wall invasion on the right. (b) The patient underwent preoperative embolization of the tumor followed by T6 and T7 spondylectomy with right-sided chest wall resection for en bloc tumor resection. (c) The stabilization was carried out using pedicle fixation three levels above and below the tumor, and carbon fiber cage and allograft reconstruction of the anterior column. Adjuvant conventional external beam radiation was administered. His most recent follow-up, 3 years and 3 months after surgery, shows no evidence of local recurrence and no evidence of systemic disease. (Courtesy of Jean-Paul Wolinsky, MD, Johns Hopkins University.)
En Bloc Resection in the Treatment of Spinal Metastases: Technique and Indications
 Introduction
Introduction
 Surgical Technique
Surgical Technique
 Local Control
Local Control
En Bloc Resection in the Treatment of Spinal Metastases: Technique and Indications
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree