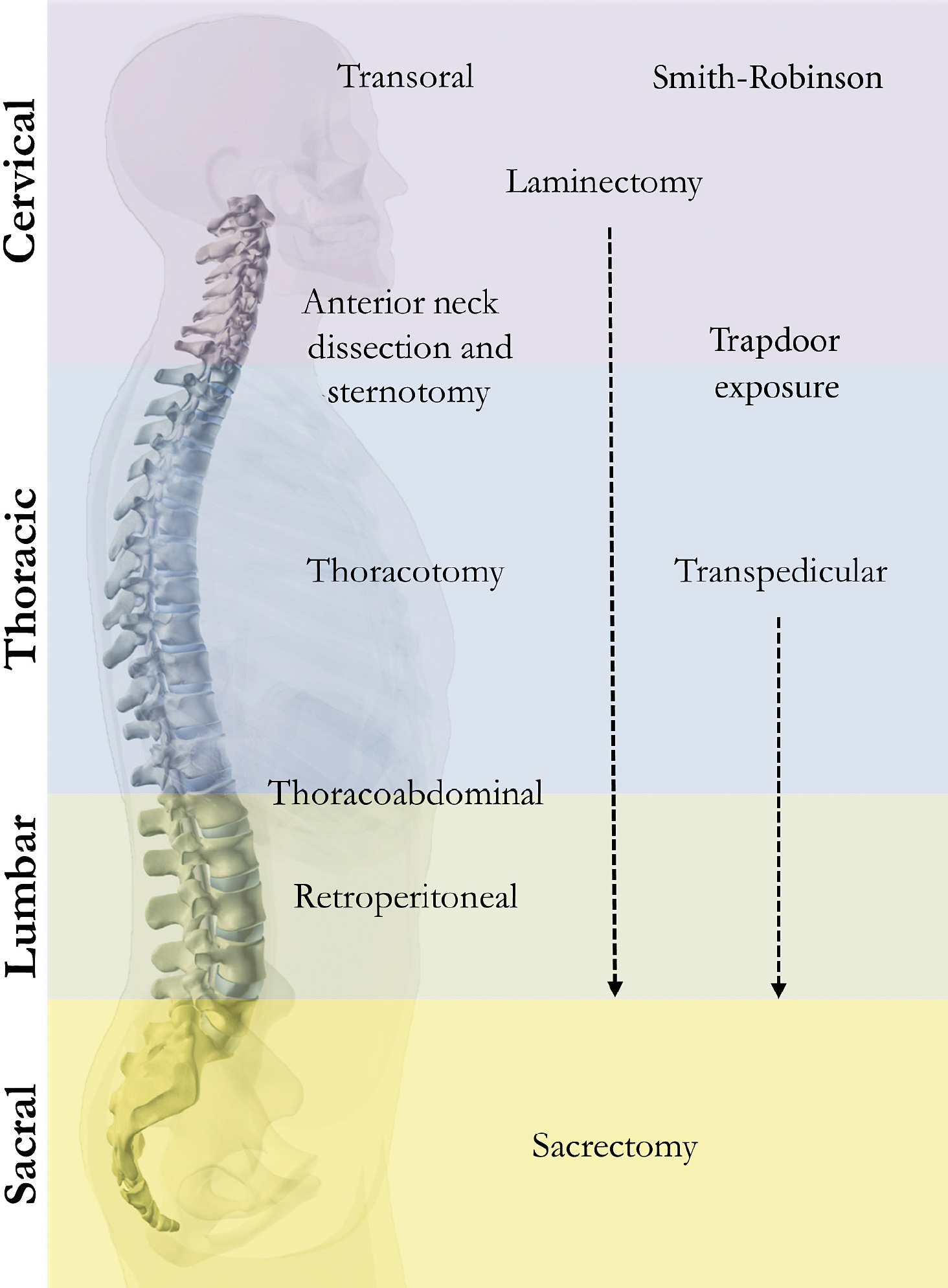
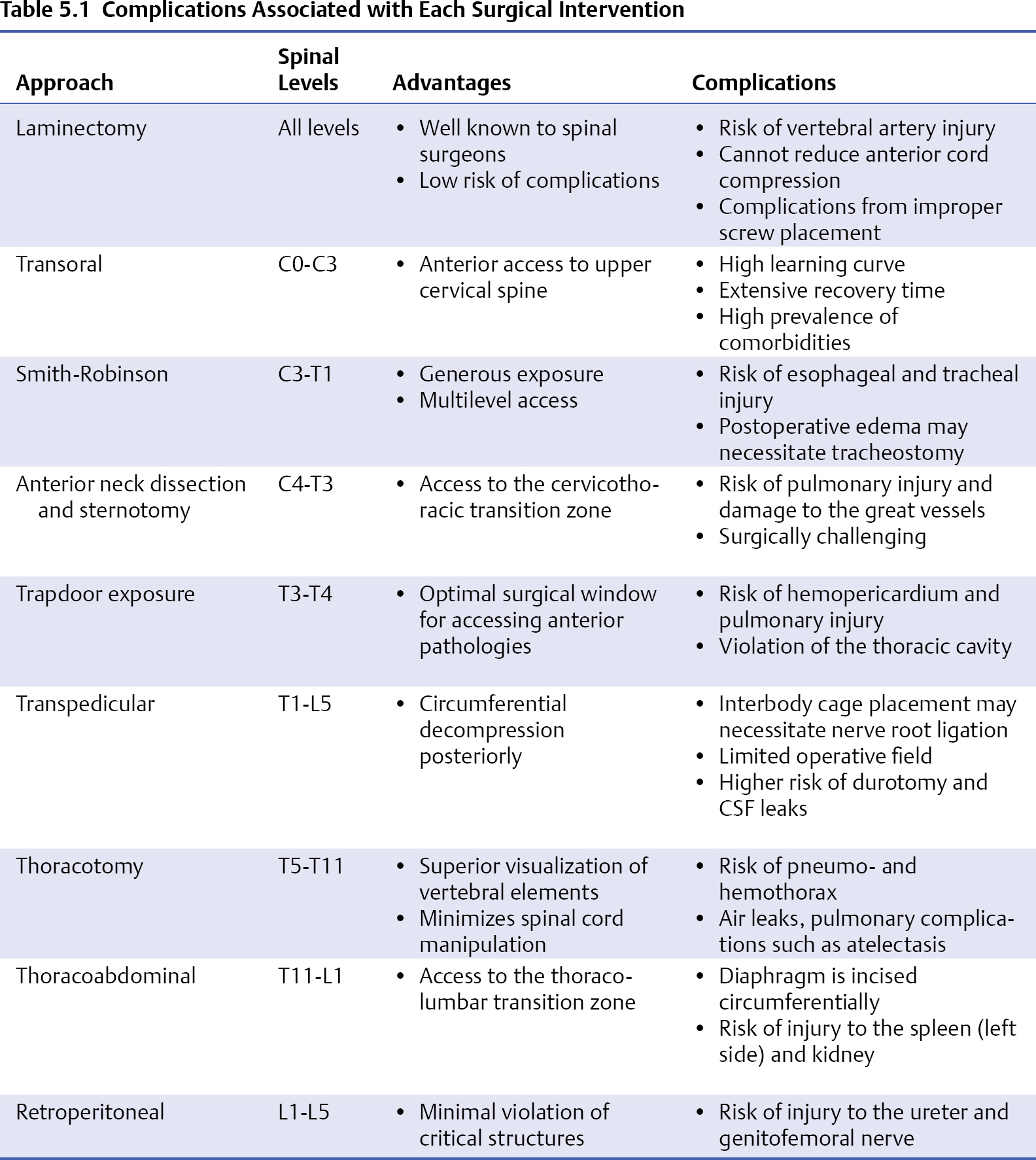
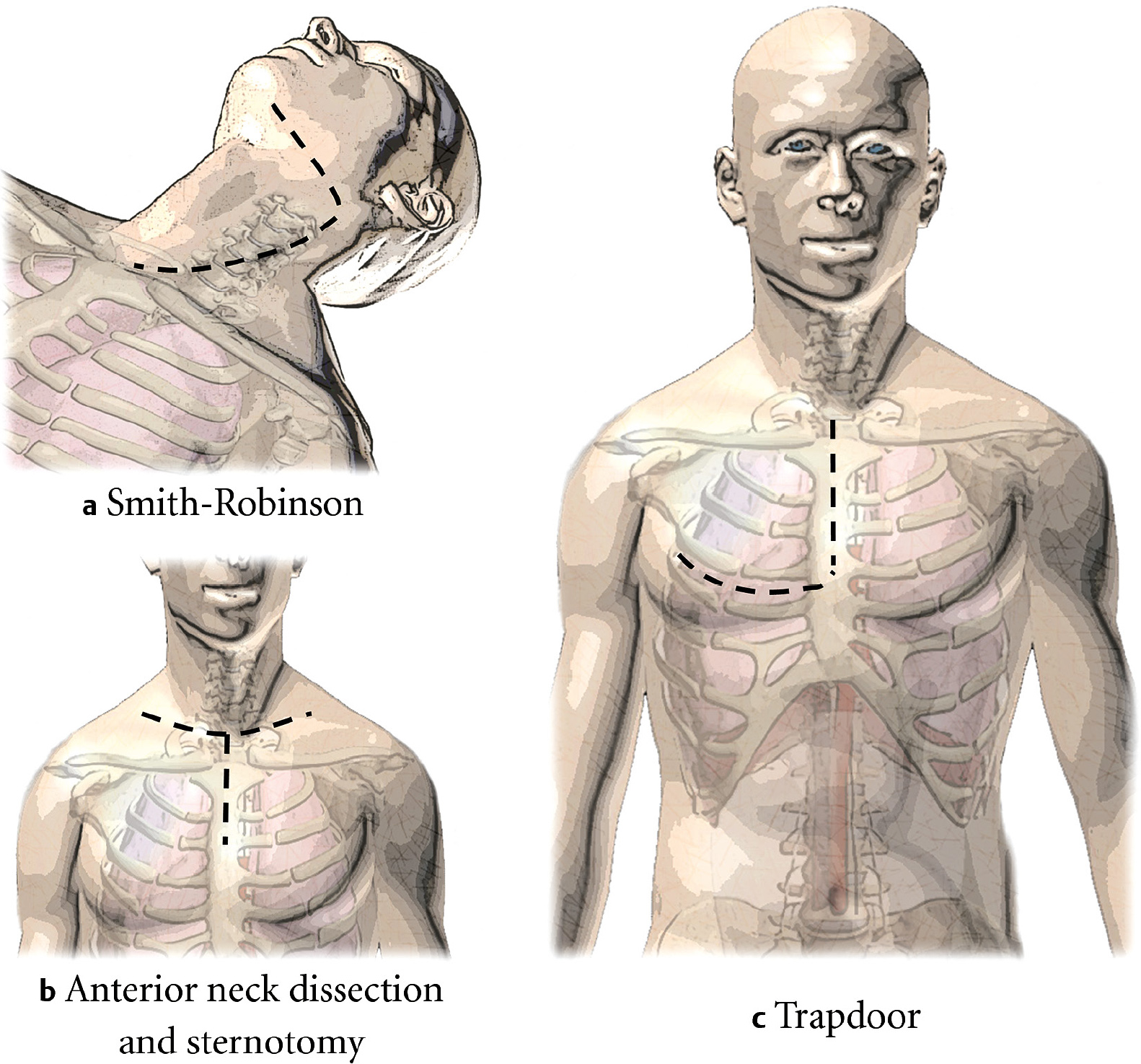
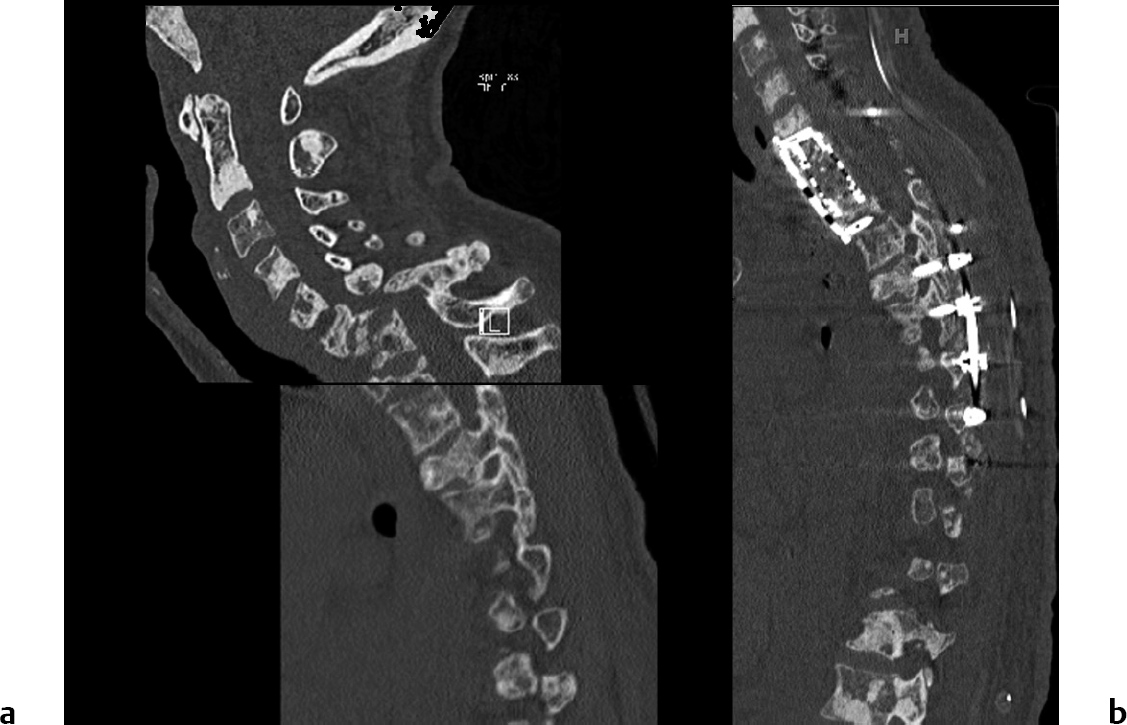
5 The spine is the third most common location of secondary metastases, after the lung and liver, occurring in up to one third of all metastatic cancer patients.1 Further, in a review of autopsy studies, it was reported that up to 70% of cancer patients had evidence of metastatic disease in the spinal column at the time of death.2 Anatomically, an overwhelming majority of spinal metastases originate from the vertebral body rather than from the posterior elements.3 Patients with symptomatic spinal metastases most commonly present with pain or neurologic dysfunction. A systemic workup with a computed tomography (CT) scan of the chest, abdomen, and pelvis for cancer staging may be necessary to guide surgical decision making, and in patients without a known primary tumor, a fine-needle biopsy under CT guidance should be performed. Patients with metastatic epidural spinal cord compression should be given high-dose dexamethasone, and in patients who respond to this therapy, radiation will likely provide relief.4 Tumor pathology dictates the appropriateness of adjuvant therapy, as radiosensitive tumors such as small-cell lung carcinoma, lymphoma, and multiple myeloma rarely require open decompression, as radiation alone provides effective palliation for patients at the end of life. Intermediately radiosensitive tumors include breast and prostate cancer, whereas melanoma is relatively radioresistant. For highly vascularized tumors, such as renal carcinoma, a preoperative angiogram with embolization should be considered to reduce the risk of intraoperative tumor bleeding during resection.5 In all pathologies, surgery with radiation should be considered if the patient is expected to live for longer than 3 months.6 In the landmark randomized controlled clinical trial of radiation alone versus radiation with surgery, Patchell and colleagues7 found that patient survival increased and the use of morphine and corticosteroids decreased with radiation and surgery compared with surgery alone. Several scoring systems help to guide surgical decision making. The Tokuhashi score has been used to identify if an excision or palliative strategy should be offered.8 Treatment goals can be tailored to the patient’s visceral and bony disease burden and grade of the malignancy as proposed in the Tomita score.9 The Spinal Instability Neoplastic Score (SINS) was proposed by the Spine Oncology Study Group (SOSG) to incorporate multiple variables to determine the stability, pending instability or gross instability caused by a primary or metastatic lesion in the spine.10 Complex approaches requiring prolonged recovery times are contraindicated if the life expectancy of the patient does not exceed 3 months, and radiation therapy may be offered for palliative treatment of pain.6 For patients with widespread metastases in the spinal column, direct decompressive surgery (i.e., laminectomy) with adjuvant radiotherapy improves neurologic outcomes and reduces the need for steroids and opioid analgesics.7 It should also be taken into account that surgical intervention delays radiation treatment due to the additional time needed for wound healing. En bloc resection for metastatic disease has been debated in the literature. Oncological cure is unlikely for metastatic disease, as widespread microscopic tumor foci are likely present; however, patients may survive many years beyond surgery. In a systemic review of the literature, Cloyd and colleagues11 found 5-year survival rates of 37.5% for patients undergoing en bloc spondylectomy for metastatic cancer in the spinal column. Aside from the technical demand of the surgery, the major risks of en bloc resection include nerve damage, excessive bleeding, spinal cord ischemia or stroke, and tumor spillage with disruption of the capsule or intralesional curettage. When planning en bloc resection, the patient must be consulted to determine his or her preferences and goals of care. This chapter reviews the approaches used for surgical resection of metastatic tumors in specific regions of the spine (Fig. 5.1), and describes patient positioning and approaches as well as the common complications associated with each surgical intervention. Complications are summarized in Table 5.1. The cervical spine comprises only 10 to 20% of metastatic spine disease cases; however, instability due to cervical metastases can lead to profound morbidity.12 More than 90% of patients with metastatic disease in the cervical spine present with nonmechanical neck pain as their chief complaint.13 Patients may also report referred pain in the shoulders. Biomechanically, in the subaxial spine, lytic invasion of metastatic tumor in the cancellous bone of the vertebral body increases the risk of collapse and subsequent loss of lordosis. At the atlanto-axial level, involvement of the C1 lateral mass leads to pain on rotational head movements. Stability of the atlantoaxial ligamentous complex, particularly the transverse ligament, determines the stability of the C1/C2 vertebral bodies. The wider spinal canal in the atlanto-axial spine reduces the risk of metastatic epidural spinal cord compression, and as a result anterior atlantoaxial subluxation is a more common cause of canal stenosis at this level.14 Lateral flexion-extension radiographs of the spine can help identify the degree of spondylolisthesis and ultimately identify regions of instability in the cervical spine. When assessing a patient with a cervical metastasis, take a thorough history and perform a physical examination to confirm the patient’s chief complaint. Cervical myelopathy, characterized by weakness in the hands and relative preservation of lower extremity function, may be the result of degenerative disease in the cervical spine unrelated to the metastatic process. Although vertebral body involvement from a metastatic lesion may be the most radiographically impressive element of the patient’s imaging, it may not be the sole cause of the neurologic impairment. Loss of cervical lordosis, degenerative disk disease with multilevel stenosis, or congenital stenosis may be the main cause of a patient’s symptoms and should be considered when planning surgery. In patients with a loss of lordosis, posterior reduction and fixation alone will not restore anatomic alignment, and an anterior approach is recommended. Posterior laminectomy or hemilaminectomy with instrumented fixation is frequently used for patients with preserved cervical lordosis suffering from metastatic disease in the cervical spine. Although the posterior elements are rarely involved in metastatic cervical tumors, decompressive laminectomy or foraminotomy are less invasive surgical procedures to provide relief of myelopathy or cervical radiculopathy. Instrumented fusion reduces the pain associated with subluxation and instability. Bone quality should also be taken into consideration in order to assess the patient’s risk of instrumentation failure, and cement can be used to reinforce screw purchase. Fig. 5.1 Schematic depicting region-specific approaches to the spine for resection of metastatic tumors. Approaches between regions are effective for cross-junctional access. Black dashed arrows demonstrate approaches commonly used at multiple regions. The patient is placed prone on the operating table with the head in a Mayfield fixator. A midline incision is made to provide adequate exposure of the level of interest. The paraspinal musculature is divided, and subperiosteal dissection facilitates direct visualization of the lamina. Although the C1 and C2 nerve roots can be sacrificed safely, subsequent nerve root damage to C3-C7 results in significant patient morbidity and should always be considered when weighing treatment options. Lateral mass screws may be used from C3 to C6, along with a fitted rod to mimic natural cervical lordosis. Intractable subluxations can warrant the placement of occipitocervical fusion (OCF) hardware, which requires a more extensive exposure and is beyond the scope of this chapter. One of the primary risks associated with surgical intervention in the cervical spine is vertebral artery (VA) injury. Wright and Lauryssen14 found that 4.1% of a cohort of 1,318 patients receiving transarticular screws incurred VA injury. Patients with tumor in this region or a history of radiation to the area may have distorted anatomy or scar tissue, further increasing the risk of vertebral artery injury. As a result, a preoperative three-dimensional (3D) CT angiogram should be considered prior to placing instrumentation in the craniovertebral junction. If a VA is injured intraoperatively, recall that the lateral mass screw acts to tamponade the vessel. Avoid removing the screw in the VA and do not place the contralateral screw, as bilateral VA injury will lead to devastating neurologic consequences. Perform an angiography immediately, if possible, to assess if endovascular repair via balloon occlusion, coil embolization, or stent deployment is feasible and to assess the patency of the contralateral VA. The transoral approach allows visualization of the anterior aspect of C1-C3 with 15 to 20 mm of lateral exposure from the midline.15 It is uncommonly performed in metastatic tumor patients, yet may be indicated for patients with significant anterior compression of the spinal cord involving the upper cervical vertebrae. For this approach, the patient is positioned supine with the neck in 10 to 15 degrees of extension in a three-point Mayfield headholder. Intra-operative fluoroscopy with a C-arm is recommended for localization. A preoperative lateral radiograph of the hyperextended neck is recommended to evaluate instability at the craniocervical junction that may be aggravated with patient positioning. Preoperative and intraoperative antibiotics should be given to cover anaerobes and oral flora. Intubation via an awake fiberoptic endotracheal intubation may be used or tracheostomy to provide ventilation without disrupting the operative field. If necessary, the soft palate can be split at the midline to increase the operative field. Although greater extension of the surgical field is possible via maxillary osteotomy or mandibulotomy approaches, they should be used with extreme caution in metastatic tumor patients due to prolonged patient recovery times and the high risk of complications. Posterior fixation is highly recommended following the transoral approach due to an increase in mechanical instability caused by the possible disruption of the alar, transverse, and anterior longitudinal ligaments.16 As a result, treatment of the atlantoaxial spine often results in OCF; however, if the occipitoaxial joint remains stable, a limited C1-C2 fixation should be considered to preserve motion.17 The most common complications associated with the transoral approach include injury to the hypoglossal and lingual nerves with subsequent speech and swallowing difficulties. A nasogastric tube may be placed intraoperatively, or a percutaneous endoscopic gastrostomy (PEG) may be placed to provide adequate nutrition for the patient in the immediate postoperative period. As with most spinal surgeries, cerebrospinal fluid (CSF) leak secondary to incidental durotomy can lead to devastating complications and should be managed with a direct repair when possible, or a CSF diverting lumbar drain or shunt as necessary. Patients with CSF leak may complain of headaches, and are at risk of meningitis.16 The splitting of the soft palate is also known to cause velopalatine incompetence, or the inability to completely close the soft palate resulting in nasal regurgitation of liquids during swallowing.18 First described by Smith and Robinson,19 the anterolateral approach to the cervical spine enables anterior access to C3-T1. On the right side, the recurrent laryngeal nerve crosses medially at C6/C7, thus a left-sided approach is recommended at this level. For this approach, the head of the bead is elevated 30 degrees and the patient is positioned supine with the head fixed in a Mayfield clamp and rotated away from the incision, with a towel placed transversely under the scapula to allow for neck extension. The head is rotated about 15 degrees to the contralateral side. Nasotracheal intubation allows complete closure of the mandible and improves the exposure. A 3- to 5-cm incision is made along the midline to the posterior sternocleidomastoid for adequate exposure of two or three disk levels corresponding to the relevant pathology (Fig. 5.2a). The platysma is then divided at the anterior border of the sternocleidomastoid. Deep dissection proceeds with division of the pretracheal fascia to open the plane between the carotid sheath and the trachea and esophagus. Care should be taken to ensure the protection of the trachea, esophagus, and recurrent laryngeal nerve during dissection. Once adequate exposure is obtained, anterior corpectomy and resection can be performed followed by the placement of a cage with allograft and anterior plate fixation. Concomitant posterior fixation is required for multilevel anterior corpectomy performed at three or more vertebral levels in order to ensure adequate construct stabilization. Traction may be used if the patient has a severe kyphotic deformity in the cervical spine or if subluxation is present. Fig. 5.2a–c Surgical markings for various approaches. (a) A “hockey stick” incision for the anterolateral (Smith-Robinson) approach to the subaxial cervical spine. (b) Anterior neck dissection and sternotomy approach with a T-shaped incision. (c) The trapdoor approach, which extends into the fourth interspace, allowing for retraction of the chest wall. The anterolateral approach to the subaxial cervical spine represents a relatively atraumatic spinal dissection with a generous exposure allowing for access to a wide range of spinal pathologies. An intraoperative tracheostomy, PEG, or nasogastric (NG) tube may be placed, as postoperative edema can compress the airway and esophagus. Additional care should be given for patients who previously received radiation treatments because scarring and tissue deterioration can significantly increase the risk of complications. Esophageal erosion from anterior plate hardware is a rare but serious complication with a reported incidence of 1.49%, and the patient should be monitored long term for any symptoms of instrumentation failure.20 Metastatic tumors in the thoracic region represent 70% of metastatic disease in the spine.3 One of the primary anatomic advantages for surgical resection of tumors in the thoracic region is that, if necessary, nerve roots can be easily ligated without severe functional deficit. In addition, the thoracic spine is more stable than other spinal regions because it is mechanically reinforced by the ribs and sternum. First described by Rosen et al,21 this approach provides the most direct access to the cervicothoracic junction (as high as C4) and to the superior aspect of the T3 vertebral body. The patient is positioned supine with towels under the scapula to extend the neck slightly. A T-shaped incision is made 1 cm above the clavicle with a vertically oriented medial incision over the sternum (Fig. 5.2b). Once exposure is established, a rectangular block of sternum is resected along with about one third of the clavicle on the operative side. Although entry from the left is preferred due to the risk of injury to the right recurrent laryngeal nerve, the approach should also be dictated by the side with the greatest extravertebral tumor extension. Instrumentation following low cervical/high thoracic vertebrectomy that does not extend across the cervicothoracic transition zone will often lead to a higher incidence of adjacent level degeneration due to added mechanical stress. As a result, this approach facilitates good visualization and proper screw and plate placement across the cervicothoracic junction. The presence of an anterolateral soft tissue mass is viewed as a contraindication for such an approach due to the already limited operative space available. Considering the relatively small operative field and the anatomic complexity of the upper thoracic cavity, this approach presents a challenge to most spinal surgeons. Patients must be made aware of the possibility of an intraoperative tracheostomy and gastrostomy, pulmonary injury, the risks of recurrent laryngeal nerve palsy, and the potential for damage to the great vessels.22 A 39-year-old woman presented with breast cancer with diffuse skeletal and spinal metastases despite chemotherapy (Fig. 5.3a). The lytic nature of the lesions at C6 and C7 resulted in vertebra plana, with complete loss of the vertebral body height. She developed paraplegia, and underwent radiation therapy and external immobilization and recovered the ability to ambulate with some assistance. A staged surgical procedure was offered. The patient underwent preoperative reduction with 35 pounds of traction with gradual correction of her deformity. The first stage of the surgery included a left anterior cervical approach and median sternotomy to gain access to the left cervicothoracic junction. The anterior corpectomy was performed through an aortocaval window above the pulmonary artery and below the innominate vein. The vertebral bodies of C6-T1 were removed using a high-speed diamond bur. Decompression of the C6-T1 nerve roots was also performed. An anterior cage and plate were placed extending from C5 to T2. Four days later, a C5-T1 bilateral total laminectomy and a C2-T8 posterior fixation completed the second stage of the procedure (Fig. 5.3b). Her clinical course was complicated by facial edema, bilateral pleural effusions, and hospital-acquired pneumonia. She was discharged to rehabilitation and survived 3½ years after surgery. Fig. 5.3a,b Metastatic lesion at the cervicothoracic junction. (a) Composite cervical and thoracic preoperative computed tomography (CT) scan from a patient with metastatic breast cancer in the cervicothoracic junction demonstrating vertebra plana of C6-C7 with focal kyphosis and grade 4 anterolisthesis. Intraoperatively, the vertebral bodies of C6-T1 were removed using a high-speed diamond bur. (b) An anterior cage and plate were placed extending from C5-T2. Four days later, C5-T1 bilateral laminectomy and C2-T8 posterior fixation completed the second stage of the procedure.
Region-Specific Approaches
 Introduction
Introduction
 Cervical Spine
Cervical Spine
Posterior Approach
Transoral Approach
Smith Robinson/Anterolateral Approach
 Thoracic Spine
Thoracic Spine
Anterior Neck Dissection and Sternotomy
Case Illustration
Region-Specific Approaches
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree