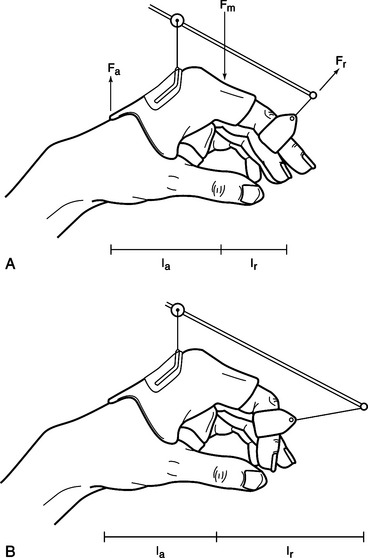
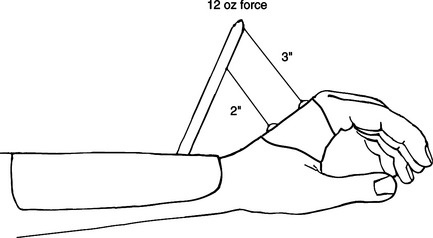
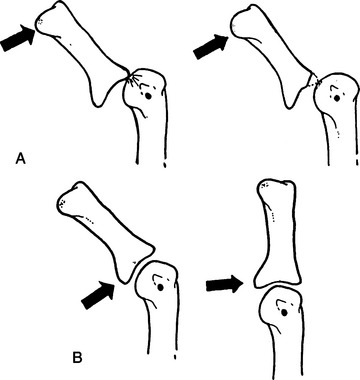
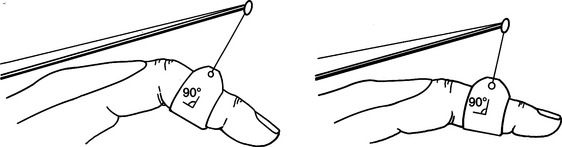
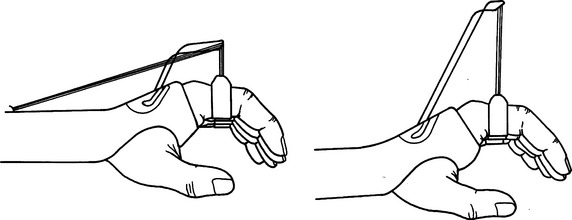
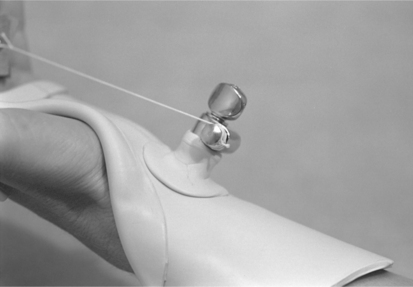
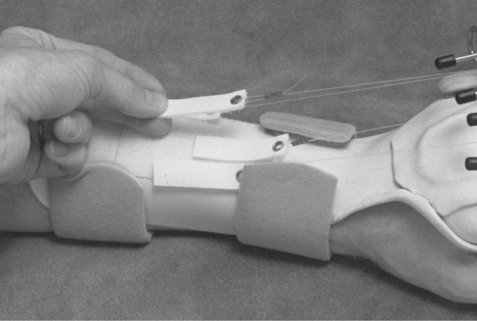
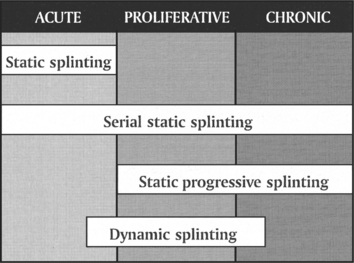
CHAPTER 11 1 Understand the biomechanics of dynamic splinting. 2 Identify effects of force on soft tissue. 3 Understand the way to apply appropriate tension. 4 Identify common uses of dynamic splinting. 5 List the goals of dynamic splinting. 6 List the materials necessary for fabrication of a dynamic splint. 7 Explain the risks of applying dynamic force. 8 Identify contraindications for application of a dynamic splint. 9 Understand the fabrication steps of three dynamic splints. 10 Identify instances in which dynamic splinting is appropriate. Mobilization splints or dynamic splints have movable parts and are designed to apply force across joints [Brand 2002]. Mobilization splints use constant or adjustable tension, or both, to achieve one of the following goals [Fess 2002]: • Substitute for loss of muscle function • Correct deformities caused by muscle-tendon tightness or joint contractures • Maintain active or passive range of motion • Provide controlled motion after tendon repair or joint arthroplasty There are many implications for the use of dynamic splinting that become more familiar to the therapist with increased exposure to various hand injuries. Some specific indications for the use of dynamic splints are presented in this chapter. However, it is important to note that the therapist must first understand the person’s injury, surgical procedures, and physician’s protocol for treatment. If any of these conditions are in question, the therapist should seek clarification prior to splinting. Whether the person has a peripheral nerve injury, spinal cord injury, or other debilitating disease, a splint can increase the functional use of a hand. The goals of splinting for loss of muscle function are to substitute for loss of motor use, prevent overstretching of nonfunctioning muscles, and prevent joint deformity. Both dynamic and static splints can accomplish these goals [Fess et al. 2005]. A common peripheral nerve injury is high radial nerve palsy. A hand with radial nerve damage has limited functional use due to the inability to extend the wrist and metacarpophalangeal (MCP) joints, and because of the lack of palmar abduction and radial abduction of the thumb. A splint that provides passive assistance to the wrist and MCP joints in extension while allowing active composite flexion of the fingers will greatly increase the functional use of the hand (see also Chapter 13,Figure 13-8). Another example of substitution for loss of motor function involves persons with spinal cord injuries. A person who has a C7 lesion may also benefit from dynamic splinting. The person’s active wrist extension will become the force to transmit motion for finger flexion in a tenodesis splint (Figure 11-1). Finally, persons who have debilitating diseases such as amyotrophic lateral sclerosis, Guillain-Barrè syndrome, or other neurologic disorders may benefit from specialized dynamic splints. However, the presence of spasticity might preclude candidates for dynamic splinting (see Chapter 14). Limited passive joint range of motion might be a result of multiple factors, including prolonged immobilization, trauma, or significant scar formation. A person who exhibits limited passive joint motion may be a candidate for a dynamic splint. However, if a large discrepancy exists between active and passive joint motion the goal of treatment should focus on active range of motion and strengthening prior to splinting. If active range of motion and passive range of motion are similar, greater active motion can be gained through mobilization splinting [Colditz 2002a]. The best results from dynamic splinting are attained when the therapist initiates treatment soon after edema and pain are under control. As mentioned previously in this text, the best way to lengthen tissue is to provide a tolerable force over a long period of time. Research indicates a direct correlation between the length of time a stiff joint is held at its end range and the resulting gain achieved with passive joint motion [Flowers and LaStayo 1994]. The focus of dynamic splinting should be on increasing the length of time the splint is worn rather than increasing the force. However, certain conditions (such as dense ligaments or scar tissue) generally always require a greater amount of force to achieve tissue remodeling. Application of external force necessitates careful attention to the distribution of pressures over the skin surface because the skin is always the weak link in the system. A general goal for a mobilization splint is to increase passive joint range of motion by 10 degrees per week [Brand 2002]. Should passive range of motion not improve following two weeks of splinting, the splinting and treatment program should be reevaluated [Fess and McCollum 1998]. Therapists use dynamic splinting to control motion after the completion of joint implant arthroplasty and flexor tendon repairs. Because of the altered joint mechanics of a person who has arthritis and undergoes joint replacement surgery, the dynamic splint has multiple functions. First, dynamic splints provide controlled motion and precise alignment of the repaired soft tissue while minimizing soft-tissue deformity. For example, after joint replacement the splint may provide forces on one finger in both extension and radial deviation. Second, the splint maintains alignment of the joints for the healing structures while allowing guarded movement of the joint [Fess et al. 2005]. After flexor tendon repairs, the therapist uses a dynamic splint to provide controlled motion to the healing structures. The reasons for controlled motion are threefold. First, moving the tendons increases the flow of nutrient-rich synovial fluid to enhance healing. Second, tendons allowed early mobilization have demonstrated increased tensile strength compared to immobile tendons. Third, by allowing 3 to 5 mm of tendon excursion adhesion formation between tendons and surrounding structures is minimized [Stewart and van Strien 2002]. Dynamic traction should be used for the treatment of selected intra-articular fractures of the finger [Hardy 2004]. A dynamic traction splint involves the use of static tension while allowing joint movement. Traction provides tension to the ligaments, which incorporates the use of ligamentotaxis to bring boney fragments back into anatomic alignment. With constant traction applied throughout the range of motion, the splint allows the fracture to heal while maintaining adequate glide of surrounding soft tissues. Mobilization splints may also be used following a severe burn to assist in wound healing. The use of such splinting during wound healing will facilitate proper collagen alignment and scar formation. Soft-tissue structures respond to prolonged stress by changing or reforming. This activity is called creep and results from the application of prolonged force [Brand and Hollister 1993b]. Soft tissue responds to excessive force with increased pain and a reintroduction of the inflammatory process [Fess and McCollum 1998]. By applying controlled stress to the tissue over a prolonged period of time, the therapist can create tension gentle enough to allow creep without tissue injury. Provided it remains within elastic limits, the stress from a mobilization splint can positively affect the gradual realignment of collagen fibers (resulting in increased tensile strength of the tissue) without causing microscopic tearing of the tissue. The ability to alter collagen formation is greatest during the proliferative stage of wound healing but continues to a lesser degree for several months during scar maturation [Colditz 2002]. To provide the greatest benefit from a mobilizing splint, the therapist must understand relevant theories of physics. Mechanical advantage involves the consideration of various forces applied by the splint base and the dynamic portion of the splint. As seen inFigure 11-2, Fa refers to the applied force and Fr refers to the resistance force. Fm is determined by the sum of the opposing forces (Fa+ Fr) [Fess 1995]. Mechanical advantage is defined as [Brand 2002]: By adjusting the length of the splint base or the length of the outrigger, the mechanical advantage can be altered (Figure 11-2) [Smith et al. 1996]. The goal of a splint is to maintain a mechanical advantage of between 2/1 and 5/1, meaning that the lever arm of the applied force is at least twice as long as the lever arm of the applied resistance [Brand 2002]. A splint with a greater mechanical advantage will be more comfortable and durable [Fess 1995]. A mobilizing MCP flexion splint that is forearm and hand based rather than just hand based will disperse pressures in addition to providing a greater mechanical advantage due to the longer lever areas of the applied force. Torque is defined as the effect of force on the rotational movement of a point [Fess et al. 2005]. The amount of torque is calculated by multiplying the applied force by the length of the moment arm (Figure 11-3). A correlation exists between the distance from a pivot point and the amount of force required. To achieve the same results, a force applied close to the pivot point (i.e., short moment arm) must be greater than the force applied on a longer moment arm. This force is called torque because it acts on the rotational movement of a joint. In practical terms, the therapist should place the force as far as possible from the mobilized joint without affecting other joints [Brand and Hollister 1993b]. A forearm-based dynamic wrist extension splint should be constructed so that its mobilizing force is on the most distal aspect of the palm, while not affecting MCP movement. An exception to placing the force as far from the mobilized joint as possible occurs when rheumatoid arthritis is involved. If the joint is unstable, a force applied too far from the joint will result in tilt rather than a gliding motion of the joint (Figure 11-4) [Hollister and Giurintano 1993]. Therefore, when splinting a hand with rheumatoid arthritis the force should be applied as close to the mobilizing joint as possible. In dynamic splinting, the therapist applies force to a joint or finger through the application of nail hooks, finger loops, or a palmar bar. When applying force to increase passive joint range of motion, the therapist must keep the direction of pull at a 90-degree angle to the axis of the joint and perpendicular to the axes of rotation [Cannon et al. 1985]. As range of motion increases, the therapist must adjust the outrigger to maintain the 90-degree angle (Figure 11-5) [Fess et al. 2005]. The outrigger should not pull the finger or hand toward ulnar or radial deviation. When excessive force is applied to the skin for a prolonged period, tissue damage can result. The amount of pressure the skin can tolerate dictates the maximum tolerable force. As a general rule, the amount of acceptable pressure or force per unit area is 50 g/cm2 [Brand and Hollister 1993a]. As the area over which force is applied becomes larger, the pressure per unit area becomes less. A leather sling with a skin contact area on a finger of approximately 4 cm2 should provide a maximum pressure of 200 g [Fess at al. 2005]. A smaller sling with less skin contact area concentrates the pressure and is less tolerable. Two features unique to mobilization splinting are the use of an outrigger and the application of force. The outrigger is a projection from the splint base the therapist uses to position a mobilizing force. The outrigger material depends on the amount and position of the desired force. If the outrigger and attachment to the base are not secure, the direction of the mobilizing force may change—reducing the effectiveness of the splint [Colditz 1983]. An outrigger can be a high or low profile (Figure 11-6). Each type has advantages and disadvantages. With a significant change in range of motion, the high-profile outrigger will result in slightly less deviation from the 90-degree angle of pull than the low-profile outrigger. Clients should be seen in the clinic frequently enough that increases in range of motion can be accommodated by regular adjustments to the outrigger, thus maintaining the 90-degree angle of pull [Austin et al. 2004]. It should be noted that a high-profile outrigger, on the other hand, is bulky and may decrease the person’s compliance with wearing the splint. A low-profile outrigger requires adjustments more frequently but is more aesthetically pleasing and less cumbersome. A therapist can form an outrigger from The therapist can use various methods for applying dynamic force to a joint. Finger loops from strong pliable material are usually best because of the increased conformability to the shape of the finger [Fess et al. 2005]. The therapist can supply force by using rubber bands, springs, or elastic thread. Although rubber bands are more readily available and easy to adjust, springs offer more consistent tension throughout the range. A long rubber band stretched over the maximum length of the splint provides more constant tension than a short rubber band [Brand and Hollister 1993a]. Elastic thread is the easiest to apply and adjust. A nonstretchable string or outrigger line is necessary to connect the finger loop to the source of the force (Figure 11-7). The choice is usually based on clinical experience and preference. Figure 11-7 The therapist uses nonstretchable nylon string to attach finger loops to the source of tension. Another method of applying force is through static progressive tension. Rather than providing the variable tension of a dynamic splint, a static tension splint uses nonelastic tension to provide a constant force. An advantage of properly applied static tension is that tissue is not stretched beyond the elastic limit [Schultz-Johnson 2002]. In place of the rubber band or spring (as used on a dynamic tension splint) the therapist may use a Velcro tab, turnbuckle, or commercially available static progressive components to apply the force (Figure 11-8). Tension is increased by gradually moving the Velcro tab more proximally on the splint base or adjusting the turnbuckle. The force is static rather than dynamic but is readily adjustable by the person throughout the wearing time (Figure 11-9). Because the person has control over the amount of applied tension, the static progressive splint is more tolerable to wear than a dynamic tension splint [Schultz-Johnson 2002]. In determining whether to apply dynamic or static tension, the therapist must identify the “end feel” of a joint. End feel is assessed by passively moving a joint to its maximal end range. A joint with a soft or springy end feel indicates immature scar tissue. A joint with a hard end feel indicates a more mature scar tissue or long-standing contracture. A splint with static or dynamic tension is appropriate for a joint with a soft end feel, whereas a joint with a hard end feel will respond only to static tension. Regardless of the end feel, static tension will increase passive range of motion faster than dynamic tension for any joint [Schultz-Johnson 1996]. Another determinant in selecting the type of tension to be used with mobilization splinting is the stage of tissue healing. As seen inFigure 11-10, different types of splints are more appropriate at various stages of healing. The acute stage is primarily characterized as the initial inflammatory stage. The proliferative stage occurs after the initial inflammation subsides and tissues are in the early stages of reorganization. The chronic stage is attained when the cells have realigned and the joint response to stress is a hard end feel [Colditz 1995].
Mobilization Splints: Dynamic, Serial-Static, and Static Progressive Splinting
Implications of Mobilization Splints
Substitution for Loss of Motor Function
Correction of a Joint Deformity
Provision of Controlled Motion
Aid in Fracture Alignment and Wound Healing
Biomechanics of Dynamic Splinting
Torque and Mechanical Advantage
Application of Force
Features of a Mobilization Splint
 -inch wire rod. This diameter is thick enough to provide stability yet pliable enough to manipulate with pliers. Construction of an outrigger using a wire rod requires precise shaping, a skill that necessitates practice. Commercial adjustable wire outrigger kits are also available. Although the use of a commercial kit may increase the material cost of the splint, the application of the adjustable components is easier and may thus reduce splintmaking time. The therapist should bear in mind that charges for fabrication time are the most costly part of the splint.
-inch wire rod. This diameter is thick enough to provide stability yet pliable enough to manipulate with pliers. Construction of an outrigger using a wire rod requires precise shaping, a skill that necessitates practice. Commercial adjustable wire outrigger kits are also available. Although the use of a commercial kit may increase the material cost of the splint, the application of the adjustable components is easier and may thus reduce splintmaking time. The therapist should bear in mind that charges for fabrication time are the most costly part of the splint.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine